Extramammary Paget disease (EMPD) is a rare cutaneous neoplasm. It is an intraepithelial adenocarcinoma that develops in areas rich in apocrine glands.1 The most commonly affected site is the vulva, followed by, in order of frequency, the scrotum, the perianal region, and the axillas.2 It is essential to screen for other tumors as EMPD is associated with malignancy at other sites.
A higher prevalence of the disease has been observed in white women aged between 50 and 80 years; because its clinical presentation is variable and nonspecific, EMPD is often confused with dermatitis, leading to delayed diagnosis and treatment.1
The traditional treatment of choice is surgical excision with wide margins, but even so, the disease has a high rate of recurrence (up to 43%).1
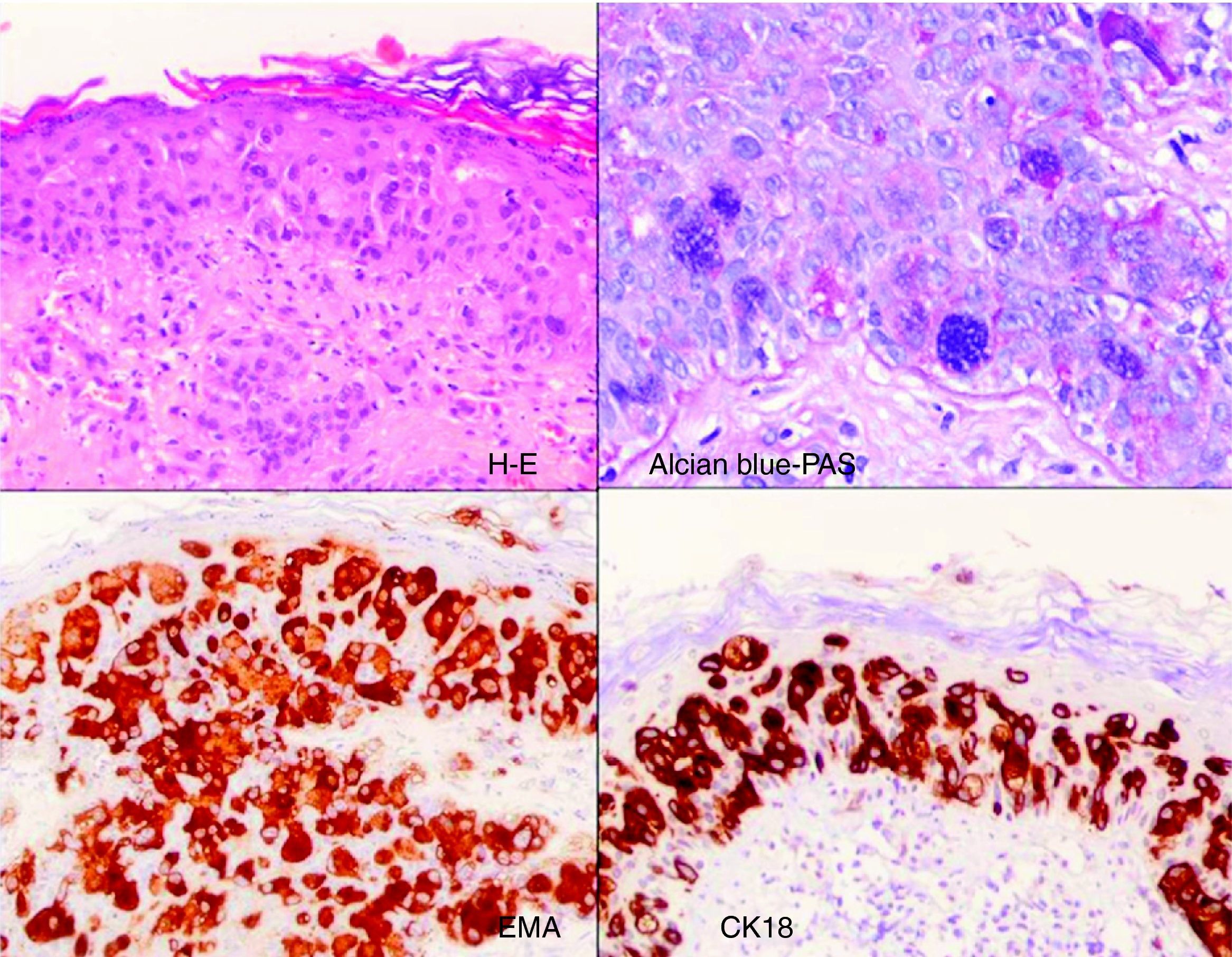
We describe the case of a 72-year-old woman, with no past history of interest, who consulted for a skin lesion with an eczematous appearance that had appeared on the vulva over a year earlier. Physical examination revealed a scaly erythematous plaque measuring 8 x 5cm containing whitish islands alongside eroded, exudative areas (Fig. 1). The patient said that she had been treated, without success, with topical corticosteroids, antibiotics, and antifungals for months.
