Systemic inflammation in psoriasis cause metabolic syndrome and cardiovascular disease (CVD), with insulin resistance (IR) as a possible pathogenetic factor1–3.
Our working group performed a cross-sectional study to determine the prevalence of IR by homeostasis model assessment (HOMA-IR) in moderate-severe psoriasis patients attended in our Dermatology outpatient clinic. HOMA-IR was calculated in all participants by measuring fasting plasma glucose and insulin levels using the score (Fasting insulin [mIU/L])*(Fasting glucose [mg/dL])/405, and IR was defined as an elevated HOMA-IR (>2.5), based on the original HOMA research5.
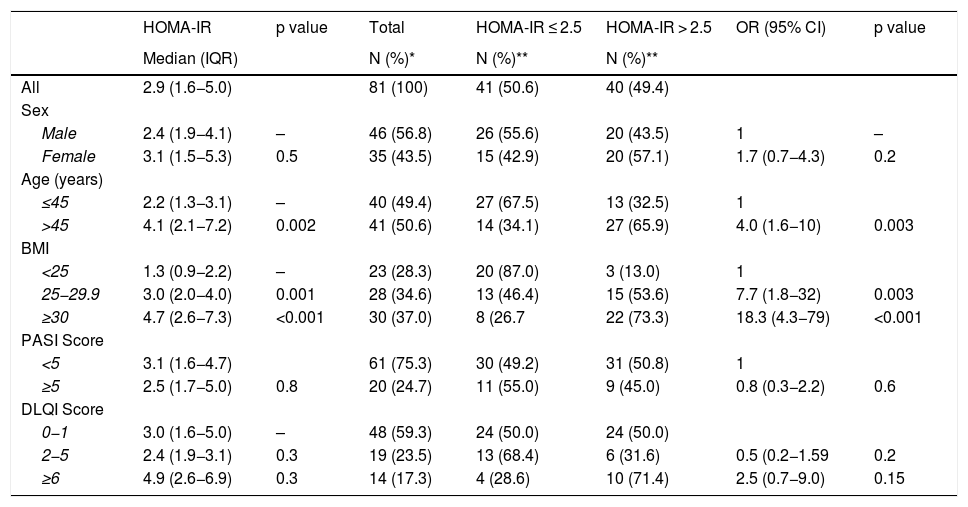
Our initial sample consisted of 100 patients. We excluded 19 patients with diabetes, leaving a sample of 81 participants (46 men and 35 women) with a median of age of 46 years (interquartile range [IQR] 35–56]. Median body mass index (BMI) was 28 kg/m2 (IQR 24.5–31.6). Median HOMA-IR was 2.9 (IQR 1.6−5.0) and 49.4% of patients had IR (95% confidence interval [CI] 38.6%–60.0%). Table 1 shows the demographic and clinical characteristics of patients by HOMA-IR score.
Demographic and clinical characteristics of patients with psoriasis by homeostasis model assessment-insulin residence (HOMA-IR).
