Lupus erythematosus (LE) rarely affects the genitalia, and few cases have been reported in the literature.1–6 In all types of LE, the skin lesions typically appear in sun-exposed areas. However, involvement of nonexposed areas, such as the scalp, the oral mucosa, or the palms and soles, is common and has been extensively described.1 Genital involvement, on the other hand, is rare and reports in the literature are sparse, for which reason we consider it interesting to report the different genital manifestations observed in 2 patients with LE.
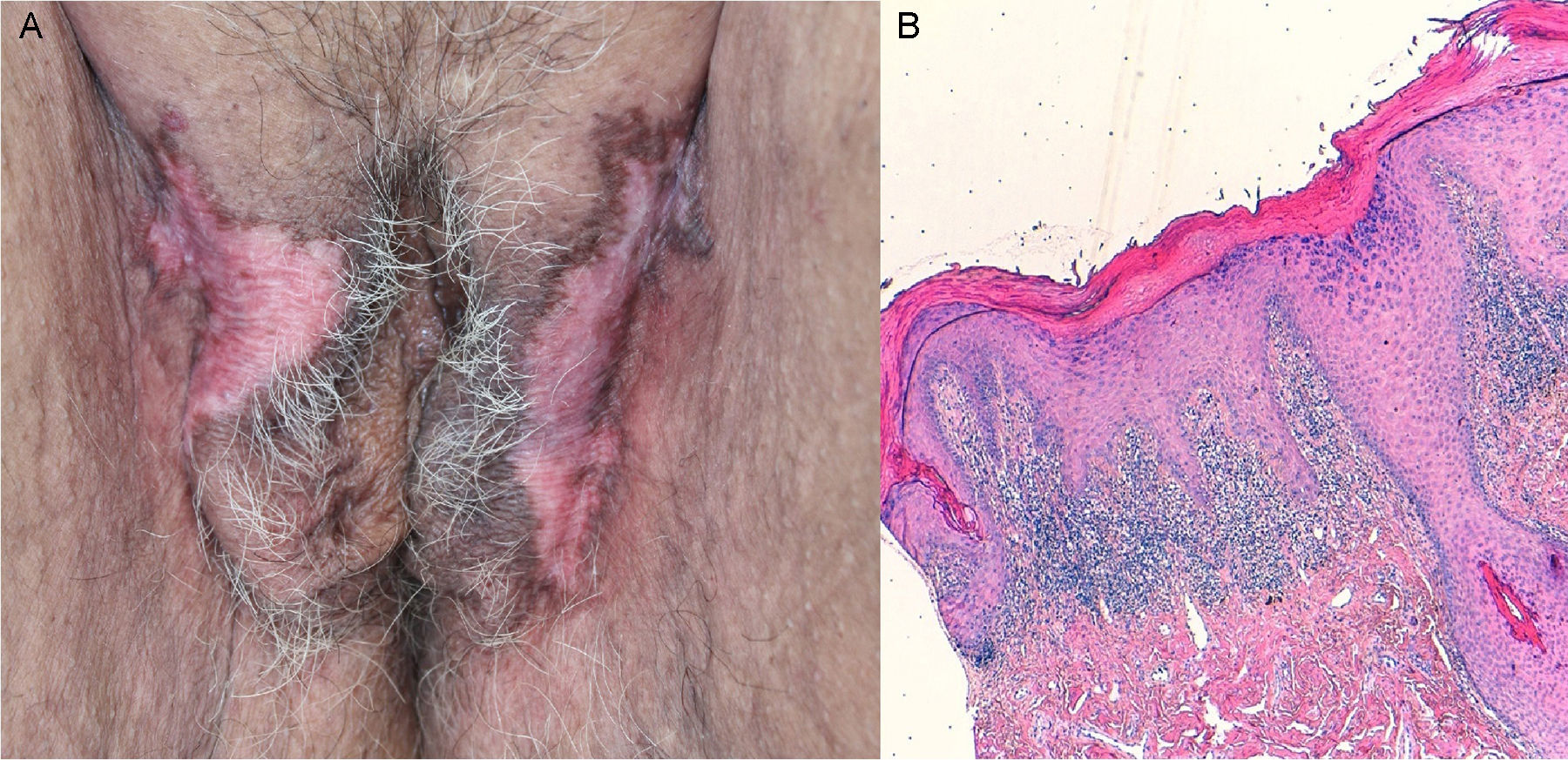
Case 1A 65-year-old woman with a past history of depressive syndrome on treatment with venlafaxine, alprazolam, and lorazepam, was referred from gynecology for asymptomatic skin lesions that had arisen a year earlier on her external genitalia. Whitish, atrophic, alopecic plaques with hyperpigmented borders were observed on the labia majora (Fig. 1A). In addition, examination revealed erythematous edematous plaques on her arms and scarring alopecic on her scalp. A biopsy taken from the genital region showed hyperkeratosis, a lichenoid infiltrate, vacuolar degeneration of the basal layer, and mucin deposits (Fig. 1B). In the blood tests, the antinuclear antibody titer was 1:160, and antiribonucleoprotein antibodies were positive. With a diagnosis of discoid LE (DLE), treatment was started with topical clobetasol for 2 months plus hydroxychloroquine, 400mg/d, for 5 months, leading to an improvement in the edematous plaques on the arms and in the erythema of the alopecia on the scalp, while the genital lesions remained stable. At the time of writing, the patient was taking hydroxychloroquine, 200mg/d, and had no active DLE lesions.
