The term psiloliparus is derived from the Greek word “psilos” which means hairless and “liparos” which means fatty. It was described in 1997 as a distinct type of mesodermal nevus affecting the scalp which is frequently a manifestation of the Encephalocraniocutaneous lipomatosis syndrome (ECCL), but it can also be present in isolation as a nonsyndromic form.1
We report two nonsyndromic nevus psiloliparus cases and one ECCL-related case.
Case study 1A female 13-year-old patient consulted due to the presence of two soft alopecic plaques located in the occipital region present since her birth (Fig. 1A).
Physical examination revealed that the plaques presented normal skin color, with a soft cotton-like surface, some white peripheral hair and they were asymptomatic.
Her psychomotor development was age-appropriate and she did not present neither convulsive history nor ocular abnormalities.
A magnetic resonance imaging (MRI) of the brain was performed and it exposed, over the occipital protuberance, the presence of a foramen in the cranial vault with rim enhancement, apparent sclerosis with absence of cancellous bone and associated with subcutaneous tissue enhancement that presents fat signal at that level, compatible with lipoma. Neither protrusions of encephalic nor meningeal structures are present in the foramen.
The lesions were in stable conditions over time and the patient did not present any other alterations.
Case study 2A female 3-month-old patient was brought to the hospital with the presence of congenital alopecic plaques on the scalp. The biggest one was a rounded lesion of approximately 3cm diameter, skin-like color, soft, with reduction of hair density. The other two lesions, adjacent to the biggest one, presented smaller round-like shapes with atrophic surface and without hair (Fig. 1B).
The neurological examination was normal. A MRI of the brain was requested and it showed the soft tissues lesion, without neither alterations of the central nervous system (CNS) nor communication between the lesion and the CNS.
The ophthalmologic and audiological examinations were normal.
Case study 3A female 10-month-old patient was brought to the hospital due to the presence of two congenital alopecic plaques of soft consistency located in the frontal region (Fig. 1C).
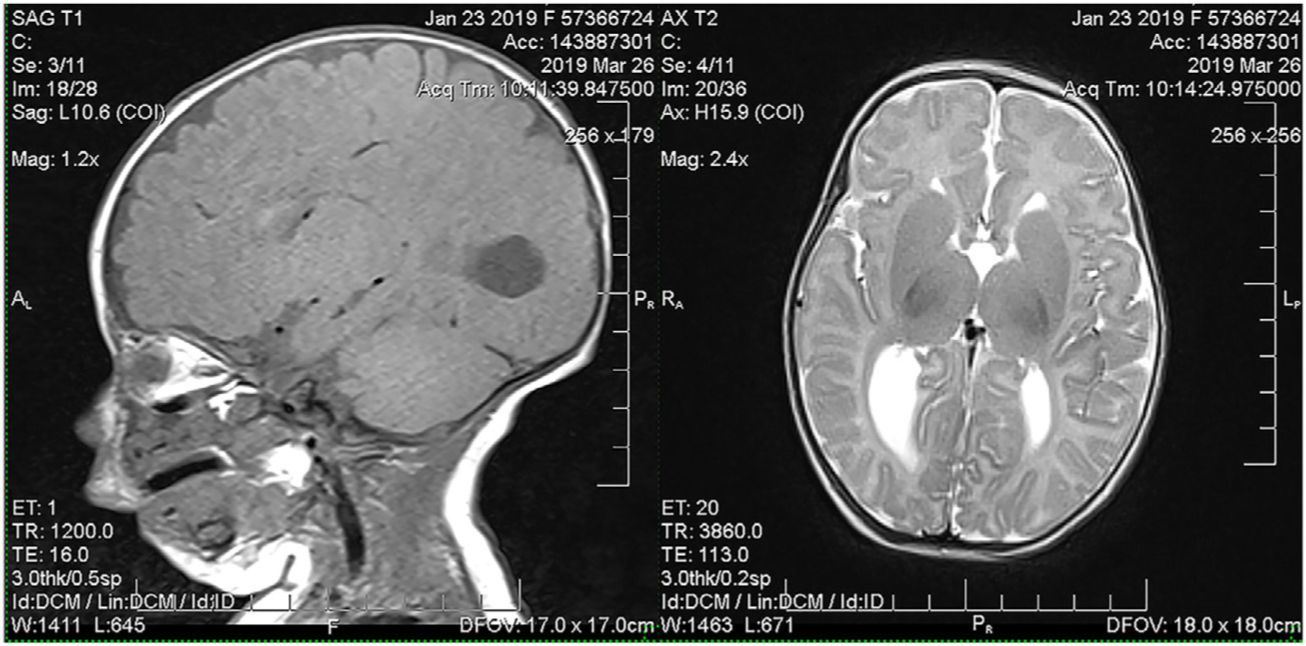
The MRI (Fig. 2) showed Agenesis of the corpus callosum, associated to a previous nodular lesion of 13mm, of high-intensity fat signal, attributable to a lipoma; and dilatation of the occipital horns of the lateral ventricles (Colpocephaly). In spite of the previously mentioned conditions, her neurological development to the present is age-appropriate. The ophthalmologic and audiological examinations were normal.
