Eczema is an inflammatory skin reaction that can have different etiologies. It is characterized clinically by pruritus and polymorphous skin lesions that can progress successively through erythema, macules, papules, edema, vesicles or blisters, excoriation, erosions, scabs, flaking, hyperkeratosis, lichenification, and fissures.1 Histologically it is characterized by spongiosis; other findings include acanthosis, parakeratosis, and a lymphocytic perivascular infiltrate in the upper dermis that may show epidermotropism and that includes a variable number of eosinophils.2
Contact eczema develops when the skin surface comes into contact with an exogenous substance. Irritant contact eczema (ICE) accounts for 80% of cases and is due to a local toxic effect caused by single or repeated contact with irritant substances. It is limited to the area of exposure in the majority of cases. ICE most commonly affects hands (80%) and face (10%).3,4 Allergic contact eczema (ACE) accounts for the remaining 20%. This is a delayed hypersensitivity reaction triggered by contact with a substance to which the patient has previously become sensitized. ACE develops in the area of exposure and occasionally also at distant sites.5 The clinical manifestations can be similar in the 2 forms of contact eczema, and a detailed medical history and physical examination are therefore essential in the search for the main risk factors.1,3–9
In the literature, we have found no descriptions of a protocol for the initial clinical evaluation of this type of patient. The German clinical guideline for hand eczema proposes a detailed medical history and meticulous physical examination (grade A recommendation), paying particular attention to the site and morphology of the skin lesions.6 We therefore present our standard approach to the first consultation in the Eczema Unit of Hospital 12 de Octubre in Madrid, Spain:
- a)
Individual characteristics of the eczema1,3–9: initial site, disease duration, symptoms (pruritus, pain, soreness), clinical behavior and extension, clinical course (persistent or intermittent), exacerbations and remissions, previous episodes of eczema, aggravating factors, seasonal variations, previous treatments, and relationship with weekends, holidays, periods off work, and exposure to sunlight.
- b)
Predisposing factors:
- –
Age and sex: ICE is more common in women, children, and the elderly.3,4,7
- –
Past history of allergy and supporting additional tests.7
- –
A personal or family history of atopic dermatitis, asthma, or allergic rhinoconjunctivitis is associated with a higher risk of ICE.3,4,7
- –
Past history of other dermatoses: Seborrheic dermatitis is associated with an increase in the levels of the proinflammatory cytokine interleukin-1α, leading to a higher risk of ICE.3
- –
Genetic factors: Polymorphism of tumor necrosis factor-308 and mutations of the filaggrin gene probably constitute a risk factor for ICE.7
- –
- c)
Factors related to exposure:
- –
Past and present occupational and domestic exposure (Table 1)1,3–5: Determine the use of personal protection measures, such as gloves, goggles, face masks, and protective clothing.
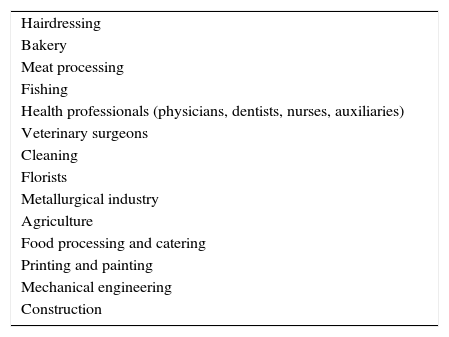
Table 1.Occupations Most Commonly Associated With Contact Eczema.
Hairdressing Bakery Meat processing Fishing Health professionals (physicians, dentists, nurses, auxiliaries) Veterinary surgeons Cleaning Florists Metallurgical industry Agriculture Food processing and catering Printing and painting Mechanical engineering Construction - –
Exposure to irritant substances (Table 2).3,4
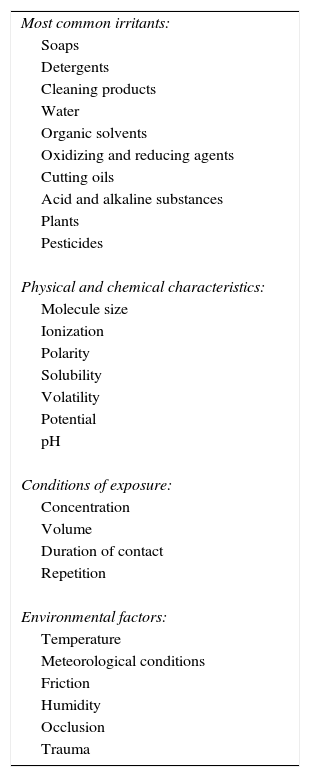
Table 2.The Characteristics of Irritant Substances.
