A 57-year-old man with no disease history of interest consulted for episodes of palpebral edema, mainly affecting the right eye. The episodes had been occurring for 8 years. The edema spread to the rest of the face and was accompanied by moderately intense erythema. The clinical picture was not associated with a trigger, and no additional symptoms were reported.
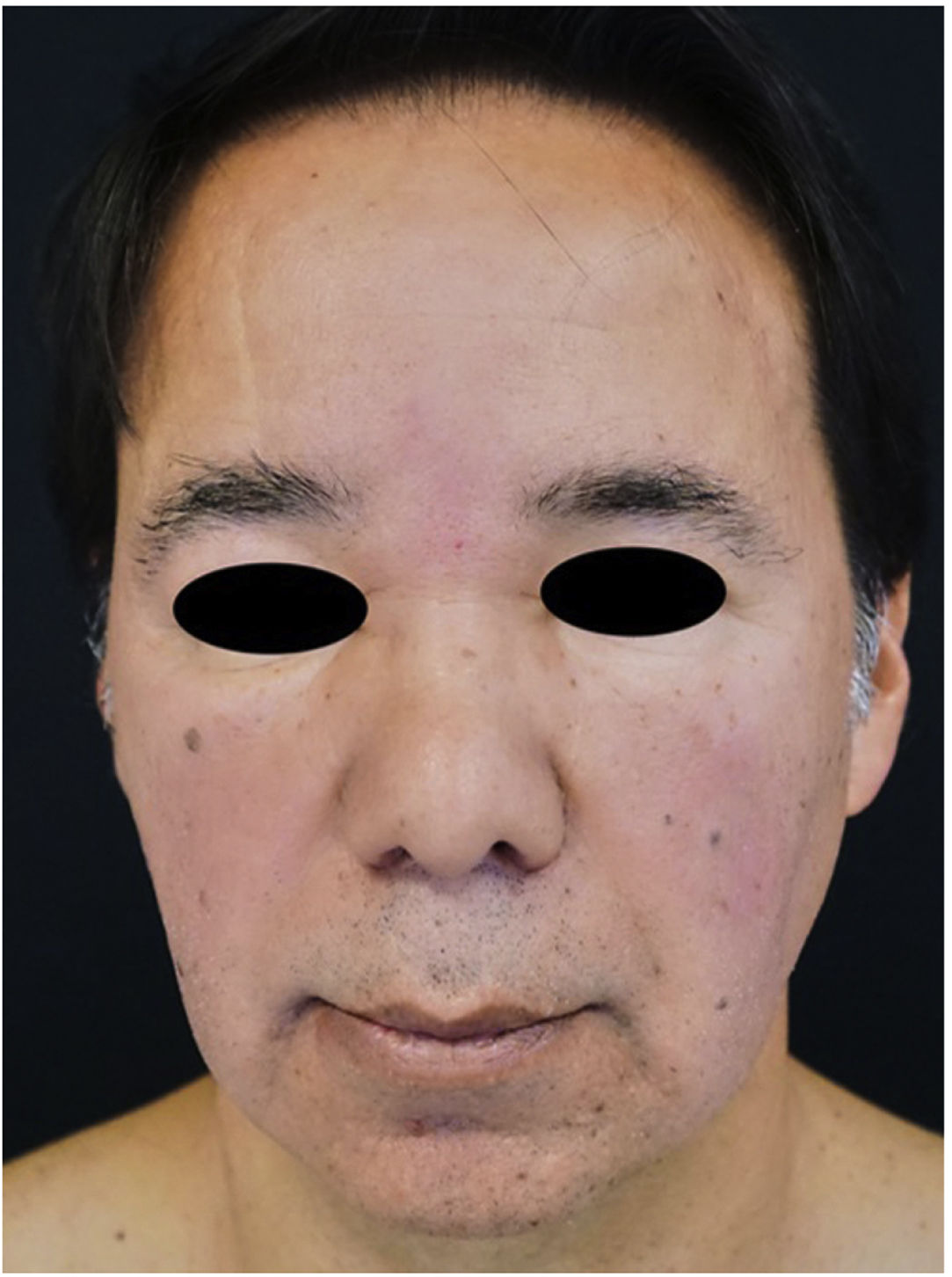
Physical ExaminationThe physical examination revealed bilateral palpebral edema extending to the center of the face and cheeks and accompanied by erythema and scaling that spared the forehead and eyelids (Fig. 1).
