Sporotrichosis is a subcutaneous mycosis caused by the dimorphic fungus Sporothrix schenckii, which can have a subacute or chronic course.1 This disease has a worldwide distribution2 and is an emerging infection in Europe, where it has become quite common.3 The most frequent method of transmission is traumatic inoculation.4 This polymorphic mycosis has 4 clinical forms: lymphocutaneous, fixed cutaneous, disseminated, and extracutaneous. The extracutaneous and disseminated forms account for 4% of total cases6 and most often affect immunocompromised patients, in whom the fungus acts as an opportunistic agent.1 Amphotericin B is the treatment of choice for systemic disseminated forms.7
We report the case of a 54 year-old male construction worker with no relevant medical history except chronic alcohol consumption. The patient reported weight loss and intermittent fever associated with rapidly spreading dermatitis, which had developed 6 months earlier and was characterized by multiple, very painful necrotic pustules and ulcers of varying size with purulent exudate, some with a verrucous surface. The lesions affected a significant percentage of the body surface, exposing muscles and tendons (Fig. 1 A-D). The patient reported that he had undergone a right radical orchiectomy in another hospital for a testicular tumor that was likely malignant.
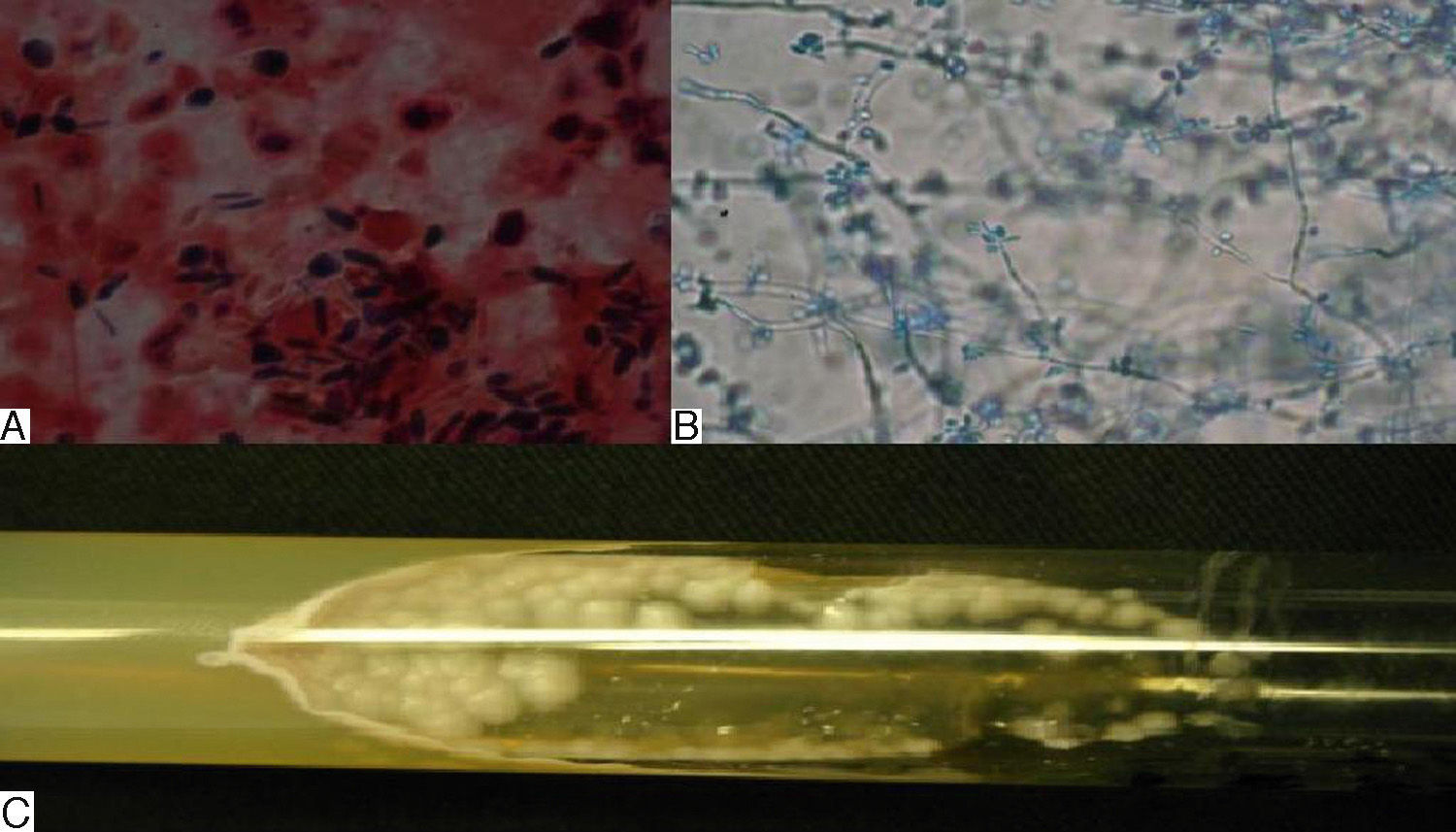
Direct examination of the skin lesions with potassium hydroxide and staining of smears with Gram stain and periodic acid Schiff (PAS) revealed abundant, elongated, cigar-shaped yeast cells (Fig. 2A). Microscopic analysis of cells cultured in Sabouraud dextrose agar showed conidia arranged laterally on the hyphae (Fig. 2 B), and identified the cells as S schenckii (Fig. 2C). The following bacterial aggregates were also observed: Acinetobacter baumanni (>250,000 colony-forming units) in a qualitative skin biopsy culture; multiresistant Pseudomonas aeruginosa in pustule exudate; and oxacillin-resistant Staphylococcus haemolyticus in a blood culture. The sporotrichin skin test was negative.