Most common irritants: Soaps Detergents Cleaning products Water Organic solvents Oxidizing and reducing agents Cutting oils Acid and alkaline substances Plants Pesticides Physical and chemical characteristics: Molecule size Ionization Polarity Solubility Volatility Potential pH Conditions of exposure: Concentration Volume Duration of contact Repetition Environmental factors: Temperature Meteorological conditions Friction Humidity Occlusion Trauma - –
Work in a moist environment: This is defined as exposure to water for more than 2hours a day, hand washing more than 20 times a day, or the use of gloves for more than 2hours a day.
- –
Leisure activities and hobbies.
- –
Use of skincare products, perfumes, cosmetics, metals, topical medicines.
- –
We also present our standard procedure for complete physical examination:
- –
Description of the eczematous lesions1,3–6,9: site, pattern (acute, subacute, chronic), distribution (single, patchy, linear, diffuse, disseminated), morphology, intensity, size, palpation, ulceration, scabs, signs of superinfection, hyperkeratosis, and lichenification.
- –
Complete dermatologic examination, including scalp, intertriginous areas, palms, soles, and nails.
- –
Thorough inspection for clinical signs of dermatophytosis, psoriasis, and atopy (Table 3).1,3–5,10
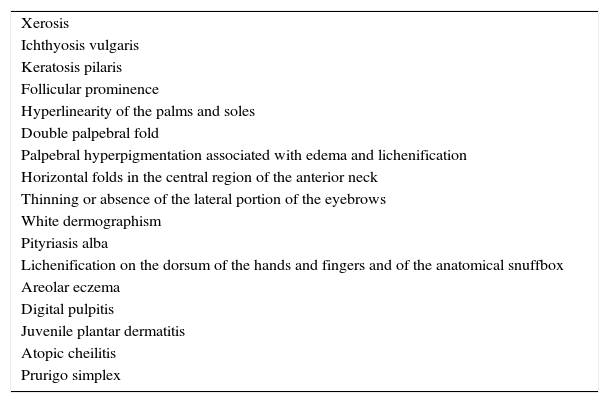
Table 3.Signs of Atopy.
Xerosis Ichthyosis vulgaris Keratosis pilaris Follicular prominence Hyperlinearity of the palms and soles Double palpebral fold Palpebral hyperpigmentation associated with edema and lichenification Horizontal folds in the central region of the anterior neck Thinning or absence of the lateral portion of the eyebrows White dermographism Pityriasis alba Lichenification on the dorsum of the hands and fingers and of the anatomical snuffbox Areolar eczema Digital pulpitis Juvenile plantar dermatitis Atopic cheilitis Prurigo simplex
A number of differential diagnoses must be considered in patients with a pruritic erythematous skin rash with eczematous lesions, including seborrheic dermatitis, atopic dermatitis, psoriasis, erythematous rosacea, asteatotic eczema, dyshidrotic eczema, dermatitis herpetiformis, lichen simplex, dermatophytosis, scabies, and mycosis fungoides.1–5
The information obtained can help to guide the choice of diagnostic procedures required, such as patch tests, prick tests, culture, and skin biopsy.1–9 In conclusion, the aim of this article has been to present the initial clinical evaluation guideline used in our center in the hope that it will help dermatologists in their evaluation of patients with contact eczema. The medical history and dermatologic examination will orient the diagnosis and the search for the etiology, will establish the relevant additional tests, and will facilitate patient education. The German guideline recommends secondary prevention measures in high-risk groups through avoidance of exposure to known irritants and allergens by the use of appropriate skin protection (level B evidence).6 Finally, the role of the dermatologist is essential in the identification of high-risk patients and the adoption of appropriate primary and secondary measures of prevention.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Imbernón-Moya A, Ortiz-de Frutos FJ, Delgado-Márquez AM, Vanaclocha-Sebastián F. Valoración inicial del paciente con eczema de contacto. Actas Dermosifiliogr. 2016;107:791–793.