The diagnosis of pigmented actinic keratosis (PAK) is often challenging because of overlapping features with lentigo maligna.
ObjectiveTo investigate dermoscopic patterns of PAK according to their different evolutionary stages, and to correlate the pattern with clinical characteristics of the patients.
MethodsDescriptive and analytical study of 232 PAK. Dermoscopic patterns were divided into two categories: the follicule surroundings tm) abnormalities (FSA) and follicular keratosis tm) abnormalities (FKA).
ResultsFSA and FKA dermoscopic patterns were related to male gender, except for star-like appearance, double white clods and dermoscopic horn (p≤0.04). Rhomboidal, annular granular pattern, gray halo, white circle and double clods were dermoscopic pattern significantly related to xeroderma pigmentosum's type of skin. Based on the evolutionary stages of PAK, the jelly sign was significantly related to thin patches of PAK. Central crusts and scales were related to thick plaques and the star-like appearance to hypertrophic PAK. The presence of 2 or more dermoscopic signs in both FSA and FKA was noticed in 99.1% of lesions.
ConclusionsThe dermoscopic diagnosis of PAK vary according to the evolutionary stages of the disease, this will increase the diagnosis accuracy, with therapeutic implications.
El diagnóstico de la queratosis actínica pigmentada (QAP) es a menudo difícil, debido a sus características, que se solapan con las propias del lentigo maligno.
ObjetivoInvestigar los patrones dermatoscópicos de la QAP con arreglo a sus distintos estadios evolutivos, y correlacionar dicho patrón con las características clínicas de los pacientes.
Mèc)todosEstudio descriptivo y analítico de 232 QAP. Se dividieron los patrones dermatoscópicos en 2 categorías; alteraciones perifoliculares (APF) y la queratosis folicular (QF).
ResultadosSe relacionaron los patrones dermatoscópicos de APF y QF con el sexo masculino, exceptuando las características de aspecto estrellado, double white clods y cuerno dermatoscópico (p≤0,04). Las características romboidal, anular-granular, de halo gris, círculo blanco y double clots constituyeron los patrones dermatoscópicos significativos relacionados con el tipo de piel del xeroderma pigmentoso. Sobre la base de los estadios evolutivos de la QAP, el signo de la jalea guardó relación significativa con los parches finos cutáneos de la QAP. Las costras y escamas centrales se relacionaron con las placas densas, y el aspecto estrellado de la QAP hipertrófica. La presencia de 2 o más signos dermatoscópicos, tanto en APF como en QF, se apreció en el 99,1% de las lesiones.
ConclusionesEl diagnóstico dermatoscópico de QAP varía con arreglo a los estadios evolutivos de la enfermedad, incrementándose la precisión diagnóstica, con implicaciones terapèc)uticas.
Actinic keratosis is considered to be an in situ epidermal dysplasia that develops in sunexposed areas in individuals having a fair skin phototype.1 It may be erythematous or pigmented; pigmented AK (PAK) is a challenging lesion also on dermoscopic examination, especially on the face, since it can be easily misdiagnosed as lentigo maligna (LM).2 Whereas LM should be excised, PAK can be treated with less invasive approaches and excellent esthetic results.3,4 A biopsy is often required to achieve a correct diagnosis, leading to unnecessary scars on a cosmetically sensitive area. The primary objective of the present study was to describe the dermoscopic patterns of PAK according to their different evolutionary stages, and to correlate the pattern with clinical characteristics of the patients in order to emphasize the usefulness of this imaging technique in the diagnosis of PAK.
Materials and methodsDescriptive and analytical study conducted in the Department of Dermatology of the University Hospital Hassan II of Fez in Morocco and extending over a period of 10 months (October 2014•July 2015).
The age, sex, skin phototype, and site of the lesions were recorded for each patient. The evolutionary stages of PAK were determined as follows: thin patches with thin or without scales; scaly plaque and hyperkeratotic plaque. Clinical and dermoscopic images were taken and then evaluated by three examiners experienced in dermoscopy independently of the histology results if the lesion was excised; and then the correlation dermoscopy-histopathology was done after the dermoscopic analysis.
