Although comedones are a prevalent entity in multiple skin diseases, their perianal location as a cluster is a rare finding. We describe 5 patients with grouped perianal comedones who developed the lesions in adulthood and were treatment-naïve in the perianal area. Four of them had had inflammatory lesions in armpits and groins. In 2, the anatomopathological examination revealed the presence of follicular infundibulum dilatation, cystification, and fibrotic and inflammatory changes in the underlying dermis—findings consistent with hidradenitis suppurativa—which is why we wonder whether grouped perianal comedones are a mild form of hidradenitis suppurativa or an isolated entity.
Los comedones son prevalentes en múltiples enfermedades que afectan a la piel, pero su localización perianal de forma agrupada es infrecuente. Describimos cinco pacientes con comedones perianales agrupados que habían desarrollado las lesiones en la edad adulta, sin la aplicación previa de ningún tratamiento en la zona. Cuatro de ellos habían tenido lesiones inflamatorias en las axilas y las ingles, y en dos se realizó un análisis anatomopatológico, observando dilatación del infundíbulo folicular y quistificación, además de cambios fibróticos e inflamatorios en la dermis subyacente compatibles con una hidradenitis supurativa. Con estos hallazgos, planteamos si los comedones perianales agrupados pudieran corresponder a una forma leve de hidradenitis supurativa o bien considerarse una entidad propia.
The presentation of grouped comedones is a rare and understudied entity. They have been described in acne, Favre–Racouchot syndrome, and hidradenitis suppurativa, typically associated with other cutaneous manifestations and more commonly located on the face and trunk.1,2 They are also found in less prevalent conditions such as Dowling–Degos disease,3 Birt–Hogg–Dubé syndrome, folliculotropic mycosis fungoides, and, occasionally, chronic cutaneous lupus.1,2,4,5 Additionally, comedones are the characteristic lesion of nevus comedonicus.6
Methods and case reportsBetween 2021 and 2023, 5 patients with grouped perianal comedones were evaluated at our center—4 men and 1 woman aged 37–65 years—with a 1–3-year history of symptomatic perianal lesions, with pruritus being the most prevalent symptom. The patients’ past medical histories and supplementary data are shown in the attached table (Table A, Appendix). Four patients also reported inflammatory and painful lesions in other locations (axillae and groin), for which they had sought treatment in emergency departments and received oral and/or topical antibiotics in 2 cases.
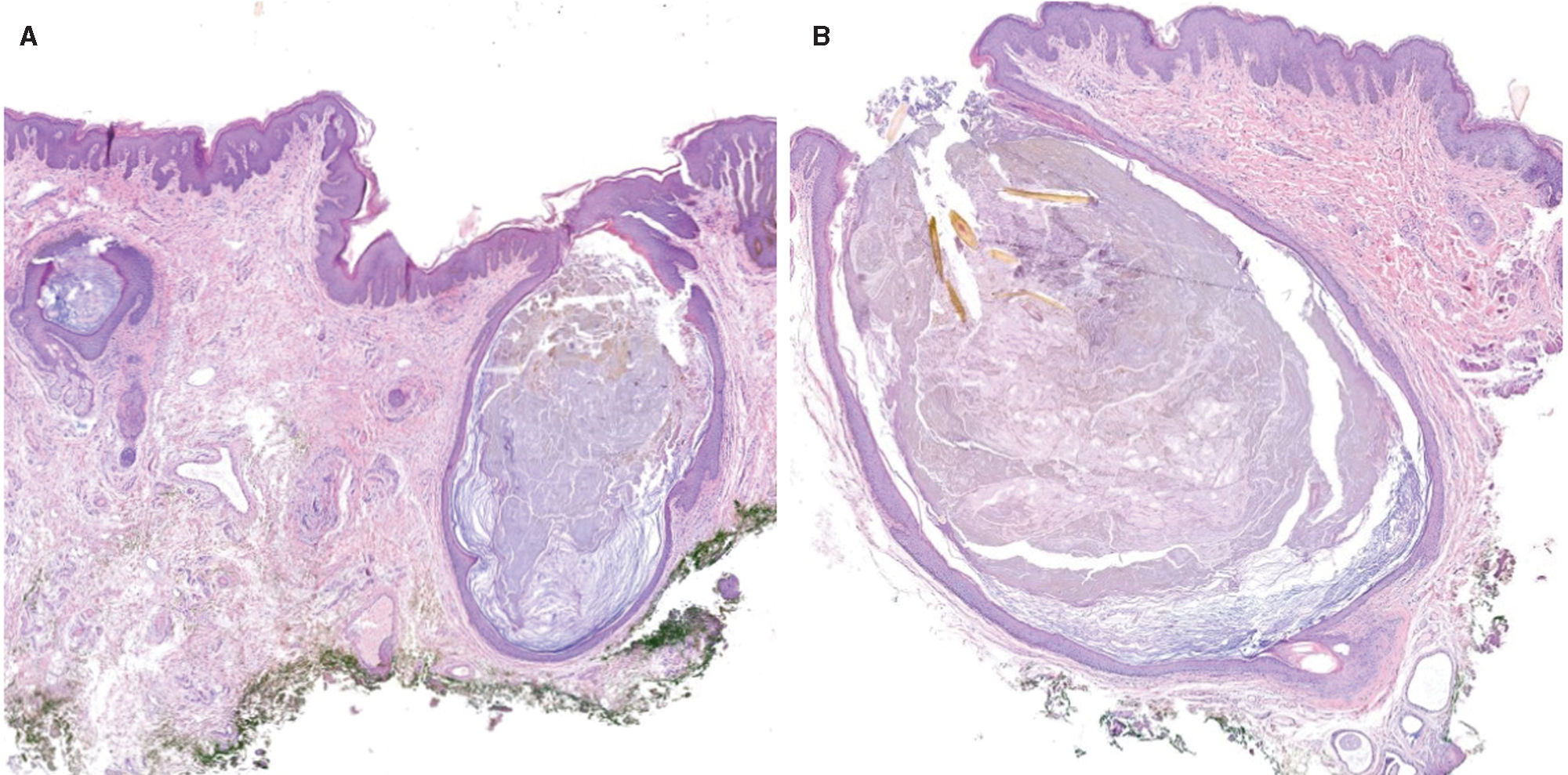
Physical examination revealed multiple open comedones with black follicular plugs, grouped in the perianal region. Some patients also exhibited closed comedones (Fig. 1). On the rest of the skin, 2 patients exhibited epidermoid cysts, and 1, multiple grouped comedones, cysts, and atrophic scars on the trunk, axillae, occipital region, and retroauricular area. In 2 patients, the histopathological analysis of the perianal area revealed dilated follicular openings filled with keratin, along with fibrotic and inflammatory changes in the underlying dermis, all findings consistent with hidradenitis suppurativa (Fig. 2).
Regarding treatment, no patient had previously applied topical products to the perianal area. After lesion onset, the 1st patient, who had experienced suppuration and episodes of perianal inflammation, was treated with cloxacillin, oral doxycycline, and topical mupirocin, with no improvement. Finally, a 2-step deroofing procedure was performed, yielding good esthetic results and symptom resolution. The 2nd patient reported pruritus improvement after applying fusidic acid. The woman, however, showed no improvement despite the use of topical corticosteroids, antibiotics, and antifungals. The remaining 2 cases experienced spontaneous resolution of pruritus without treatment.
