Procedures involving dermal filler for cosmetic purposes are carried out every day. However, this practice is not risk-free. One reported complication is that of foreign-body granulomatous reaction to a component of the filler.1,2 One of the initial treatment options is infiltration with corticosteroids, although the condition can also be managed with oral allopurinol.3–5
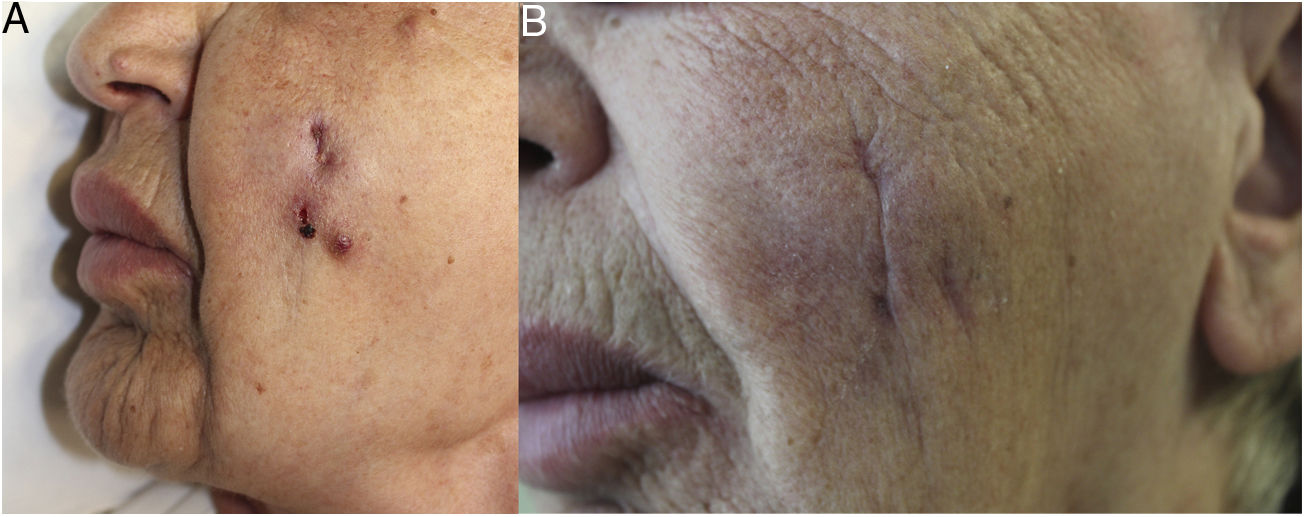
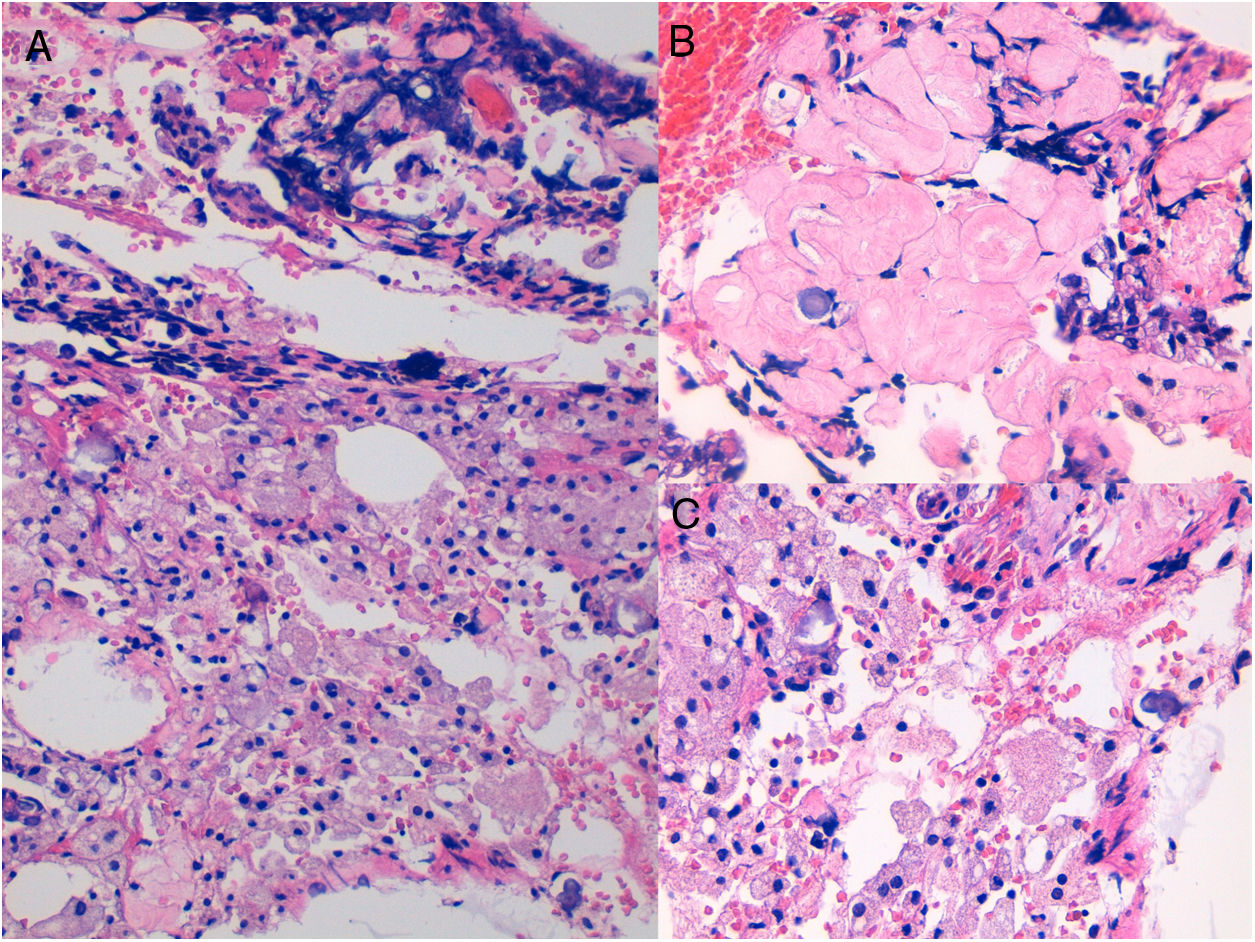
An 83-year-old woman was referred for a lesion on her left cheek that had been treated for 3 weeks with oral antibiotic therapy (amoxicillin clavulanate, 875/125mg/8h), surgical drainage, and a 2-week tapering course of oral corticosteroids (starting with prednisone 30mg/d), albeit with minimal improvement. The patient's history was remarkable only for the fact that she reported undergoing surgery in this area some years previously. Similarly, she denied having received infiltrations or fillers. Physical examination revealed a fistulous tract with purulent discharge, depressed areas of scarring, and, adjacent to these areas, a reddish exudative papular lesion. The lesions were surrounded by an edematous area with a doughy consistency, occupying almost the whole cheek (Fig. 1A). Ultrasound revealed several nodular hypoechoic lesions that differed in size, the largest being 1cm in diameter. These were mainly superficial, with vascularization in the interior and slightly increased echogenicity of the underlying subcutaneous tissue. A histopathology study was recommended. Biopsy revealed a foreign-body granulomatous reaction in the dermis and subcutaneous tissue, with the presence of 2 different materials in the histology sections: a superficial eosinophilic material with no associated granulomatous reaction and a deeper basophilic amorphous material accompanied by a moderate inflammatory infiltrate composed of macrophages with granular cytoplasm (Fig. 2). Given the diagnosis of a foreign-body granulomatous reaction and the uselessness of previous treatments, we offered the patient the possibility of treatment with allopurinol under a compassionate use regimen (300mg/d, po) combined with mometasone furoate in blocks of 15 days every month. This treatment led to a slow but gradual improvement with fluctuations until the lesions were totally controlled 8 months later (Fig. 1B), with resolution of the initial soft tissue edema and atrophic scarring. Treatment was well tolerated, and no adverse effects were reported during follow-up.
