A 61-year-old woman without any relevant past medical or surgical history presented with a several-year history of a tumor nodule located on her right upper lip. She was asymptomatic but the tumor exhibited progressive growth.
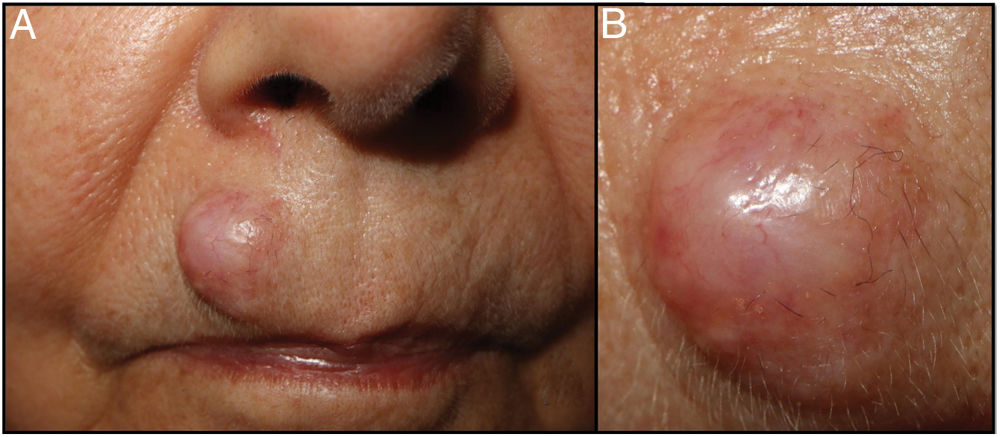
Physical examinationOn examination, an erythematous macule with fine telangiectasias and preserved follicular openings was observed, within which a 20mm subcutaneous nodule was palpable, along with an erythematous hue on the surface, fine telangiectasias, and preserved follicular openings (Fig. 1). The nodule was hard, with an irregular surface, slightly mobile, and adhered to deep planes. The lesion was confined to the skin and spared the oral mucosa. Dermoscopy of the lesion showed the presence of fine sharply focused arborizing vessels on a pink background without any other relevant structures.
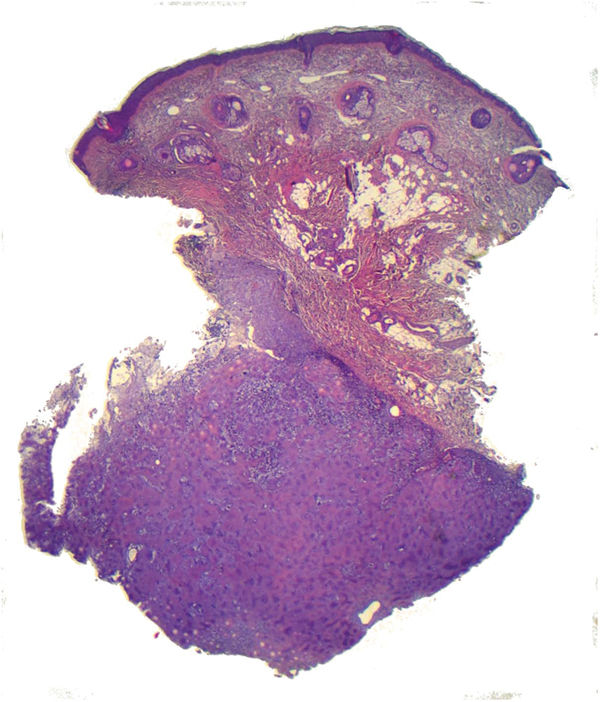
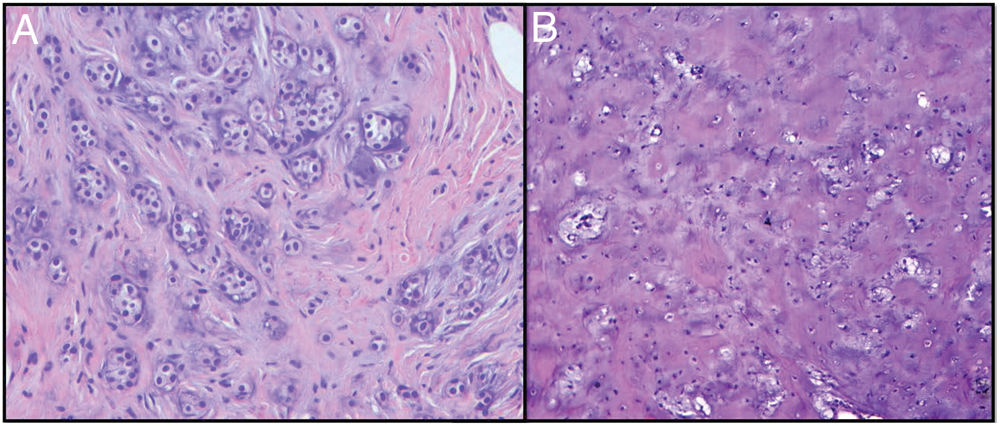
HistopathologyBiopsy of the lesion showed an epidermis of regular thickness with a preserved maturation gradient, beneath which a nodular tumor proliferation was observed in the deep dermis (Fig. 2), with mixed cellularity, consisting of areas of epithelial cells forming ducts lined by a single layer of cuboidal epithelium (Fig. 3A). Cells were positive for cytokeratins (CKAE1-3+) and broad areas of myxoid stroma with chondroid areas were observed (Fig. 3B). The histopathological study revealed few mitoses and no nuclear pleomorphism.
