The term paraffinoma refers to histological abnormality caused by subcutaneous injection of paraffin or mineral oil. The lesion is characterized by a pseudocystic pattern described in the scientific literature as Swiss-cheese appearance.1 Given the intrinsic properties of this material, which is inert and cannot be absorbed by the body, it has traditionally been used to increase the volume of certain areas of the body, such as the cheeks, lips, breasts, and external genitals.2,3
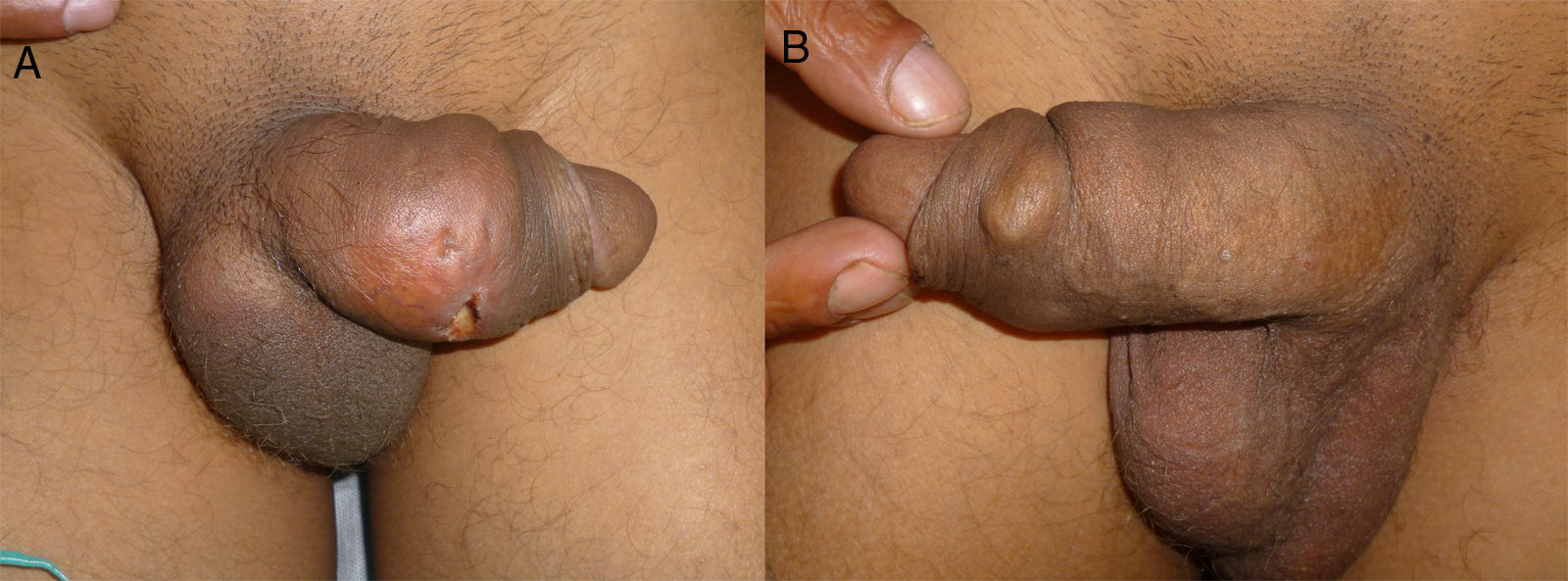
A 42-year-old man from Romania presented with a mass, which had been growing progressively over the last 20 years, on the dorsum of the penis. The lesion had been stable until 15 days earlier, when it started to become inflamed until a painful central ulcer developed. The physical examination revealed a mass with a stony consistency measuring 5×7cm in diameter in the dorsolateral region of the penis shaft. An ulcer of 1cm in diameter was present on the mass, with a fibrinous base and mild serous exudate (Fig. 1a). A rounded, hard, subcutaneous tumorous mass was observed on the ventrolateral aspect of the penis, measuring 2cm in diameter (Fig. 1b). This lesion was not painful to palpation. Of note was the presence of multiple, bilateral, swollen, stony, inguinal lymph nodes that were not painful. Given that the clinical manifestations were consistent with long-term complications of injectable filler materials, a detailed medical history was taken. This finally revealed that melted lipstick had been injected several times to increase the size of his penis.
