Facial discoid dermatosis (FDD) is a condition characterized by papules-plaques primarily affecting the face. FDD has been associated with psoriasis, seborrheic dermatitis, and pityriasis rubra pilaris. We conducted a retrospective multicenter study with 13 patients diagnosed with FDD in Spain (2014–2022). Patient demographics, clinical presentations, histopathological findings, and treatment outcomes were collected.
FDD shows as erythematous-orange, nummular papules and/or plaques with dry scales that primarily affect the facial region. Histopathological analysis revealed a consistent pattern of psoriasiform hyperplasia with confluent parakeratosis, without neutrophils within the epidermal layers.
This study provides essential insights into the clinical and histopathological features of FDD within a predominantly Caucasian patient cohort. The presence of distinct clinical features and consistent histological findings underscores the uniqueness of FDD. However, the variability in histological features and persistence of lesions despite various treatments highlight the need for further research to better understand the pathogenesis of FDD and develop effective therapies.
La dermatosis discoide facial (DDF) se caracteriza por la presencia de pápulo-placas principalmente faciales. Se ha relacionado con la psoriasis, la dermatitis seborreica y la pitiriasis rubra pilaris. Este estudio retrospectivo y multicéntrico incluyó a 13 pacientes diagnosticados de DDF en España (2014-2022). Se recopilaron datos demográficos, clínicos e histopatológicos, así como resultados del tratamiento.
La DDF se manifiesta con pápulas y/o placas eritemato-anaranjadas, descamativas, numulares, localizadas predominantemente en la región facial. El análisis histopatológico reveló un patrón de hiperplasia psoriasiforme con paraqueratosis confluyente, sin neutrófilos en las capas epidérmicas.
Este trabajo proporciona información sobre las características principales de la DDF en una cohorte mayoritariamente caucásica. La presencia de signos clínicos distintivos y hallazgos histológicos constantes resalta su singularidad. No obstante, la variabilidad histológica y la persistencia de las lesiones, a pesar de diversos tratamientos tópicos, subrayan la necesidad de investigaciones adicionales para comprender su patogénesis y desarrollar terapias efectivas.
Facial discoid dermatosis (FDD) is an entity first described by Ko et al. in 2010. Although its etiology remains unknown, a relationship with psoriasis, seborrheic dermatitis, and pityriasis rubra pilaris (PRP) has been postulated.1 Clinically, FDD is characterized by the presence of erythematous-orange papules and/or plaques, nummular, with dry scales on the surface, mainly affecting the facial region, although involvement of the neck has also been described.2 Histologically, FDD biopsies reveal parakeratosis, mild psoriasiform acanthosis, and perivascular lymphocytic infiltrate; some authors consider this disorder a variant of PRP based on some of its histopathological characteristics.1,3
Its distinctive clinical features are its lack of response to topical treatments and a chronic course of the disease.1–4 Before establishing a diagnosis of FDD, it is essential to exclude other conditions that present similar clinical and histological characteristics.
We present a case series of FDD with the aim of providing a comprehensive understanding of the clinical and histological features of FDD, mainly in individuals of Caucasian descent.
Material and methodsWe conducted a retrospective multicenter study, including 13 patients from 4 Spanish centers diagnosed with FDD between 2014 and 2022.
The inclusion criterion was patients with a final diagnosis of FDD based on clinical and/or histological criteria.
A comprehensive collection of demographic and clinical variables was performed, including gender, age, cutaneous clinical presentation—including disease onset and lesion location—laboratory analysis, histopathological findings, treatments, and disease progression.
ResultsA total of 13 patients were included, with a female predominance (11/13; 85%). Ten patients were of Caucasian ethnicity, while 2 were of Latin American descent and 1 of Afro-Caribbean origin. The mean age at diagnosis was 33.2 years (range, 18–46), and a high proportion (76.9%; 10/13) exhibited lesions restricted to the face, while 3 patients also exhibited lesions on the neck (2/13) and upper trunk (1/13).
Clinically, most patients exhibited erythematous-orange, scaly, nummular papules and/or plaques, except for the patient of Afro-Caribbean origin, whose clinical presentation was different, with a dark tone and follicular accentuation, which reinforced the clinical suspicion of lupus erythematosus (Fig. 1).
Among the complementary tests performed in all patients, blood tests with general and autoimmunity profile (ANA, anti-dsDNA, Ro, La, Sm, RNP, and complement levels) were included, without any significant alterations. Tests for anti-Dsg1 and anti-Dsg3 antibodies, performed in 3 patients with acantholysis in the histology tested negative.
In addition, 3 patients had a personal history of atopic dermatitis—without active eczema—and 2 had hypothyroidism.
The most frequently considered clinical/histopathological differential diagnoses were eczema, lupus erythematosus, dermatophytosis, psoriasis, seborrheic dermatitis, superficial pemphigus, and PRP.