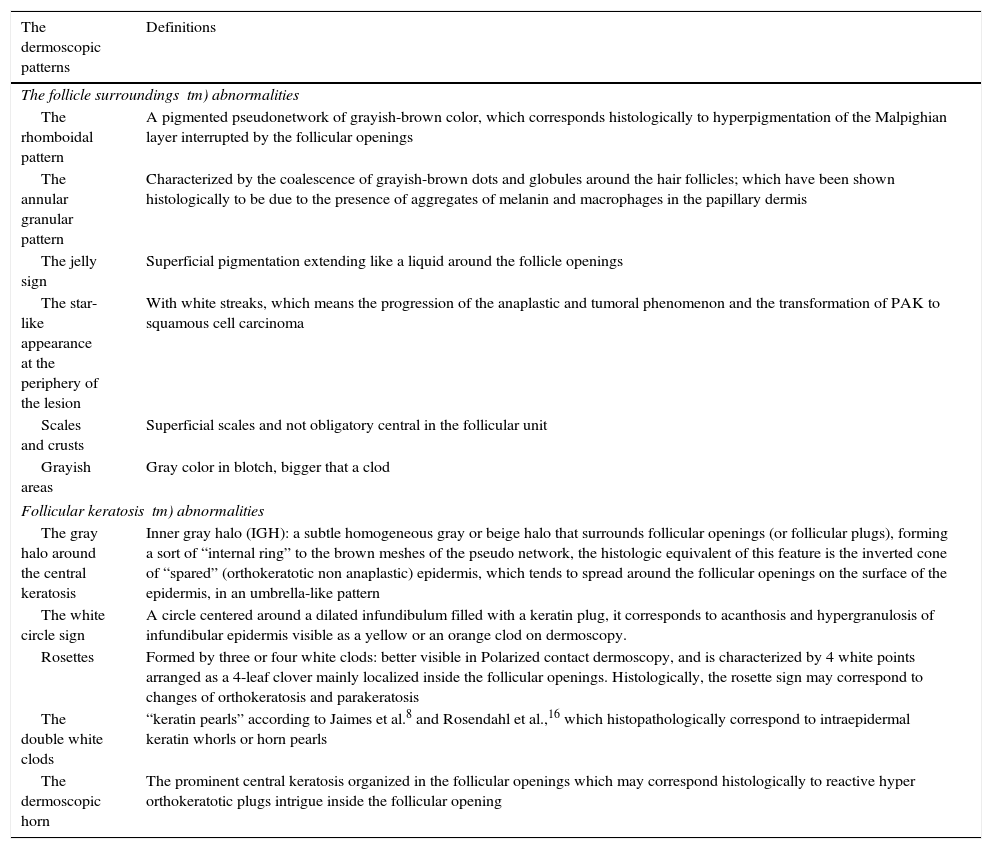
Dermoscopic patterns were divided into two categories. The follicle surroundings tm) abnormalities (FSA) which included: rhomboidal pattern, annular granular pattern, the jelly sign and the star-like appearance at the periphery of the lesion. Follicular keratosis tm) abnormalities (FKA) included: the gray halo around the central keratosis, the white circle sign, rosettes, double white clods, one white clod and the dermoscopic horn (Table 1).
Classification and definitions of the dermoscopic patterns examined in our study.
| The dermoscopic patterns | Definitions |
|---|---|
| The follicle surroundings tm) abnormalities | |
| The rhomboidal pattern | A pigmented pseudonetwork of grayish-brown color, which corresponds histologically to hyperpigmentation of the Malpighian layer interrupted by the follicular openings |
| The annular granular pattern | Characterized by the coalescence of grayish-brown dots and globules around the hair follicles; which have been shown histologically to be due to the presence of aggregates of melanin and macrophages in the papillary dermis |
| The jelly sign | Superficial pigmentation extending like a liquid around the follicle openings |
| The star-like appearance at the periphery of the lesion | With white streaks, which means the progression of the anaplastic and tumoral phenomenon and the transformation of PAK to squamous cell carcinoma |
| Scales and crusts | Superficial scales and not obligatory central in the follicular unit |
| Grayish areas | Gray color in blotch, bigger that a clod |
| Follicular keratosis tm) abnormalities | |
| The gray halo around the central keratosis | Inner gray halo (IGH): a subtle homogeneous gray or beige halo that surrounds follicular openings (or follicular plugs), forming a sort of “internal ring” to the brown meshes of the pseudo network, the histologic equivalent of this feature is the inverted cone of “spared” (orthokeratotic non anaplastic) epidermis, which tends to spread around the follicular openings on the surface of the epidermis, in an umbrella-like pattern |
| The white circle sign | A circle centered around a dilated infundibulum filled with a keratin plug, it corresponds to acanthosis and hypergranulosis of infundibular epidermis visible as a yellow or an orange clod on dermoscopy. |
| Rosettes | Formed by three or four white clods: better visible in Polarized contact dermoscopy, and is characterized by 4 white points arranged as a 4-leaf clover mainly localized inside the follicular openings. Histologically, the rosette sign may correspond to changes of orthokeratosis and parakeratosis |
| The double white clods | “keratin pearls” according to Jaimes et al.8 and Rosendahl et al.,16 which histopathologically correspond to intraepidermal keratin whorls or horn pearls |
| The dermoscopic horn | The prominent central keratosis organized in the follicular openings which may correspond histologically to reactive hyper orthokeratotic plugs intrigue inside the follicular opening |
Newly described dermoscopic signs were used in our study, namely, the prominent central hyperkeratosis and the double white clod. The prominent central hyperkeratosis in the follicular opening gives an appearance of a dermoscopic horn. This sign is the evolution of the central keratin surrounded by the inner gray halo described by Nascimento et al.5 The second newly described sign in this study was the double white clods attached against each other. Other signs such as the rosette sign,6,7 the jelly sign1 with a superficial pigmentation appearance, white globules and circles7 and the inner gray halo (IGH)5 around the yellowish keratin were examined based on recent literature. In addition, other known signs, such as rhomboidal structures, globules and dots, annular•granular pattern and scales8,9 were also examined.
Statistical analysis was performed using the SPSS 20 software. Two kinds of analysis were performed, namely descriptive and univariate analysis. The descriptive analysis where quantitative variables were expressed as means±standard deviation and qualitative variables as percentages, and in the univariate analysis, the comparison of two percentages was carried out by Chi 2 test. A p value less than 0.05 was considered statistically significant.
