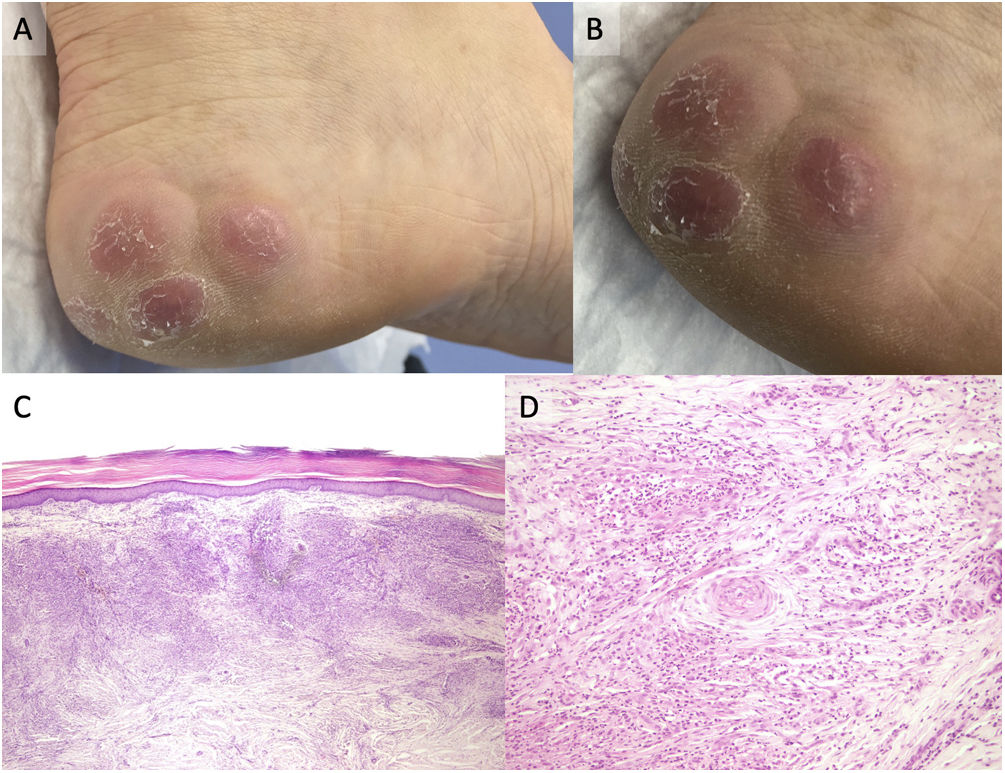
A 48-year-old woman with an unremarkable medical history presented with a 5-month history of 3 nodules on her left heel inner side (Fig. 1A and B). The 1–1.5cm nodules were erythematous, semi-firm, and minimally uncomfortable due to shoe friction. Biopsy revealed the presence of a dense infiltrate on the dermis primarily composed of neutrophils, plasma cells, and eosinophils. Leukocytoclastic vasculitis and collagen proliferation around the vessels (angiocentric, or onion skin storiform fibrosis) on the superficial and deep dermis were evident (Fig. 1C and D). To confirm the histopathological differential diagnosis and rule out other spindle cell neoplasms, immunohistochemistry was performed with S100 and CD34, which tested negative. Laboratory analyses included complete blood cell count, biochemistry, antinuclear antibodies (ANA), complement levels (C3 and C4), antineutrophil cytoplasmic antibodies (ANCA), C-reactive protein, angiotensin-converting enzyme (ACE), protein electrophoresis, and immunoelectrophoresis, all of which yielded normal, or negative results. Thoracic X-ray was unremarkable. A diagnosis of erythema elevatum diutinum (EED) was achieved, and dapsone treatment initiated with favorable progress.
EED is a rare dermatosis marked by recurrent papulonodules in extensor areas. In advanced stages, it can present as a late nodular variant that can mimic multiple skin neoplasms. Histopathologically, it exhibits leukocytoclastic vasculitis, dense neutrophil infiltrates, and collagen proliferation around the vessels (storiform or onion skin fibrosis, which are also present in other entities such as facial granuloma or IgG4 disease) leading to fibrotic regions. Leukocytoclastic vasculitis can be seen only in its early stages. In this late nodular variant, it is sometimes necessary to use immunohistochemistry techniques for the differential diagnosis of other spindle cell neoplasms, especially CD34 (to rule out dermatofibrosarcoma protuberans), and S100 (to rule out sclerotic neurofibroma, among others). Similarly, it is necessary to differentiate it from other entities such as leiomyoma, or superficial nodular fasciitis. Associations with conditions like rheumatoid arthritis, systemic lupus erythematosus, chronic myeloid leukemia, or monoclonal gammopathy should be ruled out. Dapsone is the preferred treatment.