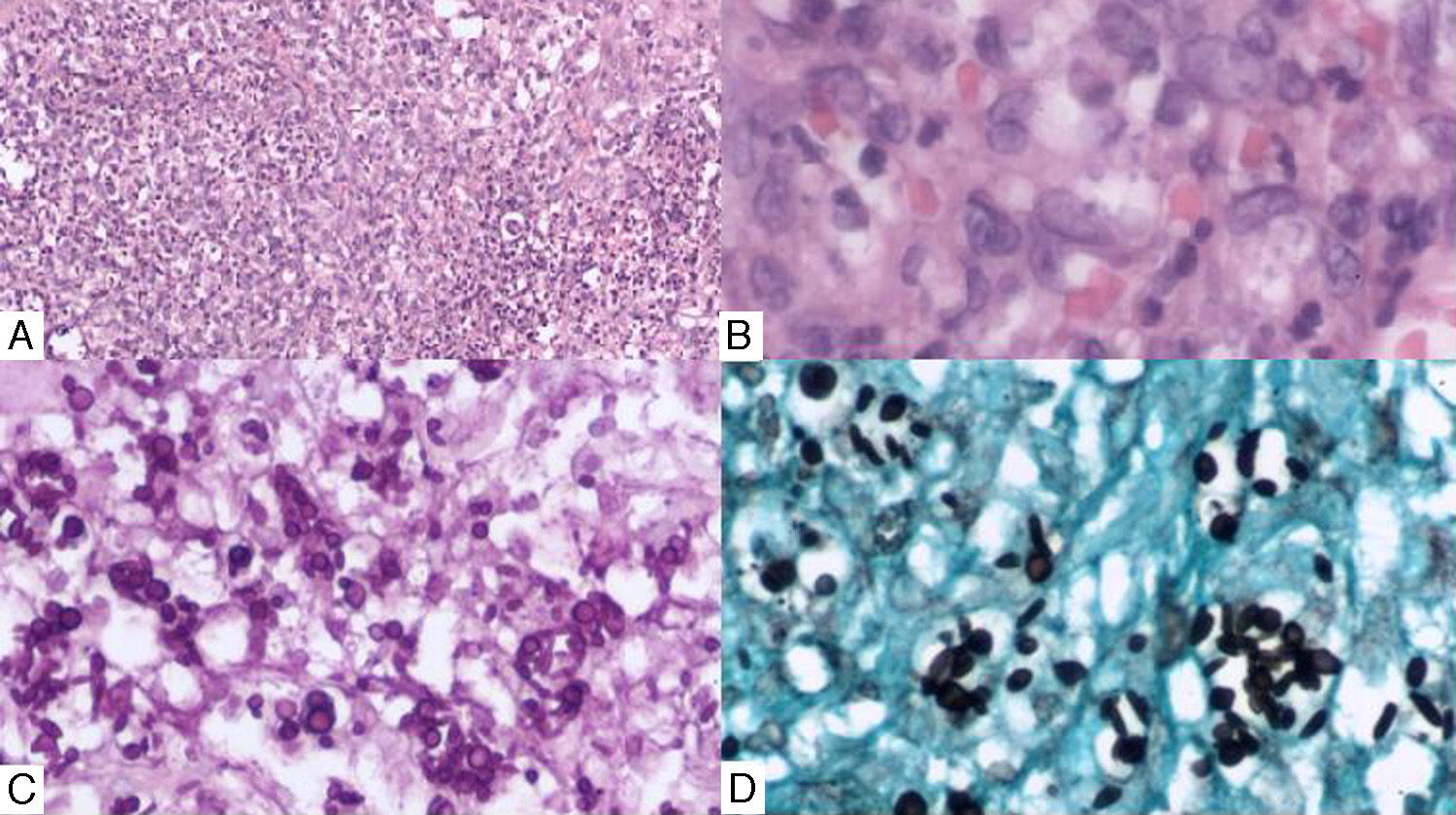
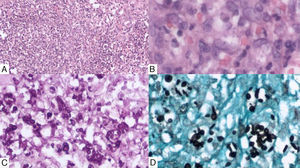
The skin biopsy showed nodular and diffuse inflammatory infiltrate, which was composed of lymphocytes, epithelioid histiocytes, multinucleated giant cells, and neutrophils, and produced suppurative granulomas and tissue necrosis (Figs. 3A and B). PAS and Grocott Gomori staining revealed abundant yeast cells, both round and elongated (Figs. 3C and D).
