Facial discoid dermatosis is a recently described entity that presents with erythematous, frequently annular, scaling papules and plaques located exclusively on the face. The main characteristic of this condition is the presence of persistent lesions that do not respond to topical or systemic treatments. The clinical differential diagnosis includes other entities involving papulosquamous lesions on the face, such as seborrheic dermatitis, tinea faciei, cutaneous lupus erythematosus, and psoriasis.
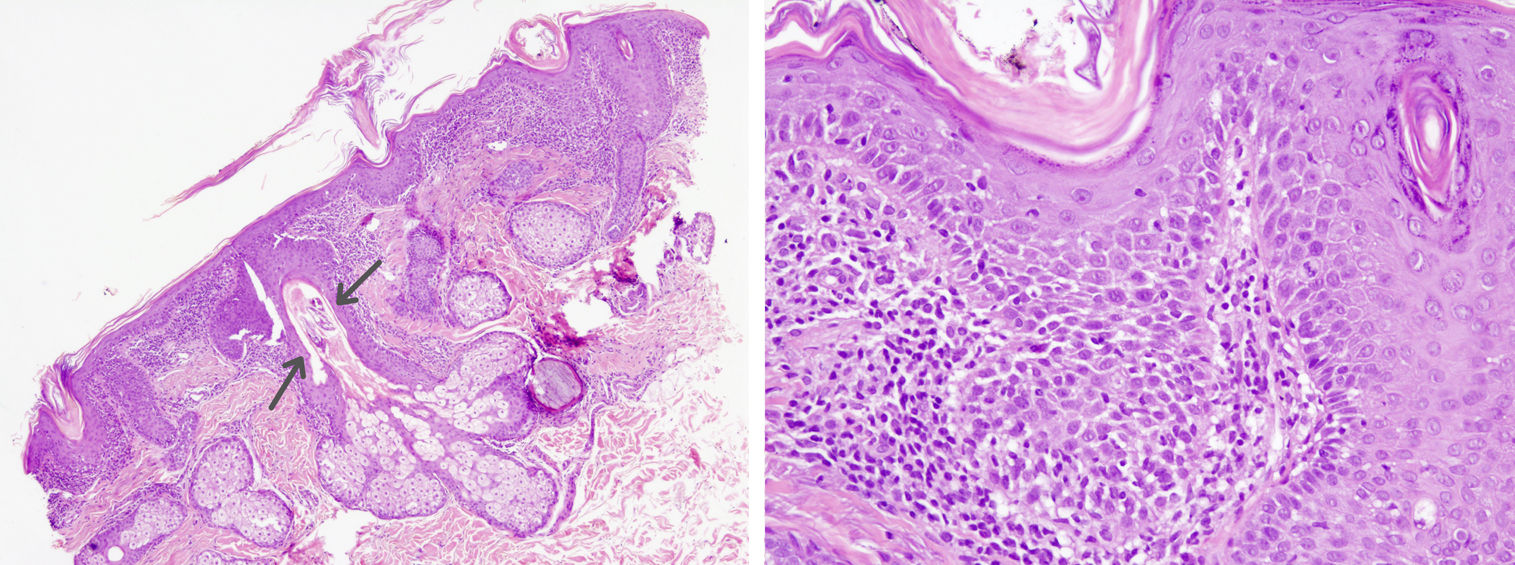
A 45-year-old woman with familial hypercholesterolemia presented with persistent facial lesions present since adolescence. The lesions had shown a complete lack of response to numerous treatments, including topical corticosteroids and calcineurin inhibitors and systemic methotrexate and hydroxychloroquine. Physical examination showed erythematous, scaling papules and plaques with a slightly orange, seborrheic appearance on the cheeks and forehead (Figs. 1 and 2). There were no lesions on any other parts of the body, including the mucous membranes, palms, soles, and scalp. Biopsy of a lesion showed mild epidermal acanthosis, hyperkeratosis with foci of parakeratosis, follicular corneal plugs, a moderate interstitial and perifollicular inflammatory infiltrate in the superficial dermis, and Demodex species in the hair follicles (Fig. 3). There was no evidence of basal vacuolar changes, basement membrane thickening, or mucin deposition. Direct immunofluorescence was negative. Blood tests were negative for antinuclear antibodies, including anti-Ro/SSA and anti-La/SSB antibodies, and showed a slightly decreased C3 fraction (83 mg/dL) without clinical relevance. Despite the absence of a definitive diagnosis, it was decided to retreat the patient with oral hydroxychloroquine and high-potency topical corticosteroids in view of the possibility of cutaneous lupus erythematosus, but there was no response. The presence of abundant Demodex species in the biopsy specimen, combined with the other manifestations, was also suggestive of a rosacea component, and the patient was started on a full course of oral metronidazole and ivermectin. Again, she showed no clinical response. Considering the clinical and histologic findings and the lack of response to both topical and systemic treatments, we established a diagnosis of facial discoid dermatosis. On reviewing the literature, we decided to treat the patient with topical calcipotriol and betamethasone based on the experience described in a case report.1 We are currently waiting to see how she responds.
Mild epidermal acanthosis, hyperkeratosis with foci of parakeratosis, follicular corneal plugging, a moderate inflammatory infiltrate in the superficial dermis, and Demodex species in the central follicle (arrows) (left, original magnification ×40; right, original magnification ×200).
Facial discoid dermatosis was first described in 2010 in a series of 3 cases in which the authors described pink-orange, frequently annular, lesions with a scale that were located exclusively on the face.2 The lesions remained stable for years and were resistant to multiple treatments. Histopathologically, they showed epidermal acanthosis, parakeratosis, and follicular plugging.
Ten other cases have been described since.1,3,4 Based on the few reports in the literature, facial discoid dermatosis appears to be more common in women (male to female ratio, 1:5.5), tends to develop in the third decade, and has a clear predilection for Asians. Lesions are limited to the facial region and mainly affect the cheeks (93%), the chin (69%), and the forehead (38%). They typically remain stable for years and respond poorly to treatment. Partial response to certain treatments, such as tacrolimus and topical corticosteroids3 and topical calcipotriol/betamethasone combined with low doses of oral acitretin, has been described in 53% of cases.1 Of note, 1 patient developed type II pityriasis rubra pilaris (PRP) during follow-up. The most common histologic findings reported are psoriasiform epidermal hyperplasia (92.3%), hyperkeratosis with parakeratosis (84%), a superficial perivascular lymphocytic infiltrate (76.9%), and follicular plugs (61.5%).
The origin of facial discoid dermatosis is unknown. The report of a case that progressed to PRP, combined with the similar histologic findings to those observed in PRP and the poor responses to treatment, has led some authors to postulate that facial discoid dermatosis might actually be a subtype of PRP.1–4 There are, however, clear clinical differences between the 2 entities and much remains to be elucidated. We believe that the case presented in this report is a clear example of facial discoid dermatosis, a little-known and probably underdiagnosed dermatosis. Of note is its persistent clinical course, with lesions that can remain stable for many years, and its lack of response to currently available treatments.
Please cite this article as: Condal L, Quer A, Ferrándiz C, Bielsa I. Dermatosis discoide facial, una entidad enigmática. Actas Dermosifiliogr. 2021;112:934–935.