Ethical approval was obtained from the ethics committees in the Department of Dermatology of the Hospital Center Hassan II in Fez-Morocco, and all the patients were informed of the conditions related to the study and gave their written, informed consent.
ResultsIn total, 232 lesions in 150 patients were included in our study. 52 lesions were confirmed clinically and 180 were confirmed histologically.
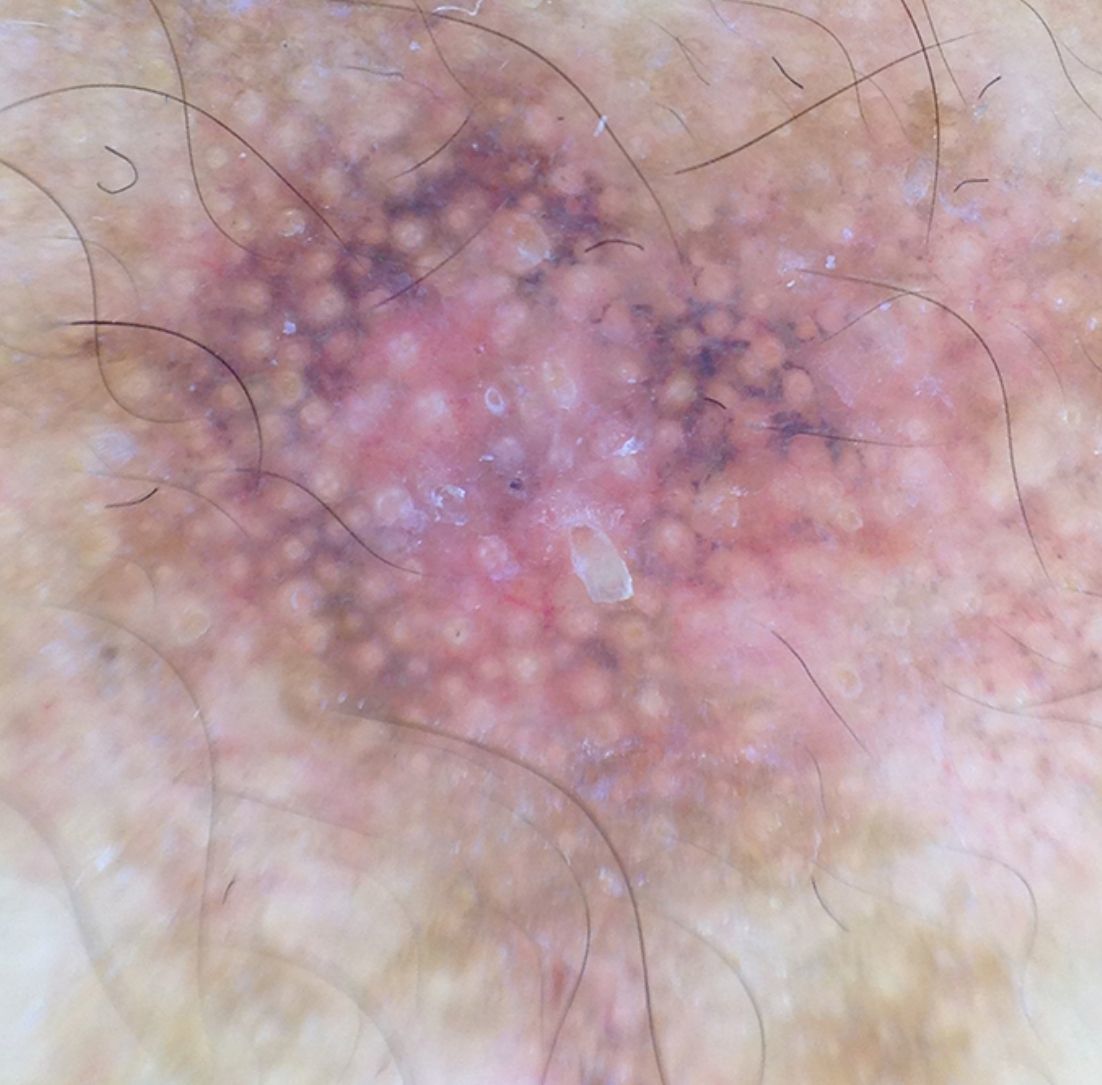
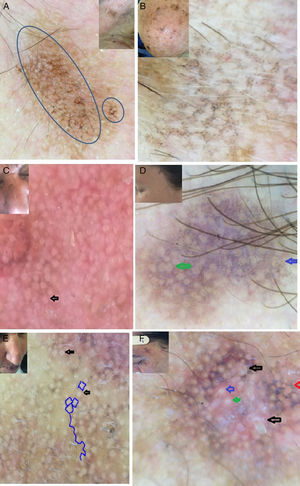
Patients tm) age ranged from 20 to 70 years (mean age 54.7 years old). The other epidemiological and clinical characteristics of lesions were summarized in Table 2 and the dermoscopic patterns described in our study were resumed in Table 3 (Figs. 1 and 2). The presence of 2 or more dermoscopic signs in both the follicule's surroundings and keratosis was noticed in 99.1% of lesions. Rhomboidal pattern, the annular granular pattern, the gray halo, the jelly sign, the white globule, the rosette sign, the white circle and the presence of grayish areas were significantly related to male sex. No dermoscopic sign was significantly related to the female gender (Table 3). Rhomboidal pattern, the annular granular pattern, the gray halo, the jelly sign and the white circle sign were significantly related to fair skin phototype (III) (Table 3). Rhomboidal pattern, the annular granular pattern, the gray halo, the white circle, the double circle and the double clods were the dermoscopic patterns significantly related to Xeroderma pigmentosum. The jelly sign with a superficial pigmentation was significantly related to the thin patches of PAK. Central crusts and scales were frequently found in thick plaques of PAK and fair skin phototype (III). The star like appearance of the lesion was present especially in hypertrophic PAK (Table 3).