A, Histopathology of skin samples with suppurative granuloma containing lymphocytes, epithelioid histiocytes, and multinucleated giant cells (hematoxylin-eosin, original magnification ×5). B, Higher magnification image showing phagocytosed yeast cells (hematoxylin-eosin, original magnification ×40). C, Note the abundance of yeast cells (PAS, original magnification ×20). D, Ovoid and cigar-shaped yeast cells (Gomori-Grocott, original magnification ×20).
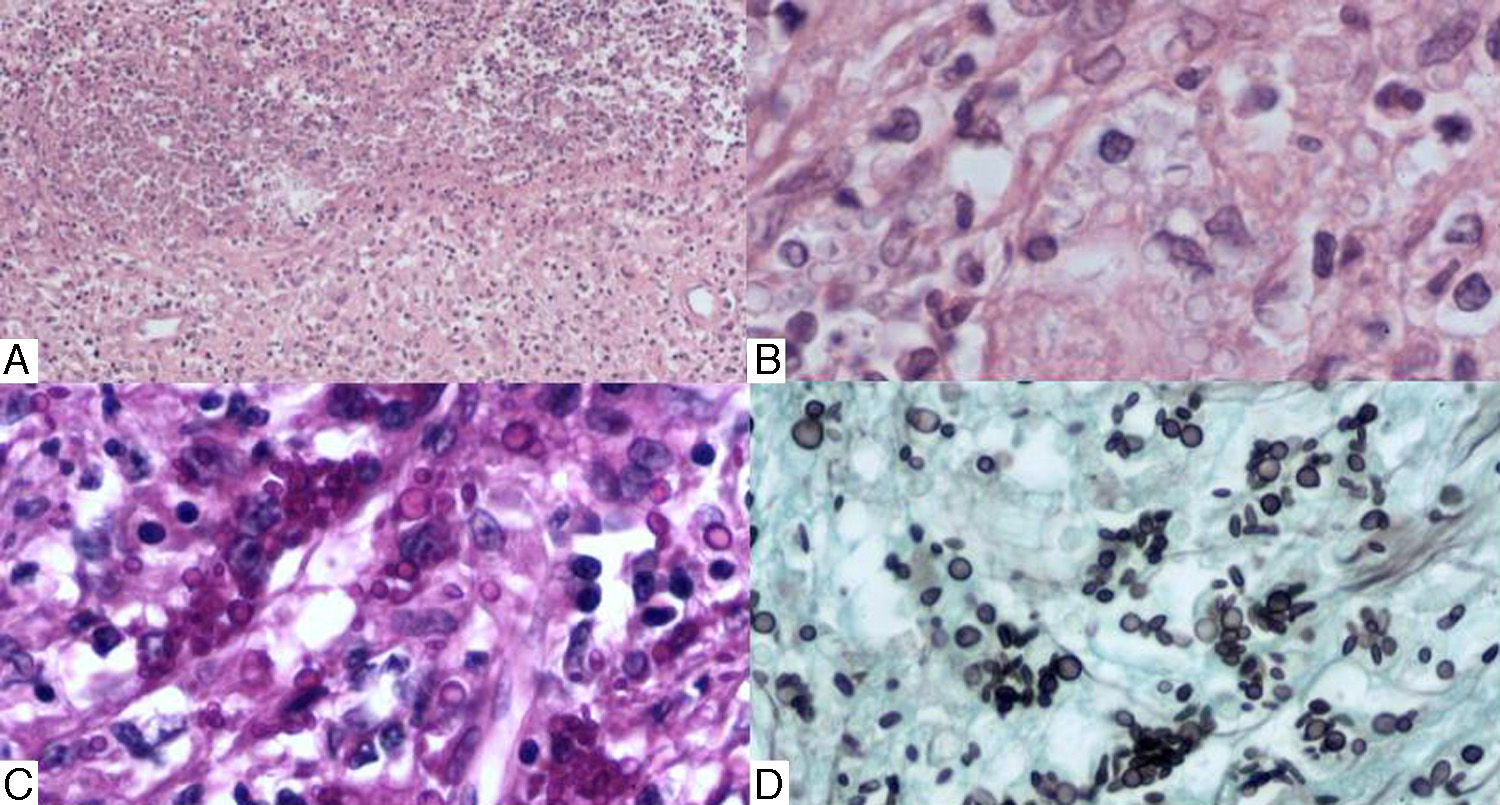
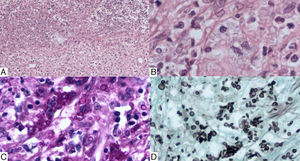
Histology of the tissue excised in the orchiectomy revealed similar findings; chronic granulomatous inflammation was observed with multinucleated giant cells, necrosis, and polymorphonuclear infiltration (Figs. 4 A and B). Staining showed spherical and cigar-shaped spores consistent with sporotrichosis (Figs. 4C and D).