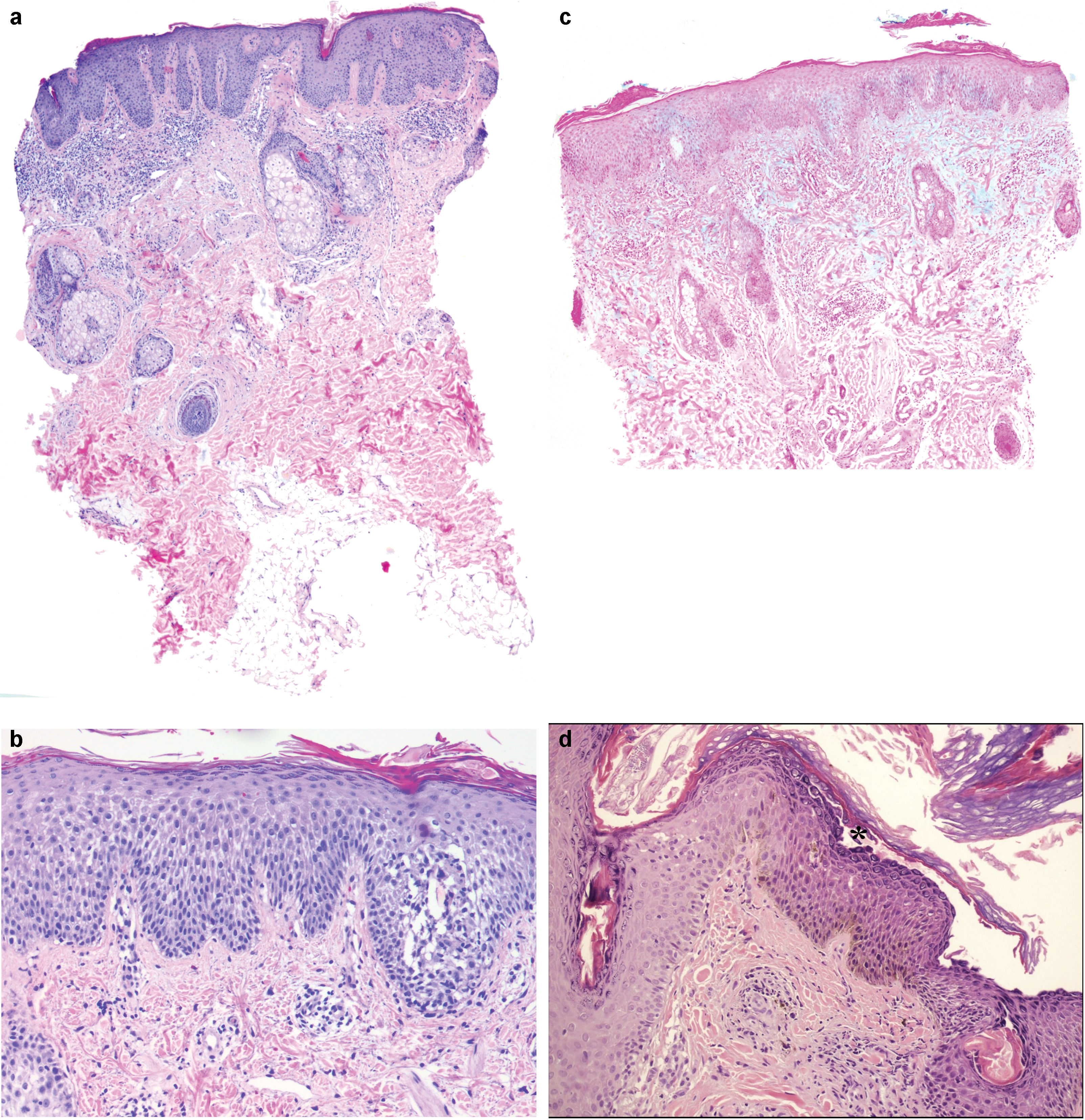
Histopathological evaluation was performed in 10 cases of facial lesions by 3mm punch biopsies, which revealed an epidermis with characteristics of regular/psoriasiform hyperplasia (7/10) with confluent parakeratosis (9/10), but with an absence of neutrophils in the epidermal layers. Perivascular lymphohistiocytic inflammatory infiltrate (9/10) and spongiosis areas (8/10) were consistently observed. Spongiosis was mild, mainly affecting the lower and middle layers of the epidermis, except for 1 case where it was markedly pronounced. In 2 additional cases, it was associated with lymphocytic exocytosis.
However, dilated follicular plugs were only observed in 5 of the 10 biopsies—although it was not possible to observe follicles in all biopsies—and focal superficial acantholysis was found in 3 biopsies (Fig. 2); nonetheless, indirect and direct immunofluorescence performed in these cases turned out negative, ruling out bullous disease.
