The rapid spread of coronavirus SARS-CoV-2 infection and its associated disease (COVID-19) constitute a major public health problem.
The SARS-CoV-2 pandemic has led to the suspension of most phototherapy units throughout the country because hospitals must adapt in order to prioritize treatment of COVID-19. However, maintenance of phototherapy with the application of special safety measures during the pandemic was recently addressed.1
Information is still lacking on the impact of skin diseases covered by phototherapy and their treatment during the course of SARS-CoV-2 and vice versa.
As the pandemic gradually comes under control, we must consider the requirements, limitations, and conditions for resuming the service provided in phototherapy units in a scenario where it is assumed that the virus will continue to circulate, with occasional and seasonal exacerbations.2
The risk of spread of SARS-CoV-2 in phototherapy units is unknown. While common areas in these units follow disinfection protocols that are similar to those of other hospital services, phototherapy is administered in the reduced space of UV booths, where patients are in contact with the equipment at an ambient temperature that facilitates maintenance and spread of the virus. Such circumstances render disinfection difficult with standard protocols and lead us to consider various safety issues with respect to the spread of SARS-CoV-2 between patients and between patients and health professionals. UV radiation, mainly UV-C, has long been used as a germicide in devices with wavelengths of 254 nm, which are consistent with the maximum wavelengths for absorption of DNA and RNA molecules and, therefore, have a marked ability to damage cells directly. Recent publications during the pandemic indicate the necessary germicidal doses of UV-C radiation for mechanical ventilation units caring for severely ill patients with coronavirus infection. Nonetheless, there is no scientific evidence showing that the UV-A and UV-B bands used in phototherapy booths during treatment are sufficient and appropriate in cases of exposure to the virus, even though they are potentially germicidal.3,4
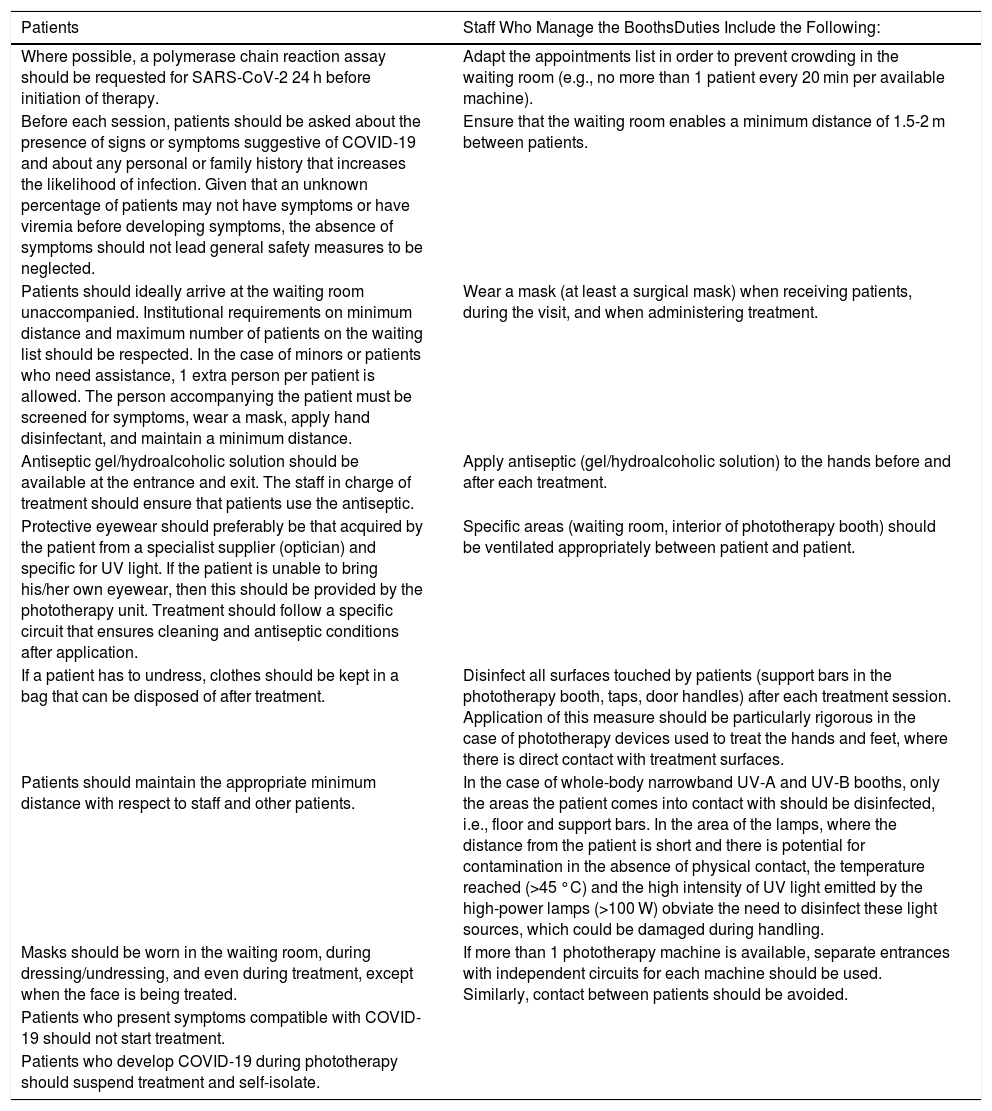
Therefore, the Spanish Photobiology Group of the Spanish Academy of Dermatology and Venereology has developed a series of recommendations to balance risks and benefits for patients and to optimize safety for staff in charge of visits and administration of treatment (Table 1).