Cutaneous mixed tumor (chondroid syringoma).
CommentAfter diagnosing the lesion—despite its benign nature—complete excision of the lesion was decided due to its size and the functional discomfort reported by the patient. The study of the complete specimen confirmed the findings made on the skin biopsy.
The cutaneous mixed tumor, or chondroid syringoma, is a benign adnexal tumor with follicular and apocrine differentiation, consisting of both an epithelial and a mesenchymal component, hence its name.1,2 Some authors believe it should be considered a hamartoma rather than an adnexal tumor, same as it happens with other neoplasms derived from adnexal structures.2
It is a rare entity and typically presents as a papule or nodule, depending on its size, on the face or neck, although it can grow anywhere, even in the genital region.2,3 Clinically, it can be confused with any other benign adnexal tumor, primarily cystic, infundibular, or trichilemmal, or malignant, such as basal cell carcinoma or sebaceous carcinoma, or even vascular proliferations when they acquire a bluish coloration.
Histologically, its dual origin (epithelial and mesenchymal) translates into the existence of 2 intermingled cellular populations in a nodular, usually dermal, well-circumscribed lesion.2,3 The epithelial component predominantly shows tubular, branched, and interconnected structures covered by 2 cell layers: the luminal one—made of cylindrical cells with decapitation secretion—and the outer one—which is in contact with the stroma—made of cuboidal cells.2 This pattern is known as a mixed tumor with apocrine differentiation, while when made of small, rounded ducts distributed across the stroma, it shows a pattern with eccrine differentiation. Regardless of the differentiation, it is surrounded by a predominant collagen component, which may be accompanied, to varying degrees, by myxoid zones and/or adipocytes.3 Despite the term “chondroid,” the appearance of cartilaginous tissue as part of the stroma is rare.2,3 Given the broad differentiation potential of both components, this lesion may raise diagnostic suspicion with other entities, such as fibromyxoid and ossifying soft tissue tumors, chondrosarcoma myxoid (both lacking ductal/tubular components), and paracordoma (which would be negative for epithelial markers, unlike the cutaneous mixed tumor).
It is a benign tumor, and due to symptoms or the patient's wishes, surgical treatment is ideal.3,4 Given its low recurrence rate, complete excision is recommended, but without the need for safety margins.4
Its indolent behavior is impaired by the existence of malignant forms, usually based on undifferentiated adnexal tumors, which can be associated with local recurrences and even distant metastases.4-6 These are histopathologically characterized by cellular atypia, a high mitotic index, local invasion, and poorly defined lesion borders.4
Additionally, similarities have been established with the mixed tumor of the salivary gland—also known as pleomorphic adenoma. However, this tumor is associated with a higher risk of malignancy and/or local recurrence when excision is incomplete.4 This spectrum of mixed tumors has led to the existence of reports in the literature of “cutaneous” pleomorphic adenoma (true cutaneous mixed tumors and non-cutaneous forms of pleomorphic adenomas of salivary origin),5,6 which underscores the need for analyzing both entities understanding them as 2 separate neoplasms.
Conflicts of interestNone declared.