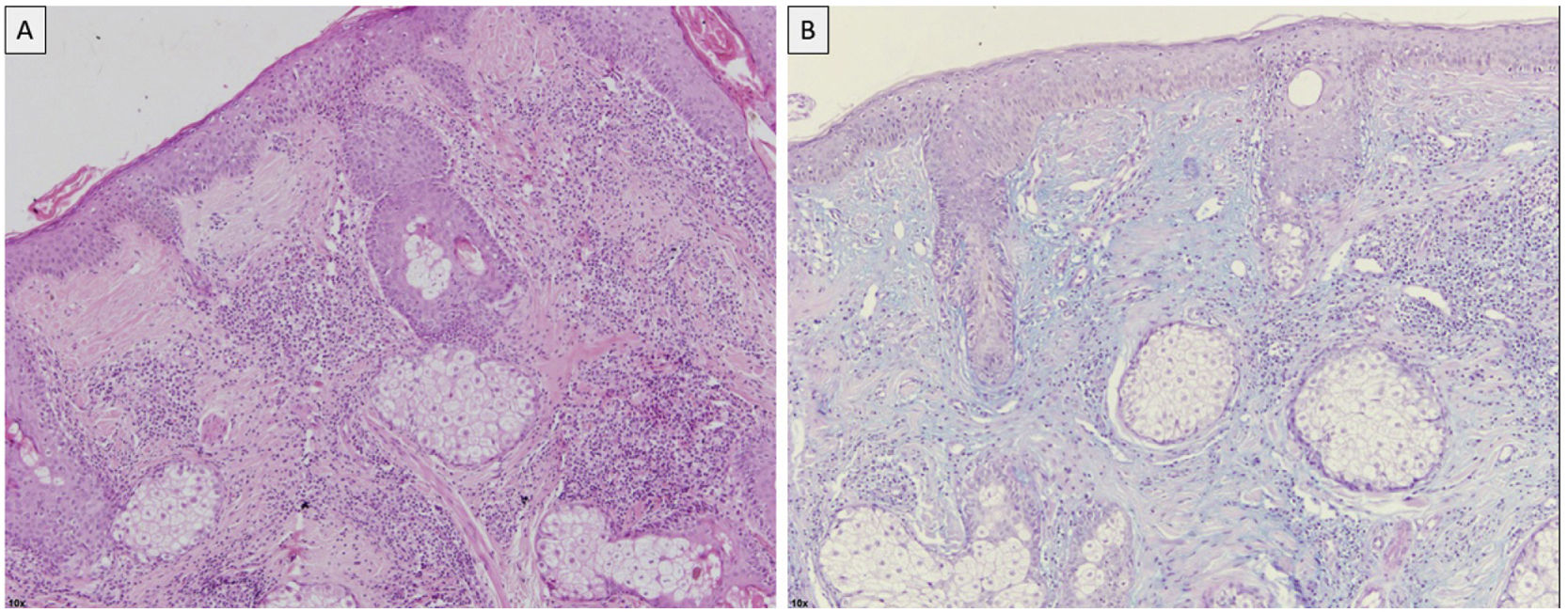
Additional TestsThe blood workup, which included a complete blood count, liver function, kidney function, and autoimmune tests, revealed no significant abnormalities. The histopathology study revealed a thinned horny layer with areas of vacuolization in the basal layer that extended to the infundibular epithelium. The dermis was characterized by edema and an abundant lymphocytic infiltrate surrounding the hair follicles and blood vessels (Fig. 2A). Alcian blue staining showed mucin to be increased in the dermis and around the adnexa (Fig. 2B).
What is Your Diagnosis?
DiagnosisCutaneous lupus erythematosus.
Clinical Course and TreatmentThe patient was prescribed strict photoprotection, together with hydroxychloroquine 400mg/d. Since he did not attend the subsequent checkups, the outcome remains unknown.
CommentLupus erythematosus is an autoimmune disease of the connective tissue that usually progresses with a broad spectrum of clinical, histopathological, and immunological findings. The skin is usually one of the most affected organs.1
The most appropriate classification for the wide range of lesions in lupus erythematosus continues to be debated. However, that of Gilliam and Sontheimer in 1981 is the most widely accepted to date.1,2
Periorbital edema and erythema comprise a rare presentation of chronic cutaneous lupus erythematosus, whose pathophysiological mechanisms are not fully established. Several authors show that the development of edema is favored by the characteristic presence of lax connective tissue and local interstitial mucin deposits.3 Similar findings were reported in the case in which the area affected was the glabella, from where the biopsy was taken.
Involvement of both the upper and lower eyelids has been reported. From the lower eyelid it can extend to the cheeks and may sometimes be accompanied by erythema and pruritus. According to a study by Wu et al.4 in 2018, this condition mainly affects middle-aged women, in whom unilateral left side involvement is the most common finding.4
In some publications, these atypical lesions are classed within the spectrum of chronic cutaneous lupus, with the discoid variant being considered the most common, even though it does not have typical characteristics, such as atrophy, scarring, and follicular plugging.5 However, the persistent and progressive course of the palpebral and facial edema in these cases accounts for their inclusion in this subtype.
As for serology findings, chronic cutaneous lupus is characterized by a lower incidence of positive autoantibodies, such as antinuclear antibodies, anti-double-stranded DNA antibodies, and anti-Sm antibodies. Such were the findings in the case we describe, as in most previously reported cases, where the peripheral blood autoimmunity workup also yielded negative results. Nevertheless, diagnosis is necessarily based on histopathological confirmation. The usual findings correspond to vacuolar degeneration of the basal layer together with epidermal atrophy and abnormalities of the dermis characterized by the presence of a dense perivascular and periadnexal infiltrate.4
The recurrence of symptoms despite multiple treatments and their exacerbation on exposure to sunlight enable us to rule out irritant contact dermatitis, cellulitis, and erysipelas. Heliotrope rash in dermatomyositis can be differentiated by its violaceous coloring, bilateral involvement, and the fact that it is accompanied by characteristic systemic and cutaneous manifestations. Telangiectasias, papules, and pustules (not reported in this manifestation of lupus erythematosus) may be found in Morbihan disease, which is considered a variant of rosacea and progresses with indurated edema affecting the upper two-thirds of the face and whose histopathological findings are nonspecific. Other differential diagnoses to be considered include sarcoidosis, foreign body granuloma, superior vena cava syndrome, and reactions to injectable fillers.4,5
Treatment is based on photoprotection and topical therapy with corticosteroids or calcineurin inhibitors. However, antimalarial drugs continue to be the option of choice.6
Finally, it is well known that some subtypes of lupus erythematosus progress with facial lesions. However, certain signs, such as chronic facial and palpebral edema, with no related findings, continue to be an uncommon and underdiagnosed manifestation, with few cases reported in the last few decades. Therefore, assessment of this condition should take into account a large number of differential diagnoses, among which cutaneous lupus erythematosus is a possibility that should always be investigated.
Conflict of InterestThe authors declare that they have no conflict of interest.