Recommendations for Patients and Health Professionals.
| Patients | Staff Who Manage the BoothsDuties Include the Following: |
|---|---|
| Where possible, a polymerase chain reaction assay should be requested for SARS-CoV-2 24 h before initiation of therapy. | Adapt the appointments list in order to prevent crowding in the waiting room (e.g., no more than 1 patient every 20 min per available machine). |
| Before each session, patients should be asked about the presence of signs or symptoms suggestive of COVID-19 and about any personal or family history that increases the likelihood of infection. Given that an unknown percentage of patients may not have symptoms or have viremia before developing symptoms, the absence of symptoms should not lead general safety measures to be neglected. | Ensure that the waiting room enables a minimum distance of 1.5-2 m between patients. |
| Patients should ideally arrive at the waiting room unaccompanied. Institutional requirements on minimum distance and maximum number of patients on the waiting list should be respected. In the case of minors or patients who need assistance, 1 extra person per patient is allowed. The person accompanying the patient must be screened for symptoms, wear a mask, apply hand disinfectant, and maintain a minimum distance. | Wear a mask (at least a surgical mask) when receiving patients, during the visit, and when administering treatment. |
| Antiseptic gel/hydroalcoholic solution should be available at the entrance and exit. The staff in charge of treatment should ensure that patients use the antiseptic. | Apply antiseptic (gel/hydroalcoholic solution) to the hands before and after each treatment. |
| Protective eyewear should preferably be that acquired by the patient from a specialist supplier (optician) and specific for UV light. If the patient is unable to bring his/her own eyewear, then this should be provided by the phototherapy unit. Treatment should follow a specific circuit that ensures cleaning and antiseptic conditions after application. | Specific areas (waiting room, interior of phototherapy booth) should be ventilated appropriately between patient and patient. |
| If a patient has to undress, clothes should be kept in a bag that can be disposed of after treatment. | Disinfect all surfaces touched by patients (support bars in the phototherapy booth, taps, door handles) after each treatment session. Application of this measure should be particularly rigorous in the case of phototherapy devices used to treat the hands and feet, where there is direct contact with treatment surfaces. |
| Patients should maintain the appropriate minimum distance with respect to staff and other patients. | In the case of whole-body narrowband UV-A and UV-B booths, only the areas the patient comes into contact with should be disinfected, i.e., floor and support bars. In the area of the lamps, where the distance from the patient is short and there is potential for contamination in the absence of physical contact, the temperature reached (>45 °C) and the high intensity of UV light emitted by the high-power lamps (>100 W) obviate the need to disinfect these light sources, which could be damaged during handling. |
| Masks should be worn in the waiting room, during dressing/undressing, and even during treatment, except when the face is being treated. | If more than 1 phototherapy machine is available, separate entrances with independent circuits for each machine should be used. Similarly, contact between patients should be avoided. |
| Patients who present symptoms compatible with COVID-19 should not start treatment. | |
| Patients who develop COVID-19 during phototherapy should suspend treatment and self-isolate. |
All of these actions can limit the number of phototherapy sessions with respect to standard numbers administered before the COVID-19 pandemic. This in turn may lead to alternative treatments being considered in some cases and in specific diseases and to treatment being restricted to those cases that are most likely to respond or for which few alternatives are available. However, maintenance of phototherapy as a feasible option in dermatology departments currently depends on it being possible to guarantee the safety both of patients and of the attending health professionals.
These considerations may be modified in the coming months depending on the course of the pandemic and new evidence.
Please cite this article as: Aguilera P, Gilaberte Y, Pérez-Ferriols A, de Argila D, Aguilera J, de Galvez MV, et al. Recomendaciones del Grupo Español de Fotobiología de la AEDV en referencia al manejo de las unidades de fototerapia durante la pandemia por SARS-CoV-2. Actas Dermosifiliogr. 2021;112:73–75.