Testicular biopsy. A, Substitution of the testicular parenchyma with chronic granulomatous inflammation with multinucleated giant cells, areas of necrosis, and polymorphonuclear infiltration (hematoxylin-eosin, original magnification ×5). B, Higher magnification image showing abundant ovoid yeast cells (hematoxylin-eosin, original magnification ×40). C and D, Spherical and cigar-shaped spores (PAS and Gomori Grocott, original magnification ×20).
Tumor staging ruled out fungal invasion of other organs, and HIV serology was negative.
The patient’ wounds were dressed and he was treated with amphotericin B deoxycholate for 14 days (total cumulative dose of 1.68g) in addition to antibiotics. The clinical course of infection was prolonged due to several complications related to treatment, associated infections, and the disease itself. These included septic shock, nephrotoxicity (acute renal failure, hypokalemia, hypomagnesemia, metabolic acidosis), liver failure, and disseminated intravascular coagulation. The patient died due to severe hemodynamic compromise.
Sporotrichosis is caused by the dimorphic fungus S schenckii.1 The most common presentation is lymphocutaneous; extracutaneous forms are rare, and are more prevalent in immunosuppressed patients.5
The case described here was classified as systemic disseminated sporotrichosis with additional extracutaneous involvement, with disseminated skin lesions, general malaise and internal organ involvement. This form is most common in immunocompromised patients.
The fungal infection was highly invasive, not only in terms of its cutaneous extension and testicular involvement, but also the degree of necrosis, depth of invasion, and the destruction of adjacent muscles and tendons. The sporotrichin skin test was anergic, indicating a poor immune response to fungal invasion by the patient. The only immunosuppression-associated factor detected was chronic alcoholism. The patient had also recently undergone orchiectomy at another institution due to clinical suspicion of a malignant testicular tumor, without prior confirmation of the nature of the lesion.
It was not possible to determine the mechanism of infection, but given the patient’ profession he may have acquired the microorganism via cutaneous inoculation, as the lesions first appeared on the left hand, and later spread throughout the body by hematogenous dissemination.
Sporotrichosis is definitively diagnosed by culture of the fungus obtained from a skin biopsy. Histology is usually not diagnostic, as the yeast is present in small amounts.3 However, in this patient, a large number of fungal elements were detected in the cutaneous and testicular biopsies.
The treatment of choice for extracutaneous and disseminated forms of sporotrichosis is amphotericin B, followed by long-term itraconazole administration in immunocompromised patients.7
In summary, our patient’ chronic alcohol abuse led to a state of severe immunosuppression, favoring the fulminant course of sporotrichosis with significant fungal invasion, which, together with a lack of prior clinical suspicion as well as complications associated with the treatment, concurrent bacterial infections, and the mycosis itself, resulted in the patient's death.
We thank Dr. José G. Chanona Vilchis, Head of the Department of Surgical Pathology of the Instituto Nacional de Cancerología, for providing testicular biopsy samples and histological descriptions.
We also thank Dr. Diana Vilar Compte of the Infectious Diseases Service at the Hospital General Dr. Manuel Gea González for microbiological identification of superadded bacterial infections, and Dr. Horacio Vidrio Morgado, Surgical Oncology Resident at the Instituto Nacional de Cancerología, and Dr. Alberto de los Ríos, Internal Medicine Resident at the Hospital General Dr. Manuel Gea González, for their role in the metabolic and surgical management of the patient.
Please cite this article as: Espinoza-Hernández C, Jesús-Silva A, Toussaint-Caire S, Arenas R. Esporotricosis diseminada con afección cutánea y testicular. Actas Dermosifiliogr. 2014;105:204–206.