Infantile hemangioma (IH) is 1 of the most common benign tumors of childhood, with an incidence of between 4% and 10%.1 The majority of IHs appear in the first week of life, although they can sometimes be observed at birth.
Some IHs arise in areas that affect the airway or vision and some ulcerate or progress to leave significant sequelae; in these situations, treatment is required. Since the first report by Léauté-Labrèze et al.2 in 2008, β-blockers have become first-line treatment. A study comparing propranolol with placebo for the treatment of IH was published recently and demonstrated the efficacy of a dose of 3mg/kg/d and the low rate of recurrences that required reintroduction of the treatment (10%).3
A key concept in the management of IH is when to start treatment. The recommendation is to initiate treatment at the start of the growth phase. However, delayed consultation is not an impediment to prescription, though the anticipated response rate will be noticeably lower.
The 3 main β-blocker drugs available for the treatment of IH are propranolol, nadolol, and timolol.
Propranolol was the first β-blocker used to treat IH. Although topical formulations (1% cream or ointment) are available, the oral preparations are preferred. Propranolol solution, 3.75mg/ml, has recently become available. The recommended initial dosage is 1mg/kg/d, divided into 2 doses of 0.5mg/kg. The highest efficacy and best tolerance were achieved with a dosage of 3mg/kg/d for 6 months. The dosage can be increased by 1mg/kg each week to reach 3mg/kg/d, except in PHACES (posterior fossa malformations, hemangiomas, arterial anomalies, cardiac defects, eye abnormalities, sternal cleft, and supraumbilical raphe) syndrome, in which the dosage is increased by 0.5mg/kg each week. Patient monitoring (whether in the hospital environment or in the community) is recommended for the first 2hours after administering the drug, performing clinical observation and heart rate monitoring, although protocols vary between centers. If the heart rate or blood pressure are below predetermined limits in 2 successive controls, treatment must be discontinued. It is advisable to administer the treatment immediately after feeding to avoid the risk of hypoglycemia.
In patients who present sleep disorders (agitation, insomnia) or nightmares during treatment with propranolol, nadolol should be used in its place as it does not cross the blood-brain barrier. Nadolol is available as an oral solution, 10mg/ml, and is administered at an initial dosage of 0.5 to 1mg/kg/d divided into 2 daily doses. The dosage can be increased by 0.5mg/kg per week to a maximum of 2mg/kg/d. Nadolol and propanolol have shown similar efficacy in the treatment of IH.4
Timolol maleate is an interesting alternative in patients with periocular or superficial IH. In daily clinical practice it is preferred for its availability, and it is widely used as a 0.25% or 0.5% solution applied twice daily. This drug can be used in patients under 1 month of age. When a good response is achieved, treatment should be continued for a month after observing complete regression. Treatment can be reintroduced if the IH reappears, but the response rate is variable. The majority of published cases are of superficial periocular lesions.
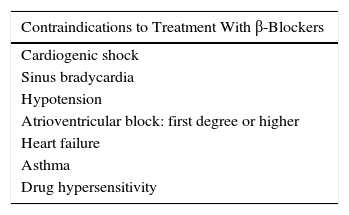
Adverse effects during treatment with β-blockers must be taken into account. These include vasospasm, hypoglycemia, hypotension, heart block, bronchospasm, and anaphylactic shock.5 Contraindications to the use of β-blockers are listed in Table 1.
In conclusion, β-blockers have revolutionized the management of IH, and knowledge of their efficacy and safety has now become not just necessary, but absolutely obligatory for the dermatologist.
Please cite this article as: Navarro-Triviño FJ. FR. Hemangiomas infantiles y β-bloqueantes. Cuándo, cómo y por qué. Actas Dermosifiliogr. 2016;107:601–602.