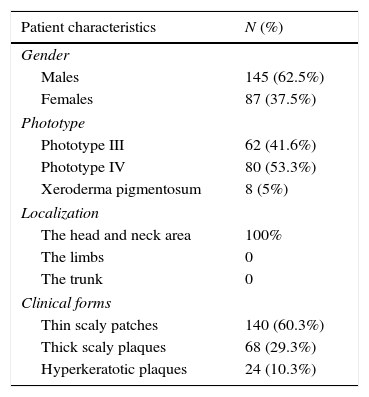
The epidemiological and the clinical characteristics of the patients.
| Patient characteristics | N (%) |
|---|---|
| Gender | |
| Males | 145 (62.5%) |
| Females | 87 (37.5%) |
| Phototype | |
| Phototype III | 62 (41.6%) |
| Phototype IV | 80 (53.3%) |
| Xeroderma pigmentosum | 8 (5%) |
| Localization | |
| The head and neck area | 100% |
| The limbs | 0 |
| The trunk | 0 |
| Clinical forms | |
| Thin scaly patches | 140 (60.3%) |
| Thick scaly plaques | 68 (29.3%) |
| Hyperkeratotic plaques | 24 (10.3%) |
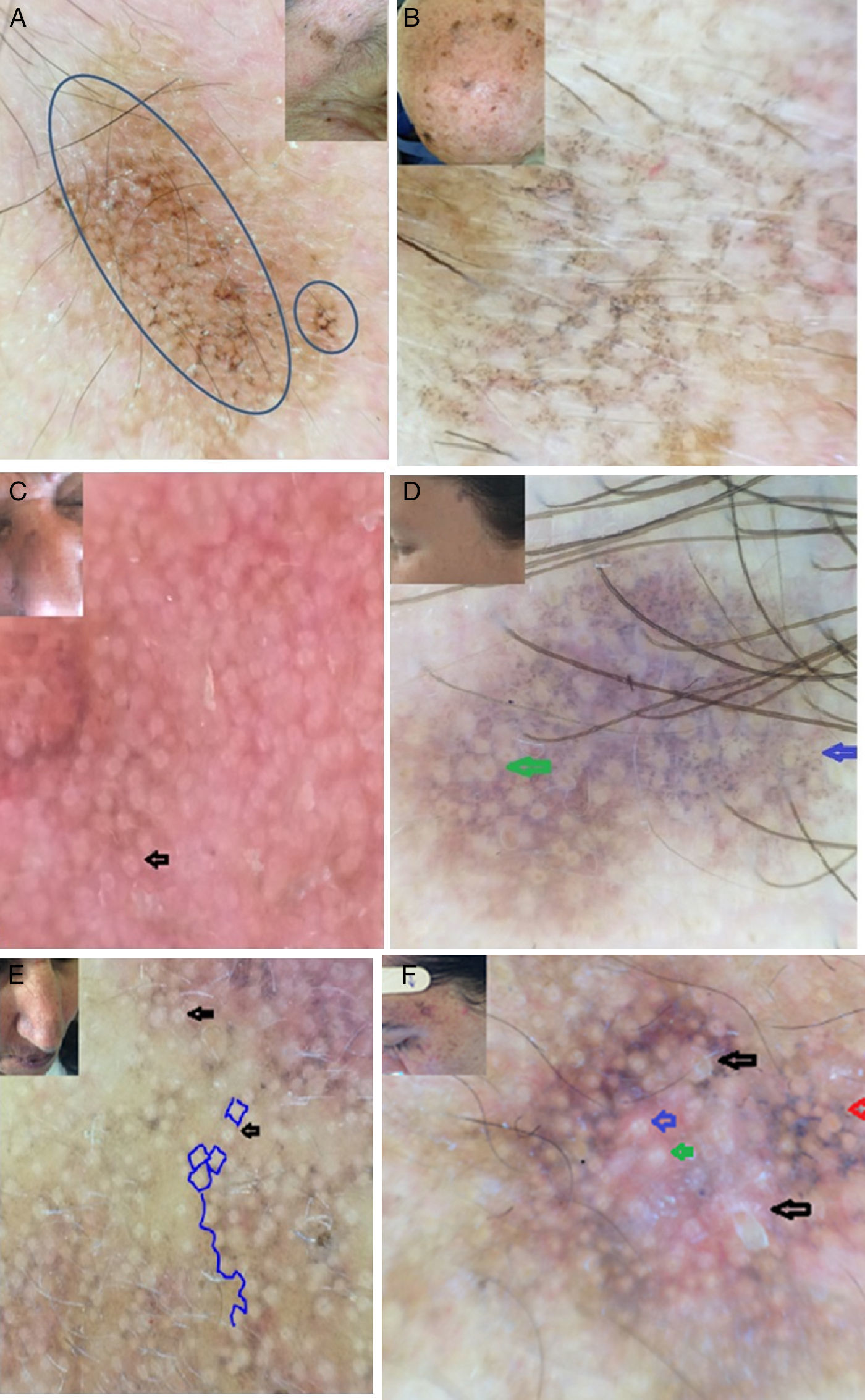
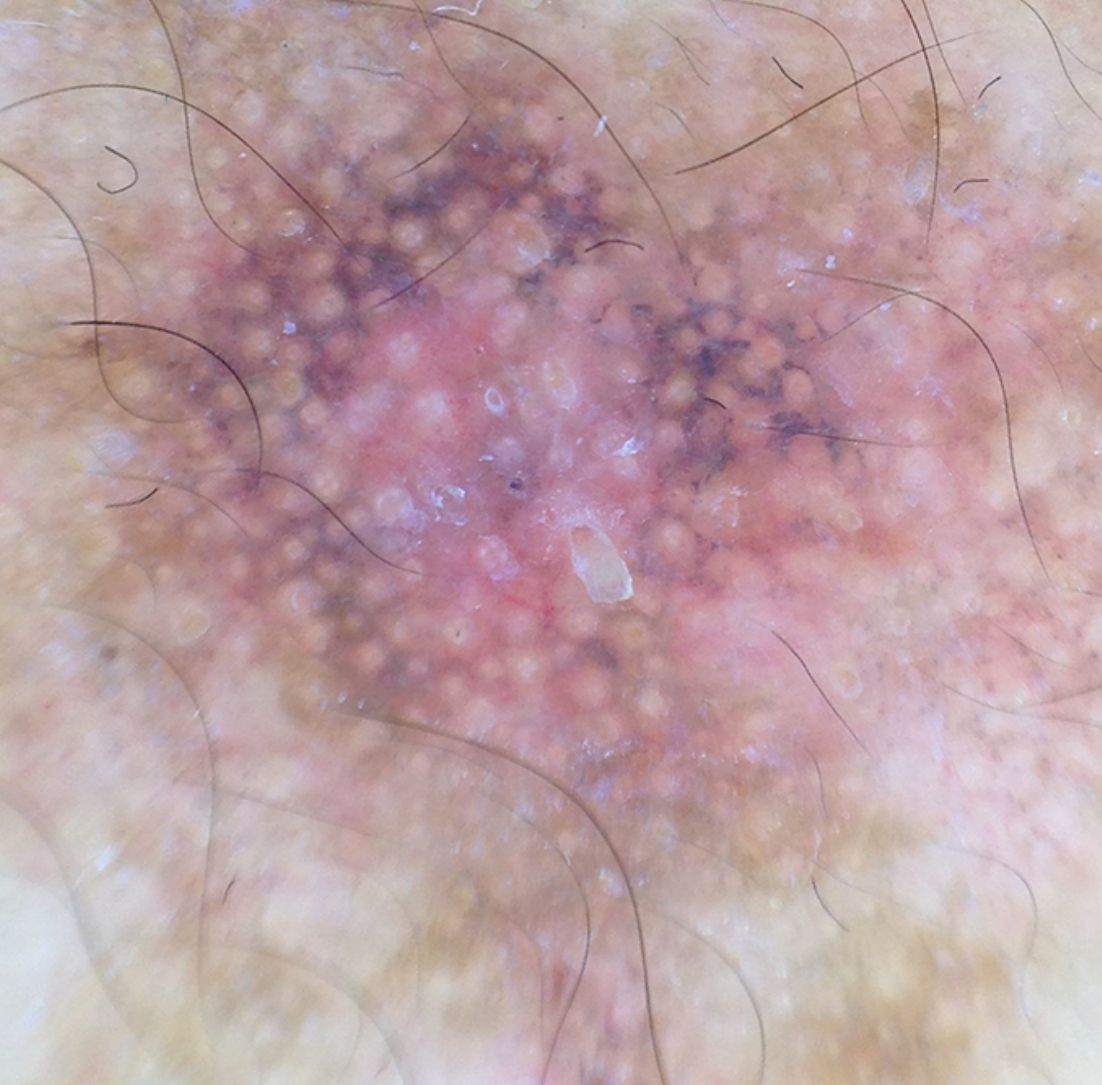
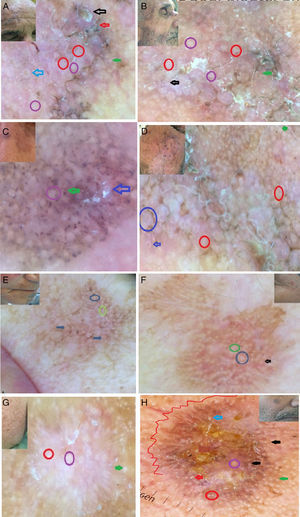
Clinical and dermoscopic images of PAK showing: A,C,E. the rhomboidal pattern (blue circle).C,E: the rosette sign (black arrow). B and D: the annular granular pattern (blue arrow), the inner gray halo around the yellowish central keratin (D: green arrow). F: the dermoscopic horn (black arrow), the gray halo around the yellowish central keratin (red arrow), the rosette sign (blue arrow), the double white clods (green arrow). G: Central crusts (black arrow), the white globule (red arrow), the rosette sign (blue arrow), the double white clods attached against each other (green circle). H: the superficial pigmentation with the jelly sign, the double white clods (green circle), the white globule (black arrow).