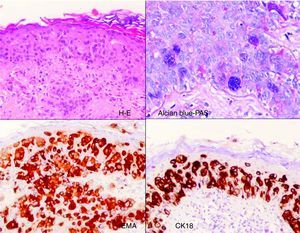
We performed a biopsy of the lesion to confirm the suspected diagnosis of EMPD. Histology showed hyperkeratosis, parakeratosis, acanthosis, and diffuse infiltration by cells with abundant pale cytoplasm and vacuolated nuclei (Paget cells) throughout the epidermis. There was no evidence of dermal infiltration. Immunohistochemistry was positive for carcinoembryonic antigen, epithelial membrane antigen, cytokeratin (CK) 7, and CK18 (Fig. 2).
On confirming the diagnosis of EMPD, we searched for associated malignancy, but the results were negative.
Because of the considerable functional and cosmetic sequelae associated with the surgical treatment of EMPD, we analyzed alternative treatments and opted for 5% imiquimod cream. The patient consented to treatment after having being informed of the good results achieved in cases similar to hers, as well as of the disadvantages associated with this therapy. After cleaning of the area, the cream was applied to the lesion and to 1 to 2cm of healthy skin around the lesion. Treatment was administered nightly 6 days a week. The patient tolerated the treatment well, despite the initial appearance of erosions and small crusts on the affected area. These lesions did not require interruption of the treatment. The patient was advised to apply fusidic acid ointment to the lesion to prevent superinfection and to help loosen the small crusts. Clinical resolution of the lesion was observed after 6 weeks of treatment (Fig. 3), but the patient was advised to continue treatment up to week 16. After this, the frequency of treatment was reduced to 3 times a week, with monthly outpatient follow-up in the dermatology department up to week 24. A skin biopsy performed several months later confirmed resolution of the disease and confirmed the absence of tumor cells. Once-weekly topical imiquimod was prescribed as maintenance therapy.3
At the time of writing, after 14 months of follow-up, there were no signs of recurrence.
The treatment of choice for EMPD has traditionally been surgical excision with control of margins or Mohs micrographic surgery. In recent years, however, there have been reports of small series and isolated cases in which EMPD has been treated with other methods such as electrodessication and curettage, laser therapy, photodynamic therapy with aminolevulinic acid, topical chemotherapy with bleomycin or 5-fluorouracil, and topical 5% imiquimod, all of which have shown the potential offered by nonsurgical approaches.4–7 It should be noted, however, that none of these treatments can be used to assess the persistence of disease. A standardized treatment regimen has not been established for imiquimod. Indeed, the literature contains varying reports of both treatment frequency (from once daily to 3 times a week) and duration (from 6 to 36 weeks). The maintenance regimen administered in our patient was based on previous recommendations to reduce the high risk of recurrence of the lesion.3
In our opinion, 5% topical imiquimod should be considered in patients with EMPD without dermal infiltration or associated underlying malignancy, and is particularly interesting for large lesions or patients with a high surgical risk.4–8 Its advantages over surgery are its noninvasive nature and its ability to target subclinical lesions. Nonetheless, further controlled studies are needed to confirm the effectiveness and safety of this treatment and to determine the most suitable treatment frequency and duration.
Please cite this article as: Hiraldo-Gamero A, et al. Enfermedad de Paget extramamaria tratada con imiquimod 5% crema. Actas Dermosifiliogr.2011;102:554-56.