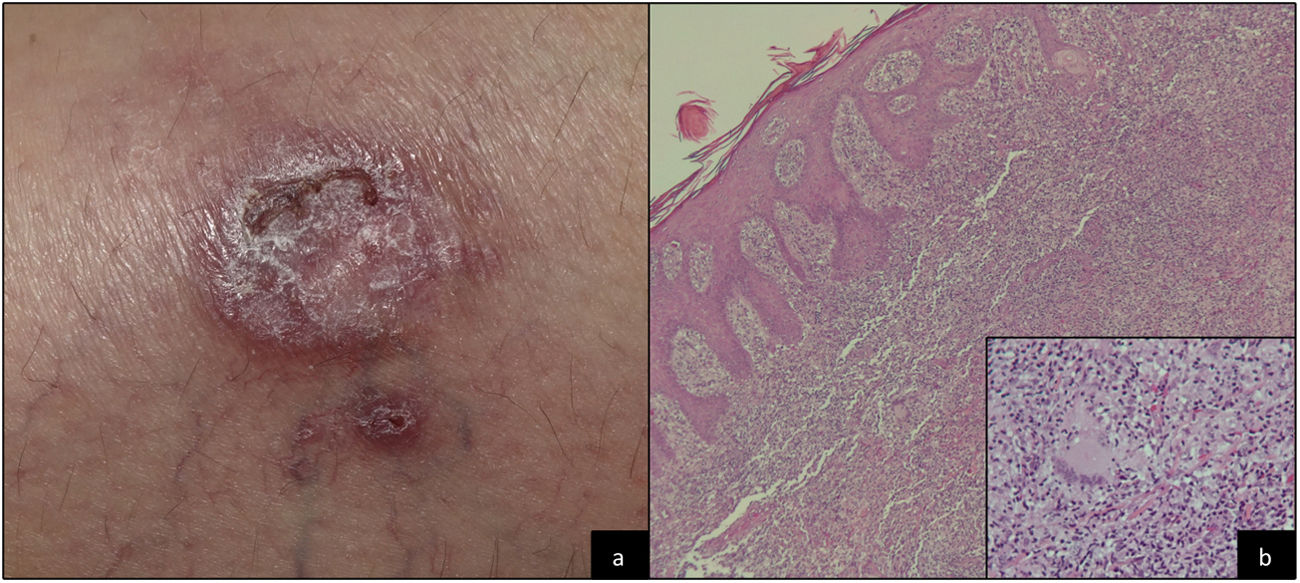
A 41-year-old woman was evaluated in the dermatology clinic for an asymptomatic ulcer that had first appeared on her left leg 3 months earlier. The lesion had violaceous borders and a keratotic center (Fig. 1A). The patient had fistulizing ileocolonic Crohn disease, for which she had undergone several surgical procedures (total proctocolectomy, resection of the small intestine, and terminal ileostomy). Her disease was well controlled with infliximab at 5mg/kg every 8 weeks, which she had been taking for the last 9 years.
A sample was taken for microbiological culture and a biopsy for histopathology. The culture result was negative, and the biopsy revealed a bandlike inflammatory infiltrate at both the superficial level and the deep level. This comprised lymphoid cells and occasional nonnecrotizing granulomas with multinucleated giant cells (Fig. 1B) and was compatible with metastatic Crohn disease.
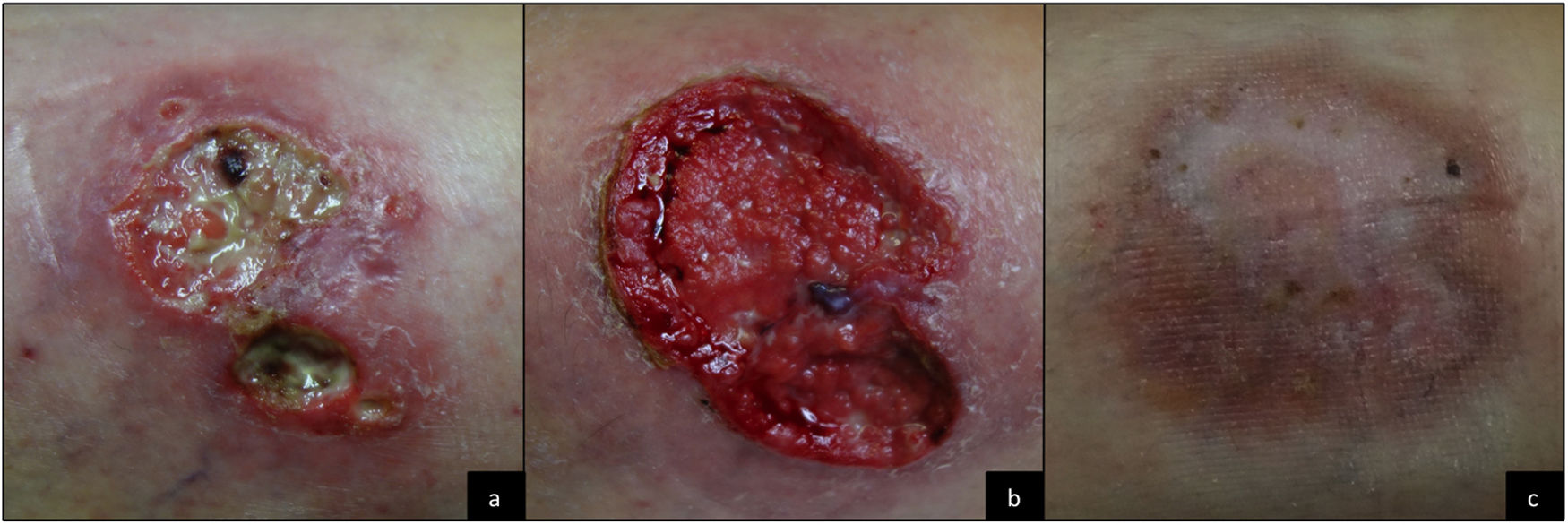
Daily topical treatment was started with clobetasol ointment, and the infliximab regimen was intensified temporarily to 4 weeks at the same dose. The lesion healed completely within 2 months. However, erosive crusting lesions appeared gradually at the same site. These progressed slowly until they again became ulcerated (Fig. 2A). The infliximab regimen was modified to 6 weeks, and additional treatments were prescribed, as follows: azathioprine 100mg every 24hours (dose adjusted according to thiopurine methyltransferase levels), oral prednisone cycles at 0.5-1mg/kg/d, and intralesional triamcinolone infiltrations. This approach was unsuccessful. The infliximab regimen was subsequently intensified to 4 weeks, and metronidazole 500mg every 8hours was added. Wet-wrap dressings (HydroClean Advance) were applied throughout treatment, and the patient was monitored for signs of superinfection. Despite the treatment prescribed, the ulcers worsened quickly and became larger and deeper (Fig. 2B). The patient remained free of digestive symptoms at all times.
Given the failure of therapy and the new indication of ustekinumab for Crohn disease, we agreed with the Gastroenterology Department to change the therapeutic target and start treatment with ustekinumab in monotherapy according to the established regimen for Crohn disease and based on the patient’s weight. The induction dose administered was 390mg followed by 90mg every 8 weeks subcutaneously. Initiation of ustekinumab led to a rapid improvement in the ulcer from the first month and complete cure in 3 months (Fig. 2C), with no adverse effects.