While relatively harmless, infiltration of dermal filler is not free of complications, which can be classed as short-term, such as hematomas and infections, and long-term, such as migration of material or foreign-body granulomatous reactions, as in the present case. Granulomatous reactions are more frequent with longer-term fillers, especially those that are permanent or semipermanent, such as silicone, polyacrylamide, and polymethyl methacrylate polymers. Once infection has been ruled out, the most common maintenance treatment reported in the literature is application of topical corticosteroids followed by infiltration of corticosteroids alone or combined with 5-fluorouracil.1,2 If the product used is suspected of being hyaluronic acid, the infiltration can be with hyaluronidase.5 In more refractory cases, oral corticosteroid regimens can be used. Nevertheless, in the long term, these treatments can lead to unaesthetic adverse effects, such as skin atrophy.1,2
Given the similarity between foreign-body granulomas and sarcoid granuloma,6 Reisberger et al.4 prescribed allopurinol (200mg/d, increasing gradually to 600mg/d). Subsequent studies revealed improvements in granulomatous reactions to silicone3 and tattoo materials.7,8 In these cases, daily doses range from 300 mg3,7 to 600mg.8 Oral allopurinol can be combined with infiltrations of 5-fluorouracil and triamcinolone acetonide.5
Allopurinol has been associated with downregulation of intracellular adhesion molecule 1 and P2X7, which are receptors of the monocyte and macrophage lineages. The reduction in intracellular adhesion molecule interferes with cellular adhesion, and P2X7 receptors have been associated with the cell fusion process leading to multinucleated giant cells during granulomatous inflammation.8
A review of the literature shows that the more superficial material (eosinophilic, with no associated reaction) could correspond to substances such as silicone, paraffin, or polymethyl methacrylate microspheres. Polymethyl methacrylate seems to be the most likely option, since the remaining products usually produce cystic/lanceolate areas in histopathology, with a very characteristic pattern. In morphological terms, the deeper material (basophilic with an associated inflammatory reaction) could correspond to polyacrylamide hydrogel, polyalkylimide gel, polyvinyl hydroxide microspheres in polyacrylamide gel, alginate reticulation, or hyaluronic acid. Given that the patient had undergone surgery several years previously, we can rule out hyaluronic acid, with a permanent filler seeming more likely. Polyacrylamide gel is more multivacuolated in appearance, whereas polyalkylimide is more granular; therefore, the substance involved in the present case could be polyalkylamide.5,9
In conclusion, we present a case of foreign-body granulomatous reaction with a good response to daily allopurinol 300mg. This treatment could be a useful alternative in patients who do not respond to conventional therapy.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: González-Delgado VA, Cordero Romero P, Terrádez-Mas L, Martín JM. Respuesta favorable al tratamiento con alopurinol de reacción granulomatosa a relleno. Actas Dermosifiliogr. 2020;111:439–441.