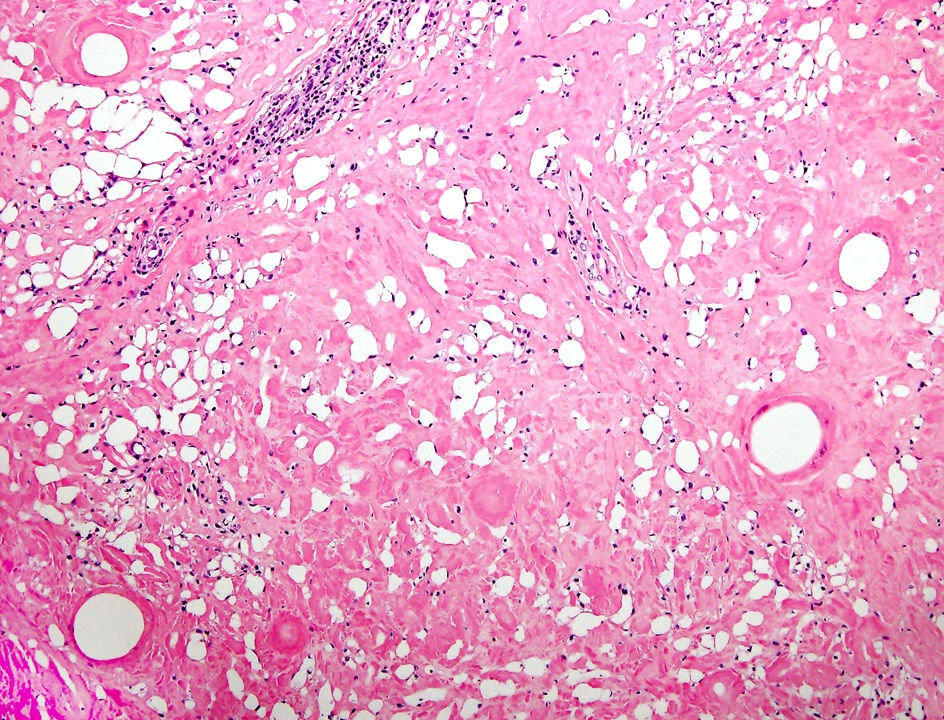
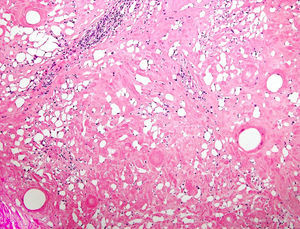
A histopathological study revealed diffuse eosinophilic sclerosis of the reticular dermis and subcutaneous tissue, completely replacing lobules of adipose tissue while preserving the septa. Isolated foci of lymphocytic infiltrate and multiple empty cavities surrounded by giant multinucleated cells formed the typical Swiss-cheese image (Fig. 2).
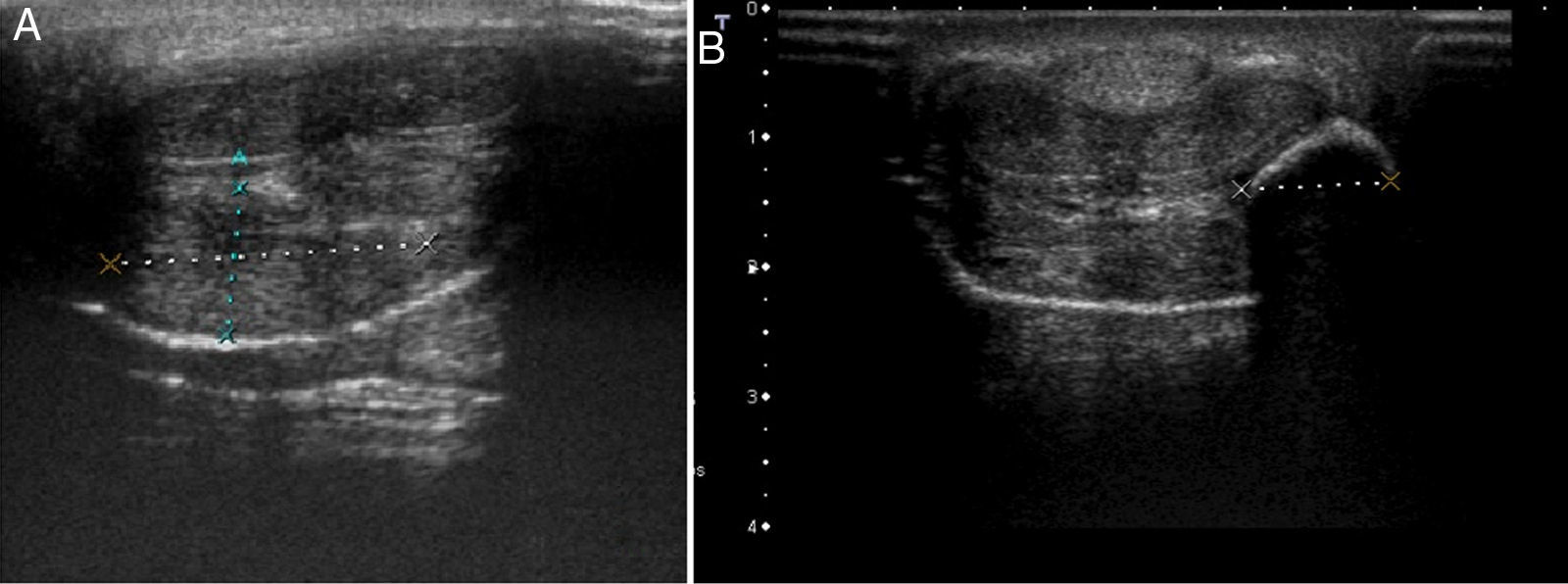
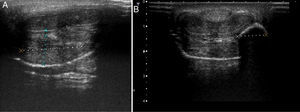
An ultrasound study of both lesions was undertaken with a linear 14MHz probe. The first lesion showed marked focal thickening of the subcutaneous cell tissue of the shaft of the penis, with no collections or foreign bodies detectable in the ultrasound throughout its thickness (Fig. 3a). No abnormalities were observed in the corpora cavernosa or the corpus spongiosum. In the second lesion, a well-defined hyperechogenic nodule measuring 10×12mm in diameter was observed with a posterior acoustic shadow (Fig. 3b). In addition, bilateral hyperechogenic swollen inguinal lymph nodes with no defined fatty hila could be observed, probably related to lymphatic drainage of foreign material.
The patient underwent surgery in the urology department. The affected region was completely excised and reconstruction surgery performed with direct closure. Unfortunately, the patient refused return for lymph node biopsy and was definitively lost to follow-up after the operation.
Injection of paraffin or mineral oil by nonmedical personnel, with the aim of increasing the size of the penis, is a common problem in countries in Eastern Europe and certain areas of Asia.4 Given that humans naturally lack specific enzymes to degrade mineral oils, subcutaneous injection of this type of substance is followed by a granulomatous reaction, the onset of which can be delayed by years. Clinically, onset is usually very nonspecific, with progressive induration, fluctuating edema, and/or local inflammation of the affected area which, as time passes, may be accompanied by necrosis, ulceration, and deformity.