Histological characteristics. (a) Biopsy of one of the facial lesions, presence of regular/psoriasiform hyperplasia associated with confluent parakeratosis and dilated follicular structures. The absence of neutrophils within the epidermal layers stands out. In addition, perivascular lymphohistiocytic infiltrates and mild atrophy of sebaceous glands are observed (patient #2, H&E, panoramic view). (b) Biopsy from patient #4 revealing the presence of epidermis with acanthosis, parakeratosis, and foci of spongiosis more accentuated at the level of the follicular epithelium (H&E, ×40). (c) Alcian blue staining reveals the presence of mucin in the mid-dermis (patient 5, ×20). (d) Subcorneal acantholysis in the biopsy sample from patient #10 (asterisk), along with basal hyperpigmentation, pigment-laden macrophages in the dermis, and a mild perivascular lymphocytic infiltrate. Presence of Demodex in the follicular orifice (H&E, ×20).
Furthermore, although alcian blue staining showed the presence of mucin in the mid-reticular dermis in 2 out of the 10 biopsies, no other findings consistent with the diagnosis of lupus erythematosus (hydropic degeneration of the basal layer, thickening of the basement membrane—PAS positive—or extensive lymphoplasmacytic inflammatory infiltrate) were observed.
Partial atrophy of the sebaceous glands was observed in the biopsy of patient #2 (Fig. 2a), without being significantly detected in the other biopsies studied.
Notably, the lesions persisted despite multiple therapeutic approaches, with an average of 3.38 treatments per patient. The most widely used treatments were topical glucocorticoids (13/13), calcineurin inhibitors (9/13), retinoids (7/13), and topical antifungals (5/13). The duration of treatment was difficult to estimate; however, in all cases, treatments were maintained for, at least, 1 month. In addition, other systemic treatments with variable durations were used, providing equally unsatisfactory results: hydroxychloroquine, ivermectin, azathioprine, phototherapy, or tetracyclines.
The follow-up period was variable, ranging between 10 months and 10 years (median, 15 months) (see Supplementary data).
DiscussionIn our series, the clinical presentation of FDD is similar to previous descriptions (erythematous-orange, scaly, nummular papules and plaques affecting the facial region).1,4 However, there is substantial histological variability associated with this disease, which has led to ongoing debate about its classification and relationship with other dermatological disorders.3,5,6
The presence of psoriasiform hyperplasia with confluent parakeratosis and absence of neutrophils seems to be consistent with cases reported in the literature.1 However, the presence of spongiosis areas was more frequently observed in our cohort vs previous descriptions (70% vs 43%, respectively), while the occurrence of dilated follicular plugs was less frequent vs that reported in the literature (50% vs 71%, respectively).1,7
Furthermore, our findings show a lower prevalence of acantholysis in Western patients with FDD vs Asian populations, since the 8 cases in which superficial acantholysis has been described belong to the cohort of the Asian population reported by Gan et al.3
Similarly, the presence of mucin in the mid-reticular dermis—not previously described—does not seem to rule out the diagnosis of FDD.8
The efficacy of topical treatments in FDD is, to date, limited, with few reported cases demonstrating significant improvement after several weeks on topical therapy (6–8 weeks).9–11 However, Rypka et al. reported the first case of FDD that showed a favorable response to ustekinumab after only 6 weeks of treatment.2
The presence of atrophy at the level of the sebaceous glands in the histology of FDD lesions has been previously described, evidencing an association of this entity with psoriasis or seborrheic dermatitis.6 This hypothesis would explain the favorable response to treatment with ustekinumab through a predominant profile of Th17 effector T cells in FDD lesions, characteristic of psoriasis. Furthermore, this hypothesis would not exclude the possibility that FDD is a subtype of PRP, since this condition has also shown a response to this therapeutic approach.12,13
In addition, it is well established that acantholysis can be observed in PRP lesions, although not in psoriasis or seborrheic dermatitis. Therefore, our finding of acantholysis in FDD lesions could be another piece of supporting evidence to consider this entity as a variant of PRP.14
To date, our cohort of FDD cases is the most extensive series ever described the literature and includes a substantial number of Caucasian patients underrepresented in previous series. Based on this series, we conclude that, clinically, FDD is characterized by distinctive features such as erythematous-orange, nummular papules and plaques with dry scales on the surface, predominantly affecting the facial region. In addition, a histological pattern of psoriasiform hyperplasia with confluent parakeratosis, without neutrophils, seems to be the predominant histopathological finding, while superficial acantholysis or follicular plugging may be additional—although less specific—characteristics, at least, in the Caucasian population.
We emphasize the importance of considering the clinical presentation, histological findings, and therapeutic response together for an accurate diagnosis of this entity.
Further research is still needed to better understand the pathogenesis and classification of FDD, as well as its different treatment options.
Conflicts of interestNone declared.