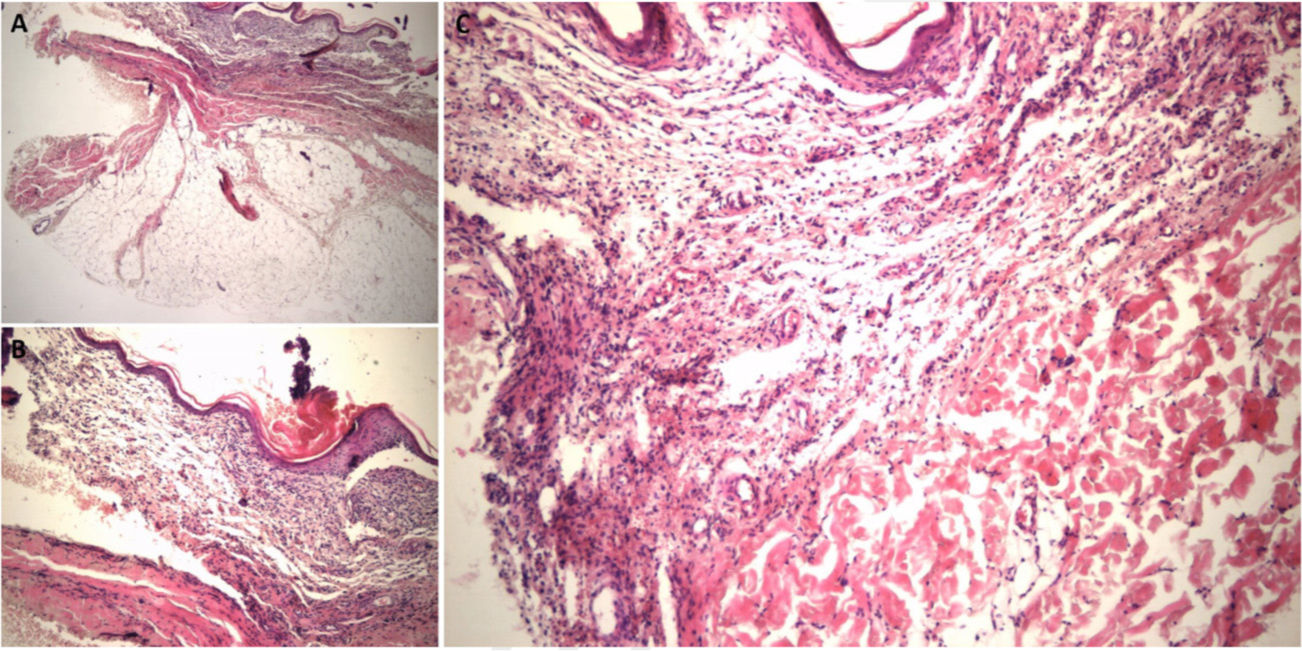
A skin biopsy was carried out in the 3 patients and the results were quite similar: abundant mature adipose tissue in depth, compressing the overlying dermis and absence of hair follicles and adnexal structures (Fig. 3), with “orphaned” hair erector muscles. The diagnosis was nevus psiloliparus.
DiscussionNevus psiloliparus is a skin lesion of mesodermal origin. It is clinically present at scalp level as a slightly raised plaque with well-defined margins, sometimes irregular, skin-colored or slightly yellowish, generally unilateral and located in the frontal or frontal–parietal region. Its most distinctive features are absence (or reduction) of the amount of hair follicles and excessive increase of mature adipose tissue.1,2
Histologically, it presents three main characteristics:
- -
abundance of non-encapsulated mature adipose tissue that may compress the dermis and make it thinner,
- -
reduction or absence of mature hair follicles,
- -
presence of regular amount of fascicles of “orphaned” hair erector muscles, that is to say, independent or non-associated with a hair follicle, located on lines parallel to the epidermal surface.3
It is frequently a marker of ECCL (Haberland or Fishman Syndrome), pathology which is characterized by the triad of: neurological anomalies (intraspinal lipomas, asymmetry of intracranial vessels, hemispherical atrophy, ventricular dilatation, etc.), ocular anomalies (choristomas, colobomas, corneal anomalies or anomalies of the anterior chamber, etc.) and skin anomalies (nevus psiloliparus, subcutaneous frontotemporal lipomas, hypoplasia or focal dermal hypoplasia). The latter are usually unilateral, located on the face and/or scalp. The most frequent one is nevus psiloliparus that represents a major criterion for this syndrome. There is no correlation between the seriousness of the neurological alterations (which determine the prognosis of these patients) and the skin lesions.4,5
The coexistence of nevus psiloliparus and aplasia cutis congenita (ACC) on the same lesion, called didymosis aplasticopsilolipara according to Torrello et al, has been described as being part or not being part of ECCL.6–8
Considering the aforesaid, we want to make emphasis on the importance of performing a complete and multidisciplinary study when we detect the presence of this type of skin lesions in order to rule out systemic threat as it occurred to our third patient. We should also know that there are isolated cases of nevus psiloliparus, as described in literature, similar to our two first case studies.
Conflict of interestThe authors declare that they have no conflict of interest.