Metastatic Crohn disease is a rare extraintestinal manifestation of Crohn disease. While no epidemiological data are available, it is the least common specific cutaneous manifestation. The condition is characterized by the appearance of heterogeneous cutaneous and subcutaneous lesions comprising noncaseating granulomata at anatomic sites not contiguous to the gastrointestinal tract. It may precede, co-occur with, or follow the gastrointestinal disease. The lesions can mimic other more common skin conditions, such as impetigo, erysipelas, erythema nodosum, and pyoderma gangrenosum.1
Clinical suspicion is essential for biopsy and early diagnosis, since the definitive diagnosis is confirmed by histopathology. The presence of persistent skin lesions in patients with Crohn disease should lead us to suspect this possibility, even if the patient is receiving immunosuppressive or biologic therapy and despite the fact that digestive symptoms have remitted.2
If the patient is receiving treatment with an anti–tumor necrosis factor (TNF) α agent, monitoring drug levels and antibody testing would contribute to better management of therapy, since we could determine whether drug levels were insufficient and whether the cause was underdosing or the presence of antibodies.3 Unfortunately, and despite the clinical interest of this approach, the required techniques are not available in many centers or for all biologics.
As there is no standard treatment for this condition, management should be tailored. If the lesions are localized, we can consider local treatments, such as topical corticosteroids or tacrolimus, or even intralesional corticosteroids.1 If there is no response, systemic treatment with oral corticosteroids can be considered. If these fail or are insufficient, then conventional immunosuppressants or biologics can be added.1 Cases have been treated with metronidazole, mycophenolate mofetil, ciclosporin, adalimumab, infliximab, certolizumab, thalidomide, surgery, and hyperbaric oxygen therapy.2–5 All of the biologics used were anti-TNF-α antibody agents. The only case reported of Crohn disease involving the genital region (vulvar and perineal) was successfully treated with ustekinumab.6
Ustekinumab is a monoclonal antibody that targets the p40 subunit of the IL-12 and IL-23 receptors. It has been indicated for Crohn disease since 2017. Given that its therapeutic target is not TNF-α, ustekinumab may prove to be a therapeutic option in patients with metastatic Crohn disease whose treatment with corticosteroids, immunosuppressants, or anti-TNF-α agents has failed.
Please cite this article as: Ballester Sánchez R, Sanchís Sánchez C, Rodrigo Nicolás B, Valcuende Cavero F. Enfermedad de Crohn metastásica tratada con ustekinumab. Actas Dermosifiliogr. 2021;112:182–183.