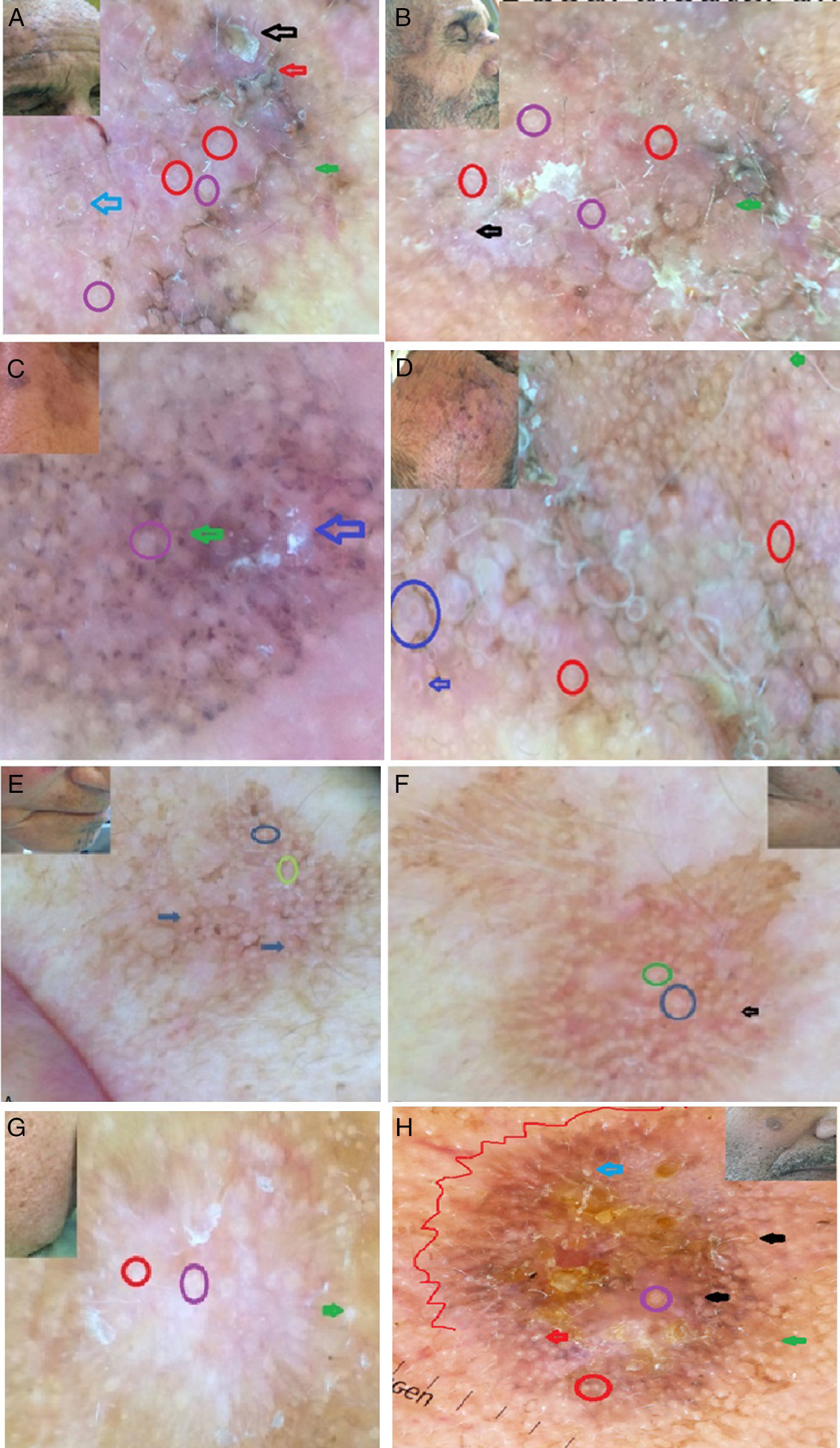
Clinical and dermoscopic images of PAK. A: the rhomboidal pattern with the dermoscopic horn (black arrow), the gray halo around the yellowish central keratin (blue arrow), the rosette sign (violet circle), the double white clods (red circle), grayish area and scales (red arrow). B: the rhomboidal pattern with the presence of white circles (black arrow), the gray halo around the yellowish central keratin (green arrow), the rosette sign (violet circle), the double white clods (red circle). C: the annular granular pattern with the dermoscopic horn (blue arrow), globules (green arrow), the rosette sign (violet circle). D: the rhomboidal pattern, the gray halo around the yellowish central keratin (blue arrow), the double white clods (red circle), the white circle (blue circle). E and F: the superficial pigmentation with the jelly sign with white globules (arrows), the rosette sign (circles). G: the star like appearance with the presence of white globules (green arrow), the rosette sign (violet circle) and the double white clods (red circle). H: the star like appearance with the presence of central crusts with peripheral white globules (green arrow), the rosette sign (violet circle), the double white clods (red circle), white circle around the follicular opening (black arrow) and the dermoscopic horn (red arrow).