Histology is, without doubt, key for achieving definitive diagnosis of these lesions. Typically, paraffinoma is characterized by the replacement of subcutaneous cell tissue with empty cystic spaces of variable size that give a Swiss-cheese appearance.1 The process is accompanied by a granulomatous foreign body reaction, with extensive fibrosis and marked inflammatory infiltrate, mainly composed of giant multinucleated cells.4
Although skin abnormalities at the injection site are the most frequent complications, other potentially more serious reactions may occur, as was the case in our patient, with likely regional lymph node involvement.5 There have even been reports of fatal lung involvement caused by migration of the filler material used.6
An exhaustive medical history is essential for diagnosis, as the patient may omit part of the prior history due to fear or shame.3 Differential diagnosis should include infectious processes such as abscesses, canker sores, thrombosis of the dorsal vein of the penis, and tumors.7 Ultrasound, which is a widely available and inexpensive technique, can be very useful for differential diagnosis. This imaging technique can also determine the involvement of structures such as the corpora cavernosa and regional lymph nodes, as well as detect the formation of abscesses or fistulas. Furthermore, it can help identify the type of filler material, as specific echographic patterns have been described for some of these.8–10 For example, in the second image, the so called snow storm pattern is observed, where a hyperechogenic region has a posterior acoustic shadow. This pattern is typical in nonabsorbable filler materials such as silicone oil, pure silicone,10 and, in our case, liquid paraffin.
To date, the only truly effective and definitive treatment for penile paraffinoma is surgical excision. This process may, at times, require substantial surgical reconstruction through grafts and/or plasties to cover the resulting defect.5
It is very important that the dermatologist recognizes the complications of filler materials, particularly when applied by nonmedical personnel. Ultrasound is of great help, both for identifying the filler material and for recognition of local complications or involvement of regional lymph nodes.
Conflicts Of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Morales-Raya C. Parafinoma de pene: ¿le hacemos una ecografía?. 2017;108:477–479.