A, Pubic region and labia majora showing whitish, atrophic plaques with scarring alopecia and hyperpigmented borders. B, Hyperkeratosis, a lichenoid infiltrate in the superficial dermis and perifollicular regions, vacuolar degeneration of the basal layer, and apoptotic keratinocytes. Hematoxylin and eosin, original magnification×100.
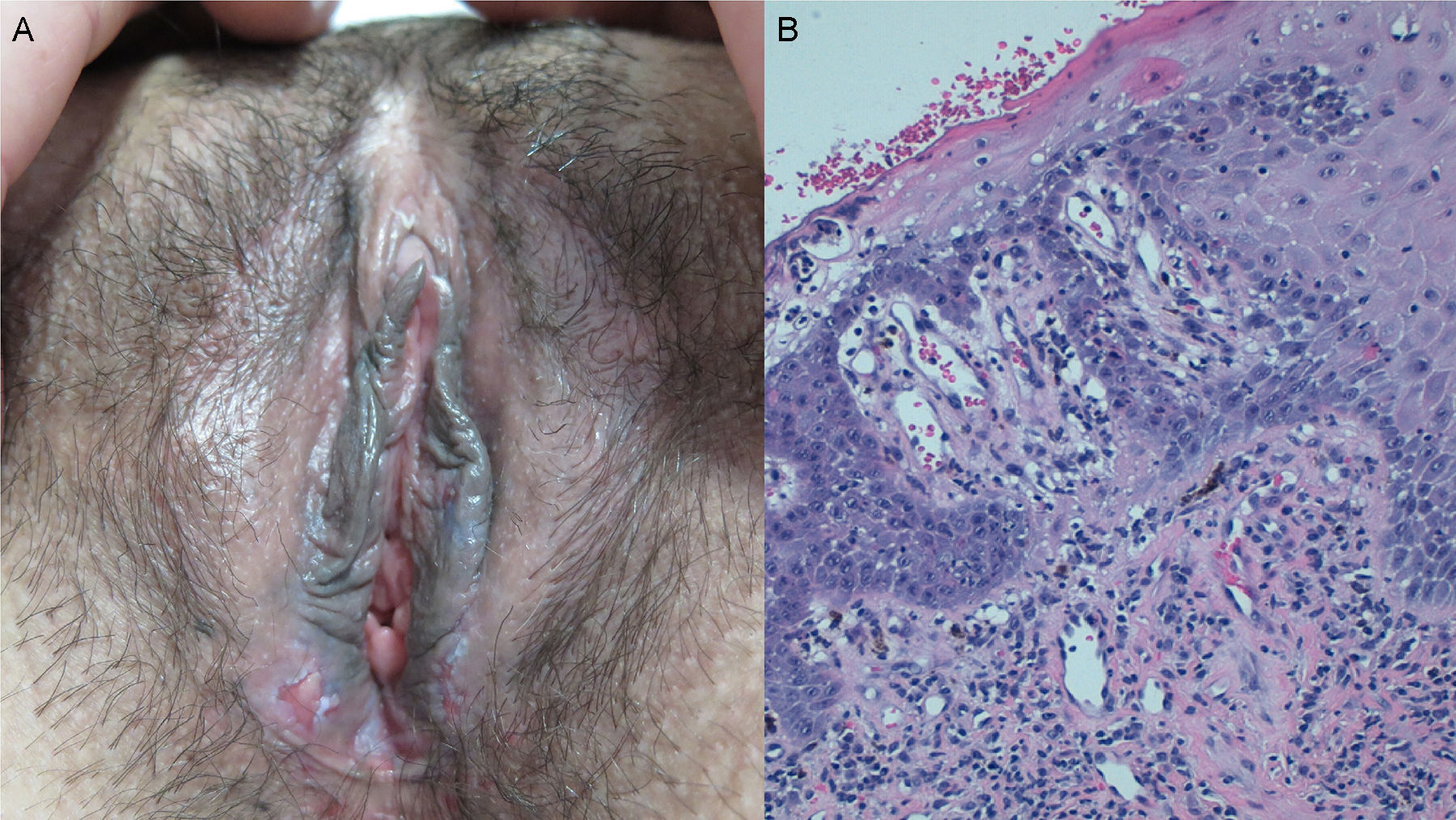
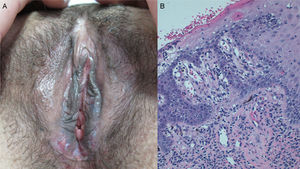
A woman aged 35 years, diagnosed with systemic LE (SLE) 10 years earlier, had presented numerous distinct cutaneous manifestations of SLE and DLE, for which she had received treatment with chloroquine, hydroxychloroquine, methotrexate, thalidomide, and immunoglobulins. She was seen for a 3-month history of painful genital ulcers that appeared to be related to menstruation and lasted for about 10 days. Examination revealed bilateral erosions at the introitus (Fig. 2A), labia minora, and perianal region. Herpesvirus culture was negative and biopsy showed parakeratosis, focal ulceration, and vacuolar degeneration of the basal layer, with apoptotic keratinocytes in the epidermis and a chronic inflammatory infiltrate in the superficial dermis (Fig. 2B), consistent withLE. Topical clobetasol was prescribed for the outbreaks of genital lesions, leading to an improvement in the pain and duration of the ulcers, though they continued to appear intermittently.