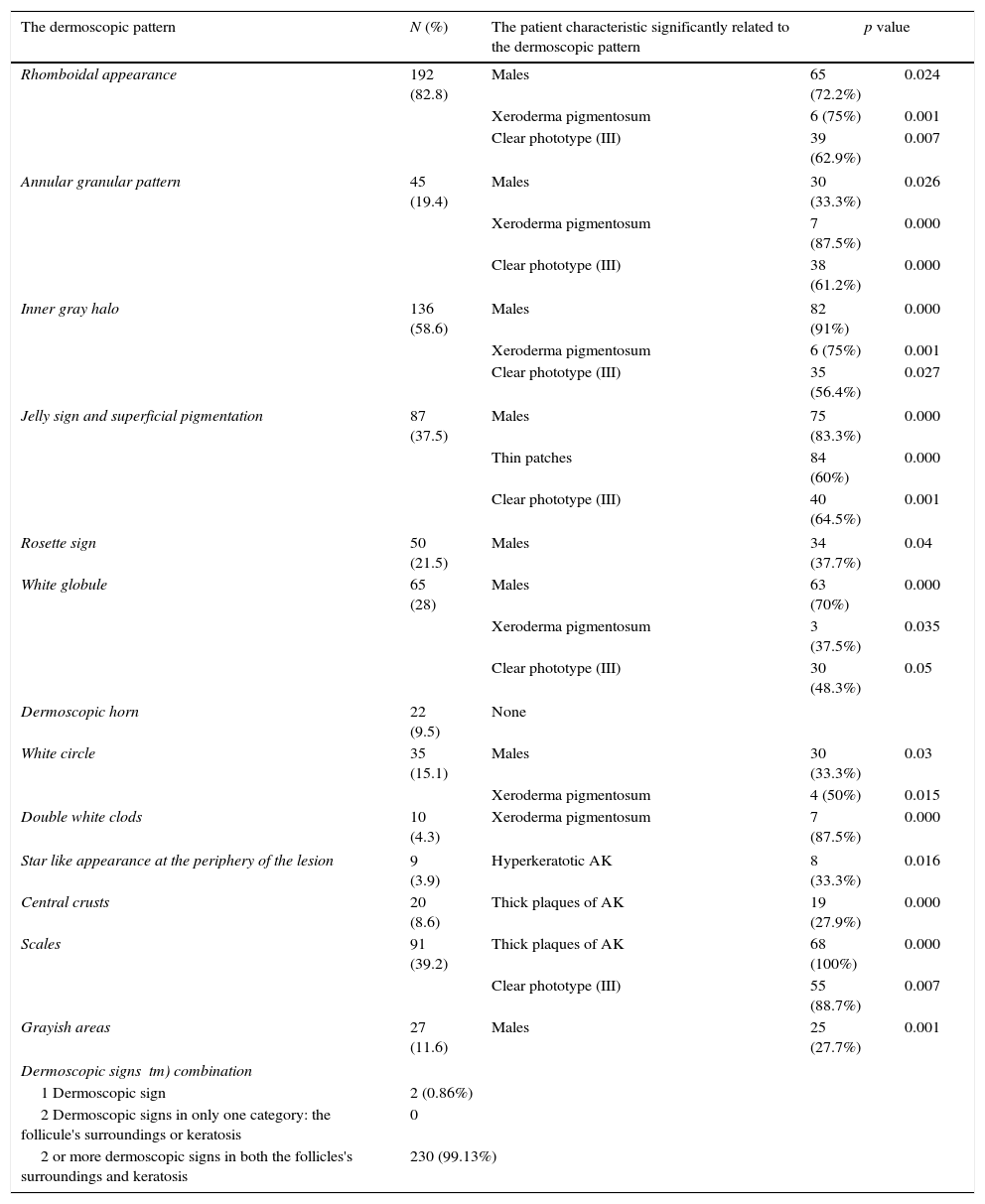
Univariate analysis showing the patients characteristics significantly related to the dermoscopic features.
