A 63-year-old Chinese woman with no medical history of interest was referred to the dermatology clinic for long-standing skin lesions on the chest.
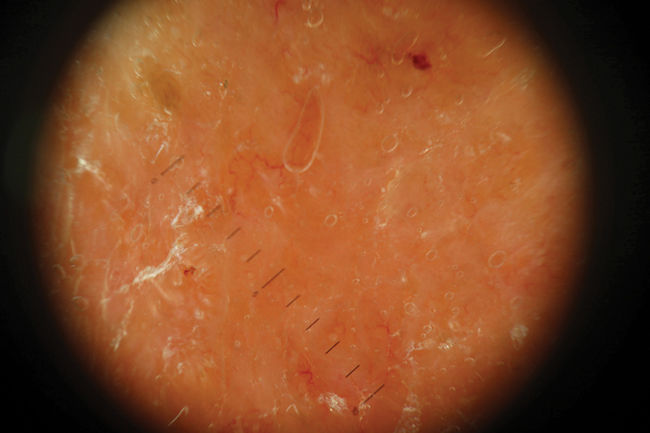
Physical ExaminationPhysical examination revealed a geographic plaque covering a large area of the chest, formed by the confluence of infiltrated and exophytic nodules, with some erosive areas. The patient presented marked bilateral axillary and submandibular lymphadenopathy (Fig. 1). Dermoscopy showed homogeneous orange areas with telangiectasias and erosions (Fig. 2).
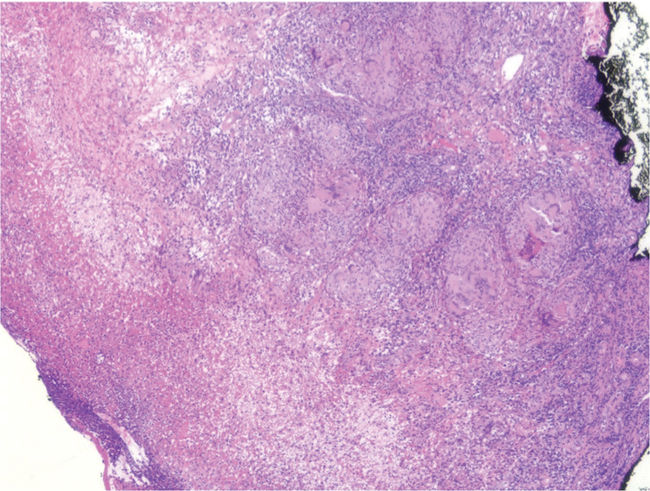
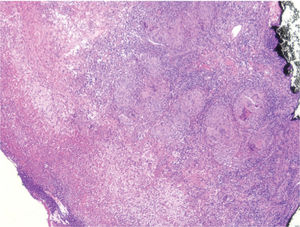
HistopathologyHistology of a punch biopsy showed the presence of compact, dense, superficial and deep granulomatous infiltrate with mild necrosis (Fig. 3). Ziehl-Neelsen staining, polymerase chain reaction (PCR) for Mycobacterium tuberculosis, and bacterial culture were negative.
Additional TestsLaboratory test findings revealed lymphopenia (0.9×109/L) and negative results for serological tests (human immunodeficiency virus [HIV], hepatitis B and C), interferon-γ release assay (IGRA), and tumor markers for lymphoproliferative processes (β2-microglobulin and lactate dehydrogenase [LDH]). Thoracic computed tomography revealed the presence of marked lymphadenopathy of the axillary and supraclavicular lymph nodes and the internal mammary chains, as well as calcified subpleural nodules, all suggestive of a lymphoproliferative syndrome. The results of a purified protein derivative (PPD) skin test were positive. The axillary lymph node was resected for histological and microbiological examination. Histology showed findings similar to those of the skin biopsy, and culture and PCR were positive for M. tuberculosis.
What is your diagnosis?
DiagnosisLupus vulgaris in a patient with active lymph node tuberculosis.
Treatment and Disease CourseTuberculostatic treatment was initiated with quadruple therapy (rifampicin, isoniazid, pyrazinamide, and ethambutol). The patient underwent follow-up for only 1 month, and was subsequently lost to follow-up after returning to her home country.
DiscussionTuberculosis continues to be a prevalent infection. Lupus vulgaris accounts for 60% of skin manifestations of tuberculosis. The clinical differential diagnosis should include other chronic granulomatous infections, cutaneous lymphomas, and even cutaneous carcinomatosis of an unknown primary tumor. It should be borne in mind that culture for mycobacteria is positive in only 40% of cases.1 Likewise, the diagnostic yield of Ziehl-Neelsen staining is limited by its poor sensitivity. Deep fungal infection and sarcoidosis should be considered as alternative histological diagnoses. The characteristic clinical presentation consists of granulomatous lesions that are usually asymptomatic (as in the present case), despite their striking presentation, grow slowly and progressively with a tendency towards ulceration, and have a characteristic “apple jelly”-like appearance on diascopy.2 Lupus vulgaris can be associated with active tuberculosis in other locations, such as the lymphatic system, as in our patient. Diagnosis is based on a suggestive clinical picture and compatible histology. IGRAs can produce false negative results, especially in patients with lymphopenia, regardless of etiology, as occurred in the present case. This technique consists of the detection of interferon-γ released by sensitized peripheral blood T lymphocytes after in vitro stimulation with specific M. tuberculosis antigens, which are absent in the attenuated strain of Mycobacterium bovis in the bacillus Calmette-Guérin (BCG) vaccine, and in most environmental mycobacteria.3 Of the 2 available IGRA types, QuantiFERON (QFT-GIT) and T-SPOT TB (ELISpot), the latter is the most sensitive in immunosuppressed patients.4 In individuals with profound immunosuppression (mainly due to HIV, but also severe non-HIV-associated lymphopenia), IGRAs can produce positive results when the test is repeated once the patient recovers their immunity after receiving appropriate treatment. The striking presentation in our patient may be a consequence of the delay in seeking a consultation (due to the language barrier or social difficulties), or the disease course in this particular patient.
FundingThis work has not received any type of funding.
Conflicts of InterestThe authors declare that they have no conflicts of interest.