A 56 years old Caucasian man presented to our Dermatology consultation with a slow-growing solitary skin lesion on the abdomen of 3-4 months of evolution, accompanied of slight burning sensation. He had a medical history of hypertension, chronic kidney disease and secondary hyperparathyroidism, that had undergone kidney transplantation 5 months before. He was being treated with tacrolimus, mycophenolate mofetil, prednisolone, nifedipine, carvedilol and cotrimoxazole.
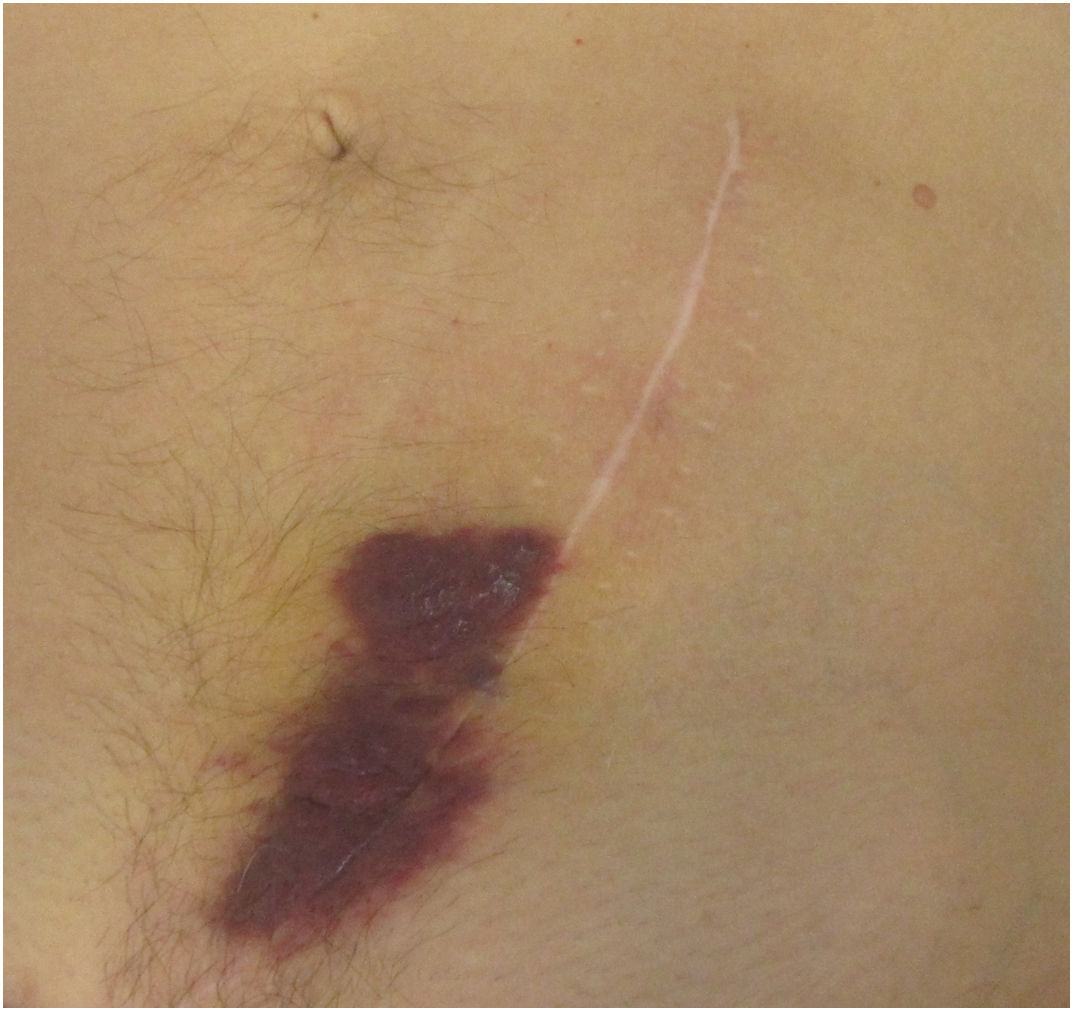
Clinical examination revealed a 20 cm large purple plaque located at the inferior extremity of the abdominal surgical scar with no other skin or mucosal lesions (Fig. 1).
