A 51-year-old woman, with no relevant past medical history, presented with a 1-month history of pruritic, evanescent wheal-like skin lesions on her trunk and extremities (Fig. 1), along with erythematous, pruritic papular lesions on the elbows and arms (Fig. 2). She also reported episodes of evening fever of up to 39°C over the past month, along with odynophagia, severe fatigue, and arthralgia in the ankles, knees, and wrists. These episodes were associated with worsening skin lesions. Physical examination confirmed the presence of left lateral cervical lymphadenopathy.
Blood test showed normocytic normochromic anemia, a mild elevation of transaminases and C-reactive protein (CRP), marked elevation of lactate dehydrogenase (LDH), and ferritin levels more than 5 times above normal range. Viral serologies (hepatitis B and C, cytomegalovirus, and Epstein-Barr virus) and an autoimmunity profile all tested negative. Protein electrophoresis and immunoglobulin levels were normal.
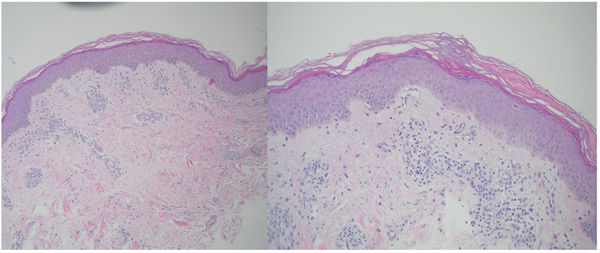
Biopsy of a wheal-like lesion revealed the presence of an interstitial lymphocytic infiltrate in the dermis with vascular dilation and edema, but no vasculitis whatsoever. Biopsy of papular lesions showed areas of parakeratosis, dyskeratotic keratinocytes on the superficial epidermis, and a perivascular mononuclear dermal infiltrate (Fig. 3).
What is your diagnosis?
DiagnosisAdult-onset Still's disease.
The patient was diagnosed with adult-onset Still's disease with atypical skin signs. She met two major diagnostic criteria from the Yamaguchi classification (>1-week history of intermittent fever >39°C and >2-week history of arthralgia) and 5 minor criteria (odynophagia, lymphadenopathy, liver dysfunction, and negative rheumatoid factor/antinuclear antibodies). Therefore, she met the required 5 criteria, with, at least, 2 being major criteria, for a definitive diagnosis. Treatment with prednisone at 60mg/day in a tapering regimen and bilastine 20mg/3 tablets daily led to significant clinical improvement and resolution of the skin lesions.
Adult-onset Still's disease is a systemic inflammatory disorder characterized by spiking fevers, arthritis, skin rash, and hyperferritinemia.1 Its incidence is rare, with 0.1–0.4 cases being reported per 100,000 population in Europe. Furthermore, its etiology remains unknown.2
Clinical presentation is defined by transient spiking fevers, predominantly in the evening, seen in 93% up to 100% of the cases. These are usually accompanied by arthritis or arthralgia, with symmetric, migratory involvement of both upper and lower limb joints.1,2 Dermatologic signs typically include a salmon-pink rash on the trunk and proximal limbs, consistent with febrile spikes and showing a positive Koebner phenomenon.2 However, atypical skin signs – such as persistent erythematous papules and plaques, linear hyperpigmentation, urticarial-like lesions, prurigo pigmentosa-like lesions, and lichenoid plaques – have been reported as well.3,4 Other signs and symptoms include lymphadenopathy, odynophagia, splenomegaly, abdominal pain, and pleuritis or pericarditis.
Marked hyperferritinemia, up to 5 times the normal value, is characteristic, although no specific laboratory or histopathological findings are pathognomonic for diagnosis. Diagnosis is primarily clinical, based on proposed classification criteria by Cush JJ, Yamaguchi M, and Fautrel B.5
Histologically, atypical papular lesions in adult-onset Still's disease characteristically exhibit parakeratosis and dyskeratotic keratinocytes on the superficial epidermis, as seen in this patient.3,4
Treatment is empirical and based on the use of immunosuppressants. Corticosteroids are the first-line therapy, administered at high doses for, at least, 4–6 weeks. Maintenance therapy may involve immunosuppressive agents such as methotrexate, cyclosporine, and hydroxychloroquine, with good outcomes. For refractory or severe cases with life-threatening complications, biologics such as anakinra (anti-IL-1), tocilizumab (anti-IL-6), and TNF inhibitors (infliximab, etanercept, adalimumab) have proven beneficial.5