| The dermoscopic pattern | N (%) | The patient characteristic significantly related to the dermoscopic pattern | p value | |
|---|---|---|---|---|
| Rhomboidal appearance | 192 (82.8) | Males | 65 (72.2%) | 0.024 |
| Xeroderma pigmentosum | 6 (75%) | 0.001 | ||
| Clear phototype (III) | 39 (62.9%) | 0.007 | ||
| Annular granular pattern | 45 (19.4) | Males | 30 (33.3%) | 0.026 |
| Xeroderma pigmentosum | 7 (87.5%) | 0.000 | ||
| Clear phototype (III) | 38 (61.2%) | 0.000 | ||
| Inner gray halo | 136 (58.6) | Males | 82 (91%) | 0.000 |
| Xeroderma pigmentosum | 6 (75%) | 0.001 | ||
| Clear phototype (III) | 35 (56.4%) | 0.027 | ||
| Jelly sign and superficial pigmentation | 87 (37.5) | Males | 75 (83.3%) | 0.000 |
| Thin patches | 84 (60%) | 0.000 | ||
| Clear phototype (III) | 40 (64.5%) | 0.001 | ||
| Rosette sign | 50 (21.5) | Males | 34 (37.7%) | 0.04 |
| White globule | 65 (28) | Males | 63 (70%) | 0.000 |
| Xeroderma pigmentosum | 3 (37.5%) | 0.035 | ||
| Clear phototype (III) | 30 (48.3%) | 0.05 | ||
| Dermoscopic horn | 22 (9.5) | None | ||
| White circle | 35 (15.1) | Males | 30 (33.3%) | 0.03 |
| Xeroderma pigmentosum | 4 (50%) | 0.015 | ||
| Double white clods | 10 (4.3) | Xeroderma pigmentosum | 7 (87.5%) | 0.000 |
| Star like appearance at the periphery of the lesion | 9 (3.9) | Hyperkeratotic AK | 8 (33.3%) | 0.016 |
| Central crusts | 20 (8.6) | Thick plaques of AK | 19 (27.9%) | 0.000 |
| Scales | 91 (39.2) | Thick plaques of AK | 68 (100%) | 0.000 |
| Clear phototype (III) | 55 (88.7%) | 0.007 | ||
| Grayish areas | 27 (11.6) | Males | 25 (27.7%) | 0.001 |
| Dermoscopic signs tm) combination | ||||
| 1 Dermoscopic sign | 2 (0.86%) | |||
| 2 Dermoscopic signs in only one category: the follicule's surroundings or keratosis | 0 | |||
| 2 or more dermoscopic signs in both the follicles's surroundings and keratosis | 230 (99.13%) | |||
The dermoscopic horn was not related to a special epidemiological or clinical characteristic of PAK in our patients.
DiscussionThe primary objective of the present study was to describe different dermoscopic patterns of PAK and to correlate the pattern with clinical characteristics of the patient and the evolutionary stage of the lesion. Only few previous studies1,5,8,9•14 focused on the pigmented form of AK, reporting the dermoscopic signs of PAK, without information about clinical characteristics of the patients. The most challenging form of PAK is the flat or thin patch, as already highlighted by Tschandl et al.8 The authors in their study examined a series of flat pigmented lesions, about half of the lesions were malignant. In our study, the jelly sign was the dermoscopic pattern significantly related to thin patches, in contrast to the study of Ciudad et al.1 where they didn tm)t find this feature in PAK patients. An other dermoscopic pattern found in our study and recently reported is the inner gray halo (IGH). The grayish color seems to be justified by the Tyndall effect of hypermelanotic keratinocytes located in the basal layer of the anaplastic epidermis, which spreads underneath the “umbrella” of normal epidermis in the follicles.5 This dermoscopic pattern is frequently found and was reported as the most sensitive and specific feature of PAK.5 In our study it was present in 58.6% of cases, which is lower than other studies where it was present in 94.1% of cases, and it was significantly noticed in clear phototype and sun damaged skin. White structures (clods and circles) are the signature sign of keratinization,14,15 and may be present in SCC and keratoacanthoma as well, yet if present, they are a very good feature that could allow to rule out the diagnosis of LM.
The star-like appearance at the periphery of the lesion was significantly related to hypertrophic PAK. This sign must lead the clinician to the necessity of the excision of the lesion in order to rule out a pigmented squamous cell carcinoma in situ. The dermoscopic horn is a new term that we have used in our study to describe the prominent central keratosis organized in the follicular openings. This feature was present in 9.5% of patients with thick and hyperkeratotic AK. We think that this sign would be of great help not only in the differential diagnosis of PAK, but also a good sign of keratinization and the benignity of the disease. Based on the evolutionary stages of PAK, the jelly sign with a superficial pigmentation was significantly related to the thin plates of AK. Central crusts and scales were frequently found in thick plaques of AK and clear phototype (III). The star-like appearance of the lesion was present especially in rough hypertrophic AK. This correlation is particularly useful for the prognostic and the therapeutic choice according to the degree of infiltration of PAK. As described in previous studies,2 these dermoscopic features were significantly more noticed in males than in females while the dermoscopic horn and grayish areas were not related to any special epidemiological or clinical characteristic of PAK in our patients. The description of significance of these dermoscopic features, their relationship with the phototype, the gender and the clinical form of PAK or in special types of skin like in xerodema pigmentusum (XP) patients is very important, because it may limit the unnecessary biopsies and excisions. Although it was not the aim of our study, and a control population is mandatory to talk about the diagnostic accuracy of PAK in comparison with LM, it seems that the diagnosis of PAK should be based on 2 or more dermoscopic signs in both the FSA and FkA. Notably, 99.1% of PAK lesions contained 2 or more dermoscopic signs in both the FSA and FkA. This theory of combination was already reported for the dermoscopic diagnosis of malignant pigmented skin lesions.16 Therefore, we suppose that the diagnosis of PAK especially flat lesions can not be based on the presence of a single criteria.
ConclusionIn conclusion, we emphasize the importance of the dermoscopic analysis according to the gender, the phototype, the type of skin and the clinical forms of PAK.
Ethical disclosuresProtection of human and animal subjectsEthical approval was obtained from the ethics committees in the Department of Dermatology of the University Hospital Center Hassan II in Fez-Morocco.
Confidentiality of dataAll the subjects agreed to participate in the study (prospectively) or to use their materials or data for research purposes (retrospectively).
Right to privacy and informed consentAll the subjects were informed of the conditions related to the study and gave their informed consent for publication. of their images for science.
Conflicts of interestThe authors declare that they have no conflicts of interest.