DiscussionGrouped perianal comedones have been rarely described in the literature. Oliet and Estes reported the first case back in 1982, linking them to fluorinated corticosteroid use.7 This association was later criticized by Silver,8 who observed these lesions in patients with anal pruritus who had not used any treatments. Subsequently, 3 cases of asymptomatic patients with perianal comedones as incidental findings have been reported.1,2,9 According to these authors, lesion development may result from occlusive effects in the perianal region, along with maceration and exposure to irritants such as feces and bile acids.1,2
We propose that grouped perianal comedones could be a sign of hidradenitis suppurativa, which seemed to be less severe in our cases. Four of the 5 patients had or reported characteristic hidradenitis lesions in other locations, without demonstrating a torpid course of the disease. Additionally, the perianal area is subject to constant friction, facilitating and explaining lesion development. Lastly, 4 patients were smokers, and 1 was an ex-smoker, suggesting tobacco may act as an aggravating factor, as it does in conventional hidradenitis. Hidradenitis suppurativa is an inflammatory disease of the pilosebaceous follicle, clinically presenting with nodules, fistulas, abscesses, scars, and comedones. In hidradenitis, comedones typically appear grouped and are referred to as “double-headed” comedones. Although these lesions can develop anywhere on the skin, they are more common in intertriginous areas.10 It has been reported that mechanical stress or friction plays a key role in the development and exacerbation of hidradenitis lesions, thus explaining their usual localization in skin folds.11
On the other hand, differential diagnosis of the lesions observed in our patients could include nevus comedonicus, an asymptomatic congenital epidermal nevus that appears during childhood characterized by multiple dilated follicular openings filled with keratin, resembling comedones.6 There is also an inflammatory variant of nevus comedonicus, where patients develop hidradenitis-like lesions over the initial nevus. In the series published by Sharma et al.,6 all cases of inflammatory lesions occurred in intertriginous areas. In our patients, this option was ruled out as the lesions appeared during adulthood, and the perianal localization has not been previously reported in nevus comedonicus cases.
ConclusionsGrouped perianal comedones may represent a mild form of hidradenitis suppurativa or constitute a distinct entity without associated lesions. It would be interesting to follow these patients over time to determine whether, in cases where comedones are the sole finding, other characteristic signs of hidradenitis develop, and whether in patients with hidradenitis stigmata, these lesions serve as a marker for mild or aggressive disease progression. We also suggest routinely examining the perianal area in patients with hidradenitis suppurativa, as these lesions may often be present and overlooked.
FundingNone declared.
Conflicts of interestNone declared.
We wish to thank the entire Dermatology team at Hospital Germans Trias i Pujol (Barcelona, Spain) for their contributions and corrections. Special thanks to Dr. Quer for her invaluable assistance and providing histopathology images.