A, Bilateral ulcers at the introitus and on the labia minora. B, Epidermis with focal ulceration, foci of parakeratosis, and marked vacuolar degeneration of the basal layer, with necrotic keratinocytes and a chronic inflammatory infiltrate in the superficial dermis. Hematoxylin and eosin, original magnification×200.
The genital manifestations of LE have been described on few occasions in the literature. In 1989, Burge et al.2 estimated a prevalence of 5% in patients with chronic DLE, whereas Fresko et al.,7 in 1993, found no genital lesions in a series of 48 women with SLE.
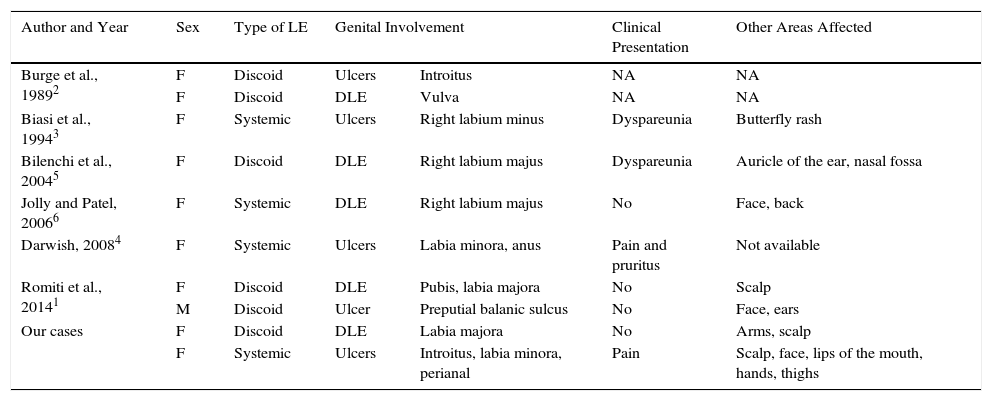
We have found only 8 published cases (Table 1),1–6 of which 7 were women. Five of those patients had DLE and 3 SLE. Clinically the lesions include ulcers and erosions,1–4 as well as erythematous atrophic plaques with scarring alopecia characteristic of DLE.1,2,5,6 Both the ulcers and the plaques typical of DLE can appear in patients with SLE or DLE. Although they are usually asymptomatic, 2 women reported dyspareunia3,5 and one described pruritus and discomfort on passing urine or defecating.4 The histology is typical of LE, with hyperkeratosis, a perivascular and periadnexal inflammatory infiltrate, vacuolar degeneration of the basal layer, apoptotic keratinocytes, and mucin deposits, although not all findings are always present.1–6
Characteristics of Our Patients and of Those Described in the Literature.