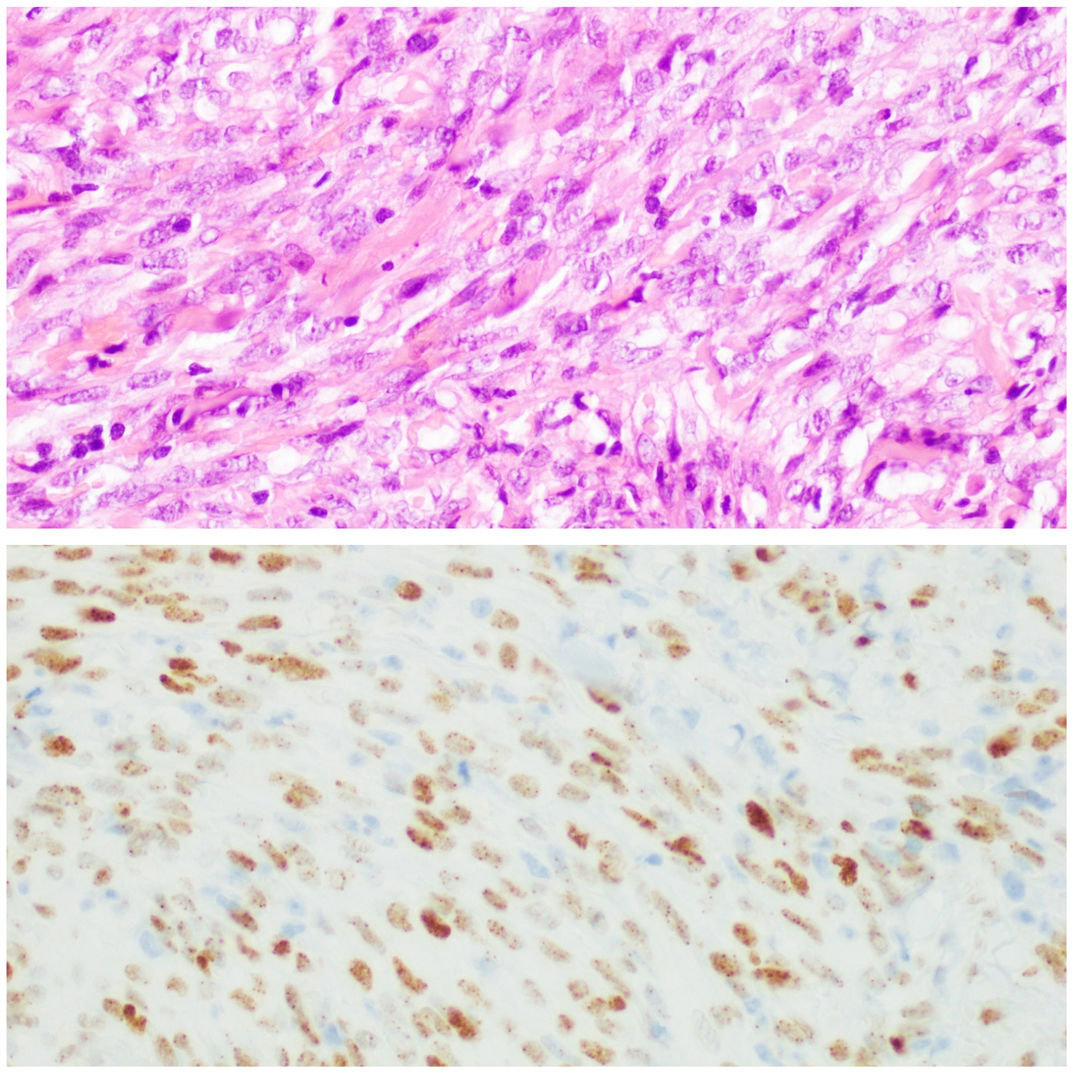
A punch biopsy demonstrated dermal proliferation of spindle shaped cells with mild cytologic atypia, which formed slit-like channels and stained positive for human herpesvirus 8. These features are characteristic of Kaposi sarcoma in plaque/nodular stage (Fig. 2).
After the diagnosis of Kaposi sarcoma, tacrolimus was replaced by everolimus and he was referred to the Oncology department, to proceed with exclusion of extra-cutaneous manifestations, that proved to be negative.
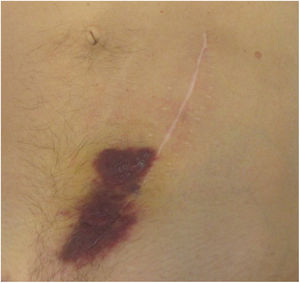
Gradually the skin plaque on the patient scar disappeared and was replaced by an hyperpigmented brown patch (Fig. 3).
Kaposi sarcoma (KS) is an angioproliferative disorder that is associated with infection with human herpes virus 8 (HHV-8).1
Iatrogenic, immunosuppressive drug-associated KS is frequent among renal transplant recipients, accounting for < 3-4% of all neoplasms.2
The incidence of KS among solid organ transplant recipients is 500 times greater as compared with the general population’s, suggesting a role for immunosuppression in the development of the disease.3 Iatrogenic Kaposi sarcoma presents mainly with cutaneous manifestations.3,4
A presentation of Kaposi sarcoma, de novo, in a scar is extremely rare, and this location can be explained by the Koebner’s phenomenon. The Koebner phenomenon is the localization of skin disease to a site of trauma in an individual who is susceptible to that disease.5 A key role has been suggested for basic fibroblast growth factor (b-FGF), a mitogen for endothelial cells and keratinocytes. Trauma, like surgical intervention, to susceptible skin may cause the release of this and other cytokines (interleukin-1, interleukin- 6, tumour necrosis factor-alfa, vascular endothelial growth factor, platelet-derived growth factor, granulocyte–macrophage colony-stimulating factor) triggering angiogenesis. The increased angiogenesis and the reactivation of the HHV-8 would contribute to the development of Kaposi sarcoma.4
The advent of inhibitors of the mammalian target of rapamycin (mTOR inhibitors), such as sirolimus and everolimus, represents an alternative for the antirejection maintenance therapy. Furthermore, they can have a role in the treatment of Kaposi’s sarcoma, since they also decrease the production of VEGF and inhibit the response of vascular endothelial cells to stimulation by VEGF. Therefore, mTOR inhibitors, not only inhibit the growth of certain vascularized tumors, while maintaining a lower risk of losing the renal graft.6
In the present case the patient presented only with a cutaneous lesion due to Kaposi Sarcoma, that resolved with the switch from tacrolimus to everolimus. This fact supports that mTOR inhibitors represent an alternative that allows the preservation of the renal graft, while treating Kaposi sarcoma.
Please cite this article as: Santos Silva LF, Miroux Catarino A, Sordo Amaro C, Faro Viana I. Sarcoma de Kaposi, de novo, en una cicatriz quirúrgica de transplante de riñón. Actas Dermosifiliogr. 2021;112:671–672.