A 51-year-old male with a past medical history of hypertension, bronchial asthma, and allergies to aspirin and amoxicillin presented to the Dermatology ER with a 1-h history of a pruritic skin rash, which started 1 day after beginning treatment with cefuroxime 250mg/12h for cystitis. During his stay in the ER, the patient developed oppressive chest pain along with autonomic symptoms.
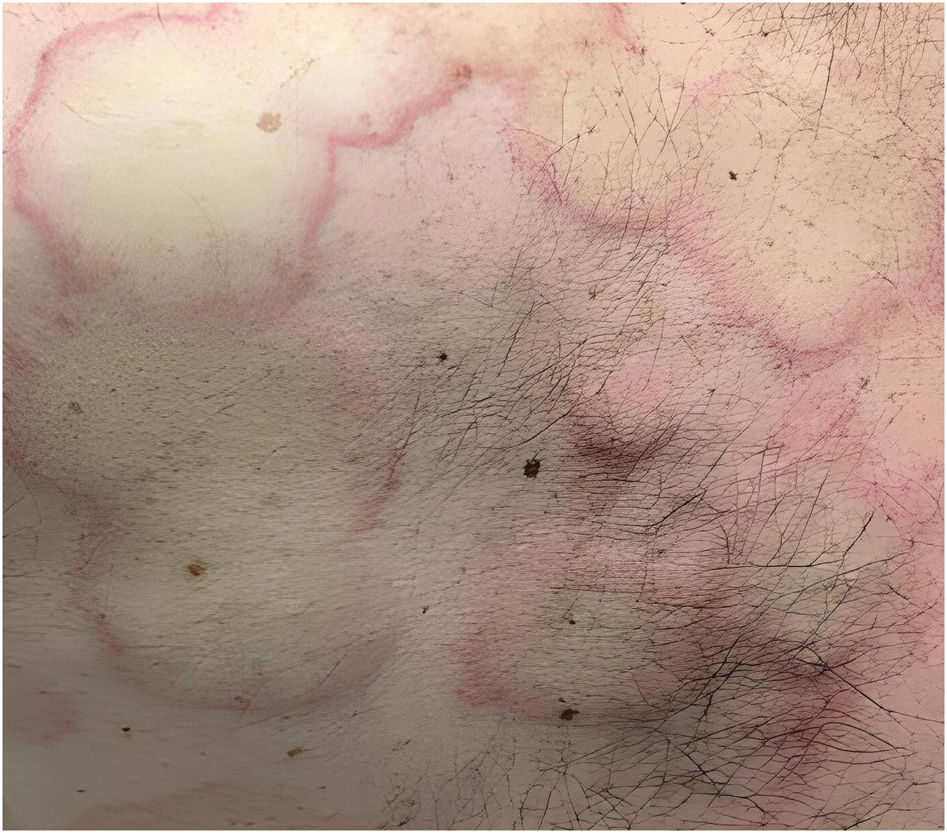
Physical examinationThe physical examination revealed the presence of erythematous–edematous plaques with a pale yellow center and hyperemic periphery of axial (Fig. 1) and limb distribution, along with bilateral eyelid edema (Fig. 2).
Supplementary testsThe electrocardiogram (ECG) revealed negative T waves in leads II, III, and aVF. The coronary computed tomography angiography of the chest ruled out pulmonary embolism, and the high-sensitivity troponin T myocardial injury marker was normal.
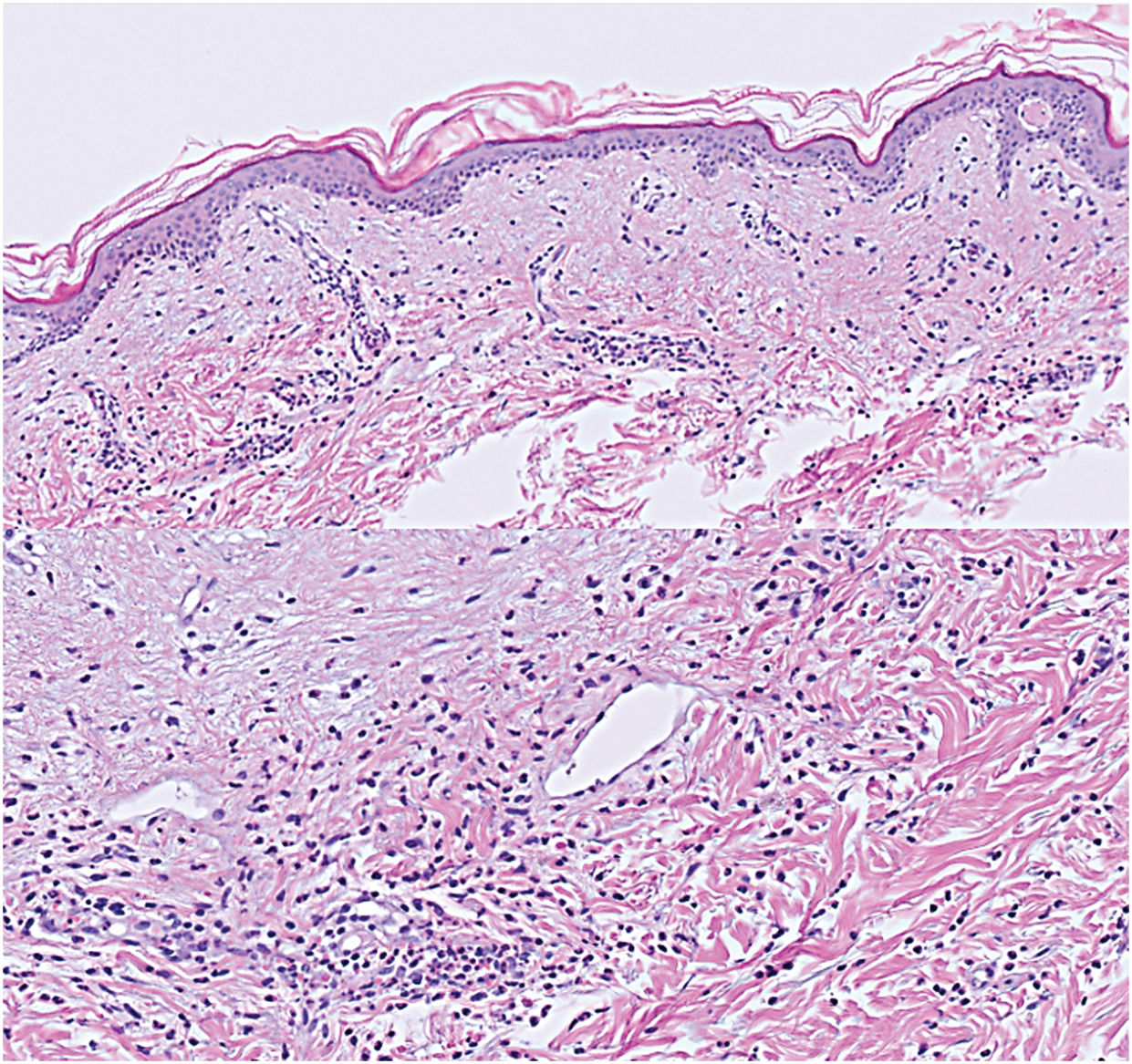
HistopathologyAn incisional biopsy of one of the plaques revealed the presence of perivascular infiltrate including lymphocytes and neutrophils, as well as edema in the papillary dermis, which were findings consistent with acute urticaria (Fig. 3).
What is your diagnosis?
Kounis syndrome type I.
Disease progression and treatmentIV methylprednisolone and dexchlorpheniramine were administered, which resulted in the resolution of chest pain and normalization of the ECG changes. The patient was discharged with a tapering course of oral prednisone 30mg and loratadine 10mg/12h. He was referred to Cardiology for coronary evaluation and to Allergy for beta-lactam allergy testing. Unfortunately, the patient did not attend the recommended follow-up appointments.
CommentKounis syndrome (KS) is a myocardial ischemia-related phenomenon triggered by allergic or anaphylactic stimuli. The three main variants of this syndrome are allergic vasospastic angina (KS type I), allergic myocardial infarction (KS type II), and previous stent thrombosis (KS type III). Of these, KS type I is the most common one, accounting for more than 70% of the cases.1,2
KS is more prevalent in men aged 40–70 with a past medical history of allergies and cardiovascular risk factors.1 Our patient's profile matches the typical KS epidemiology: 51 years old, asthmatic, allergic to beta-lactams, and hypertensive.