| Author and Year | Sex | Type of LE | Genital Involvement | Clinical Presentation | Other Areas Affected | |
|---|---|---|---|---|---|---|
| Burge et al., 19892 | F | Discoid | Ulcers | Introitus | NA | NA |
| F | Discoid | DLE | Vulva | NA | NA | |
| Biasi et al., 19943 | F | Systemic | Ulcers | Right labium minus | Dyspareunia | Butterfly rash |
| Bilenchi et al., 20045 | F | Discoid | DLE | Right labium majus | Dyspareunia | Auricle of the ear, nasal fossa |
| Jolly and Patel, 20066 | F | Systemic | DLE | Right labium majus | No | Face, back |
| Darwish, 20084 | F | Systemic | Ulcers | Labia minora, anus | Pain and pruritus | Not available |
| Romiti et al., 20141 | F | Discoid | DLE | Pubis, labia majora | No | Scalp |
| M | Discoid | Ulcer | Preputial balanic sulcus | No | Face, ears | |
| Our cases | F | Discoid | DLE | Labia majora | No | Arms, scalp |
| F | Systemic | Ulcers | Introitus, labia minora, perianal | Pain | Scalp, face, lips of the mouth, hands, thighs | |
Abbreviations: DLE, discoid lupus erythematosus; F, female; LE, lupus erythematosus; M, male; NA, not available.
A recent publication from 2015 described a series of 22 patients with bullous LE, in which 2 of the patients presented genital lesions. However, the morphology, site, duration, and time since onset of the genital manifestations were not reported.8 We have found no cases of subacute LE affecting the genitalia.
Our 2 patients illustrate the 2 identified profiles of genital manifestations in LE: one of them had the typical plaques of DLE, which enabled us to make the diagnosis, while the other patient presented ulcers, leading to a broader differential diagnosis, mainly including sexually transmitted infections such as herpes simplex and syphilis, and aphthous disorders, including Behçet disease, fixed pigmented erythema, and erosive lichen planus.5
The pathogenic mechanisms responsible for the skin lesions of LE are not fully understood. In one study, no differences were found in cytokine expression between the lips (sun-exposed area) and the oral mucosa (sun-protected area). This would suggest that although UV light may be the most relevant environmental factor in the induction of skin lesions, there could be other intrinsic mechanisms that are similar in the 2 areas.9 In addition, other factors, such as the Köebner phenomenon, could be the key to involvement of the genitalia.1
Therapy is the same as for other manifestations of lupus erythematosus. The treatments of choice are a high-potency topical corticosteroids plus systemic hydroxychloroquine or chloroquine.2,4,5
We have presented 2 cases of LE affecting the genitalia. One patient with DLE who presented asymptomatic, whitish atrophic plaques, and another with long-standing SLE in which painful erosions developed at the introitus. Genital involvement is rare in LE and is perhaps underdiagnosed. It can present in the 2 clinical forms described. It is important to be aware of these presentations to make a correct diagnosis, and the existence of genital lesions or discomfort should be recorded in the medical history.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: del Alcázar-Viladomiu E, López-Pestaña A, Tuneu-Valls A. Lupus eritematoso con afectación genital: una localización inusual. Actas Dermosifiliogr. 2018;109:78–80.