| HOMA-IR | p value | Total | HOMA-IR ≤ 2.5 | HOMA-IR > 2.5 | OR (95% CI) | p value | |
|---|---|---|---|---|---|---|---|
| Median (IQR) | N (%)* | N (%)** | N (%)** | ||||
| All | 2.9 (1.6−5.0) | 81 (100) | 41 (50.6) | 40 (49.4) | |||
| Sex | |||||||
| Male | 2.4 (1.9−4.1) | – | 46 (56.8) | 26 (55.6) | 20 (43.5) | 1 | – |
| Female | 3.1 (1.5−5.3) | 0.5 | 35 (43.5) | 15 (42.9) | 20 (57.1) | 1.7 (0.7−4.3) | 0.2 |
| Age (years) | |||||||
| ≤45 | 2.2 (1.3−3.1) | – | 40 (49.4) | 27 (67.5) | 13 (32.5) | 1 | |
| >45 | 4.1 (2.1−7.2) | 0.002 | 41 (50.6) | 14 (34.1) | 27 (65.9) | 4.0 (1.6−10) | 0.003 |
| BMI | |||||||
| <25 | 1.3 (0.9−2.2) | – | 23 (28.3) | 20 (87.0) | 3 (13.0) | 1 | |
| 25−29.9 | 3.0 (2.0−4.0) | 0.001 | 28 (34.6) | 13 (46.4) | 15 (53.6) | 7.7 (1.8−32) | 0.003 |
| ≥30 | 4.7 (2.6−7.3) | <0.001 | 30 (37.0) | 8 (26.7 | 22 (73.3) | 18.3 (4.3−79) | <0.001 |
| PASI Score | |||||||
| <5 | 3.1 (1.6−4.7) | 61 (75.3) | 30 (49.2) | 31 (50.8) | 1 | ||
| ≥5 | 2.5 (1.7−5.0) | 0.8 | 20 (24.7) | 11 (55.0) | 9 (45.0) | 0.8 (0.3−2.2) | 0.6 |
| DLQI Score | |||||||
| 0−1 | 3.0 (1.6−5.0) | – | 48 (59.3) | 24 (50.0) | 24 (50.0) | ||
| 2−5 | 2.4 (1.9−3.1) | 0.3 | 19 (23.5) | 13 (68.4) | 6 (31.6) | 0.5 (0.2−1.59 | 0.2 |
| ≥6 | 4.9 (2.6−6.9) | 0.3 | 14 (17.3) | 4 (28.6) | 10 (71.4) | 2.5 (0.7−9.0) | 0.15 |
BMI: body mass index; CI: confidence interval; DLQI: dermatology life quality index; OR: odds ratio; PASI: psoriasis area and severity index.
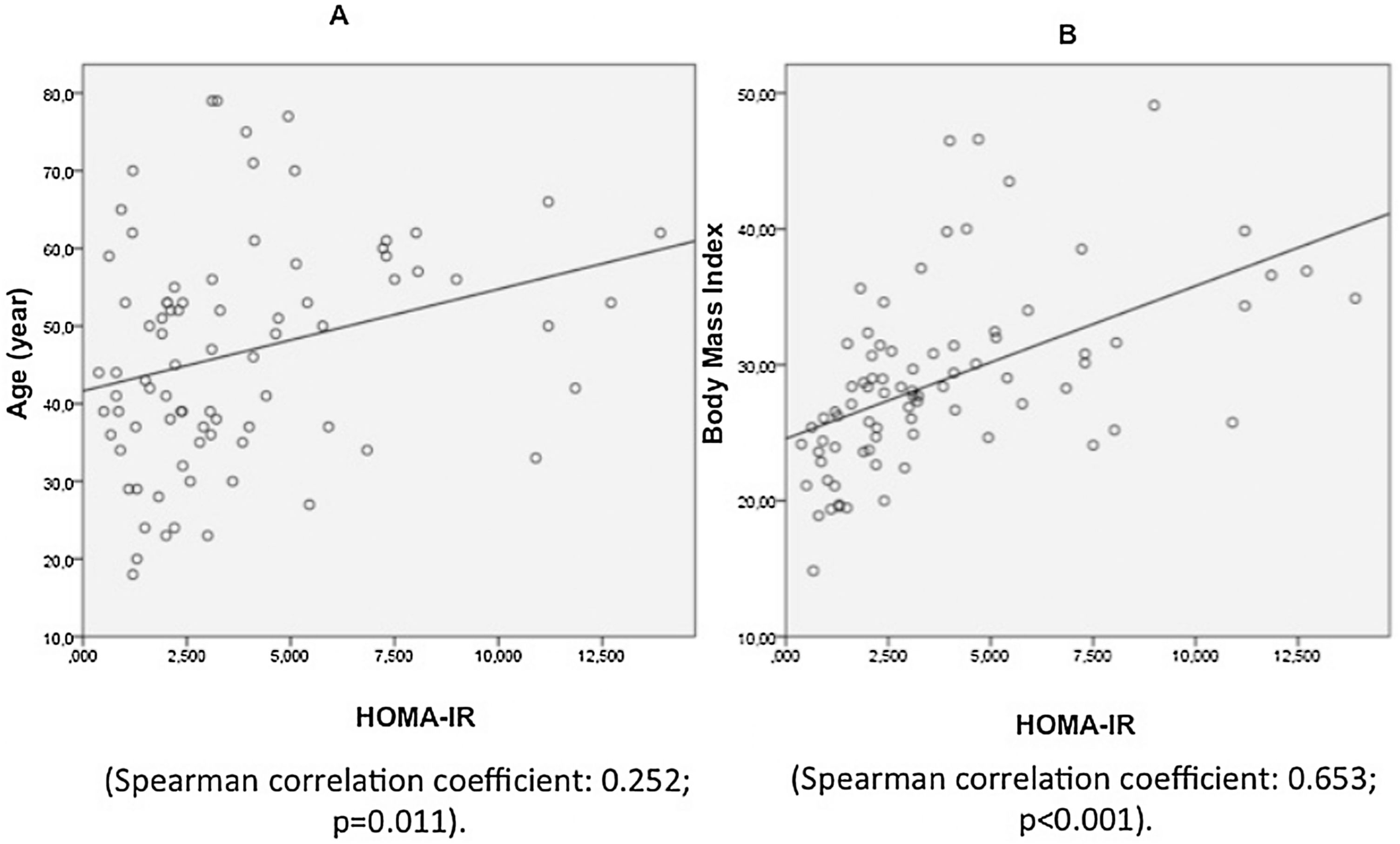
In patients aged more than 45 years, median HOMA-IR was significantly higher than in those aged 45 years or younger (p = 0.002), indicating a correlation between age and HOMA-IR. The prevalence of IR in patients aged over 45 years was 65.9% (odds ratio [OR] 4.0, 95% CI 1.6–10; p = 0.003). BMI was also correlated with higher median HOMA-IR (1.3 in patients with normal weight [BMI < 25 kg/m2], 3.0 in patients who were overweight [BMI 25−29.9 kg/m2], and 4.7 in patients with obesity [BMI ≥ 30 kg/m2]; p = 0.001; Fig. 1). The prevalence of IR > 2.5 was 13.0% in patients with normal weight, 53.6% in patients who were overweight (p < 0.003), and 73.3% in patients with obesity (p < 0.001). It is interesting to note that the values of HOMA-IR were not associated with sex, psoriasis area and severity index (PASI), or the dermatology life quality index (DLQI) (Table 1).
IR represents the best predictor of type 2 diabetes mellitus, and it plays a central role in the high cardiovascular risk associated with metabolic syndrome4. In our study population with moderate-to-severe psoriasis the prevalence of IR was high, almost half of the patients (49,4%). Although our study did not have a control group, the overall IR prevalence is much higher than reported in a similar population-based study (approx. 9%)4. We have detected a clear relationship between the IR and the BMI, as shown in Fig. 1. Similarly, Boehncke et al. observed a clear relationship between high BMI and IR3. Interestingly, the values of the HOMA-IR index were not related to the severity of psoriasis defined by PASI in our patients, which contrast with those reported previously, who did detect a significant correlation between PASI and insulin secretion3.
A substantial proportion of psoriasis patients, particularly those with high BMI, will have IR. We would like to emphasize that dermatologists must assume responsibility for preventing, promptly detecting, treating, and caring for those psoriasis patients with subclinical IR and therefore at risk for diabetes and CVD. Hence the HOMA-IR score can help clinicians to achieve it in a simple way.
Please cite this article as: Romero-Pérez D, Belinchón Romero I, Ramos Rincón JM. Índice de evaluación del modelo de homeostasis (HOMA) y resistencia a la insulina en la psoriasis. Actas Dermosifiliogr. 2021;112:867–868.