The pathophysiology of KS is based on mast cell and platelet degranulation induced by the allergenic stimulus.1,2 Mast cells are abundant in cardiac tissue; during an allergic reaction, mast cell degranulation releases substances that induce vasospasm (histamine, chymase, cathepsin-D, leukotrienes) and/or cause plaque erosion and rupture through fibrinogen degradation, which destabilizes it (tryptase, neutral proteases).1,2 Symptoms primarily include cardiac (angina, palpitations), dermatological (hives, angioedema), and respiratory (dyspnea, wheezing) signs.2 The presence of the allergen is necessary to trigger the episode, so once it has been removed, recurrence of skin lesions or other symptoms is not expected in the mid-term.2,3
Antibiotics are the primary triggers of KS. Cephalosporins are the most widely reported drug responsible for KS after penicillins, with cases ranging from cefuroxime-induced coronary spasm to allergic myocardial infarction.3,4
In addition to the supplementary tests performed in this case (electrocardiogram, CCTA, high-sensitivity troponin I, and skin biopsy), serum tryptase and IgE levels are recommended to support a KS diagnosis.2,5 However, these parameters are not available in our center ER.
Regarding treatment, KS type I usually resolves with standard hypersensitivity reaction treatment: systemic corticosteroids and antihistamines.1,2,5 In contrast, KS types II and III require therapies such as those used to treat other acute coronary syndromes, which will be managed specifically by Cardiology.1,2,5 There are specific considerations for managing KS: aspirin can trigger anaphylactoid reactions and exacerbate the condition, while epinephrine may worsen vasospasm-induced events (KS type I).2,5 The utility of the two drugs in KS requires further evidence, and their use should be individualized.2,5
In addition to skin and airways, mast cells may affect other target organs, requiring multidisciplinary intervention in the emergency setting.1,2,5 KS should be considered in any patient who develops chest pain during an allergic reaction, with a thorough review of drug allergy history and recent drug administration.