Herpes zoster (HZ) is caused by the reactivation of the latent varicella-zoster virus (VZV) in the dorsal root ganglia. As a result, the most common complication of HZ is postherpetic neuralgia. In rare instances, the virus can involve the ventral horn cells of the spinal nerve, leading to motor complications like an abdominal phantom hernia.1 We describe two such cases that presented to our department.
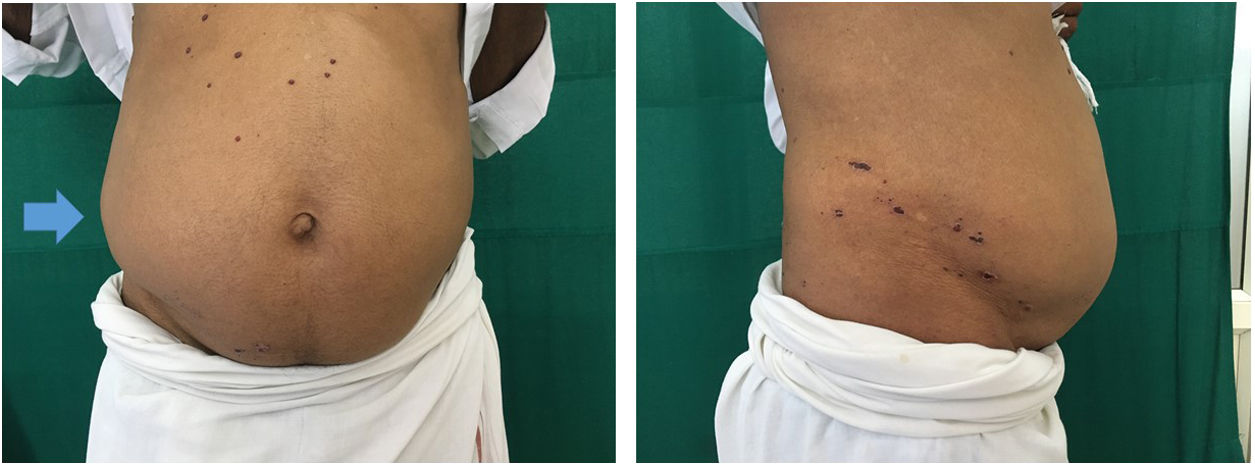
Case 1: A 72-year-old man presented with complaints of swelling and pain on the right side of the abdomen for 10 days. He had a history of herpes zoster that had occurred a month prior and was treated appropriately with antivirals. On examination, we observed crusted haemorrhagic plaques on the right side of the abdomen, involving T11–T12 dermatomes. Distension of the right side of the abdomen was also noted (Fig. 1). Tenderness was present on palpation. An ultrasound of the abdomen and pelvis showed no abnormality. A diagnosis of post-herpetic neuralgia with phantom hernia was made. He was reassured that the distension would resolve with time but was also counselled regarding the possible development of gastric complaints. Review after 3 months showed a mild decrease in the distension with complete resolution after 10 months.
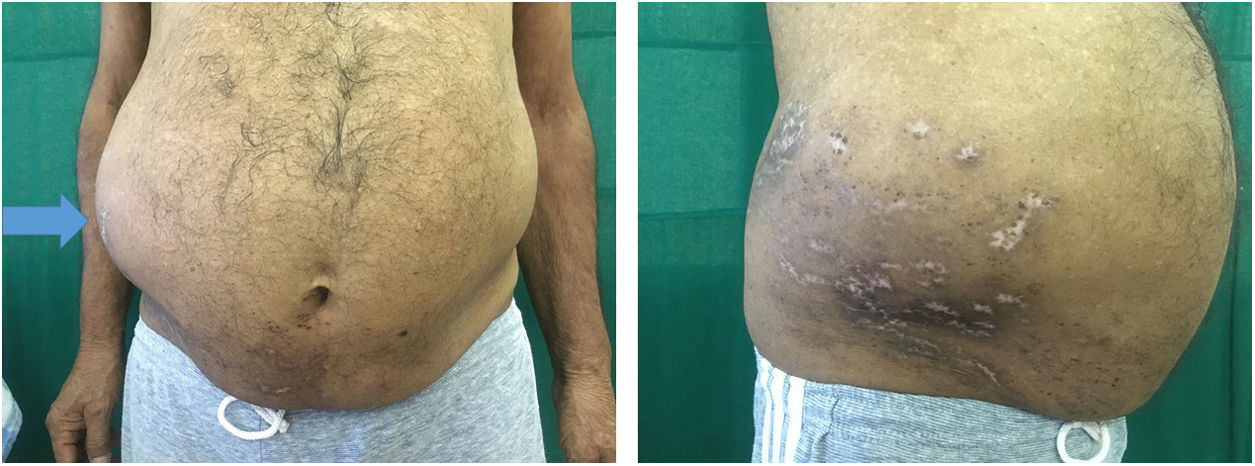
Case 2: A 69-year-old man with comorbidities of diabetes and hypertension was referred to our department. He was treated three months’ prior for herpes zoster of the right T10–T12 dermatomes. On examination, we observed the presence of depigmented atrophic scars on the right side of the abdomen along the T10–T12 dermatomes, with mild distension of the abdomen (Fig. 2). There was no tenderness on palpation. Ultrasonography of the abdomen revealed no abnormality and a diagnosis of phantom hernia was confirmed along with the surgery team. He was reassured and taught abdominal strengthening exercises.
A pseudo hernia is defined as ‘bulging of the abdominal wall that is not caused by structural defects, collection of fluid, or a mass but, rather, muscle paralysis.’2 Common causes include diabetic radiculoneuropathy, trauma or ventral root injury. Pseudo hernia due to HZ occurs in 0.17% of the cases and is a rare complication.3 It occurs most commonly in middle-aged to elderly, obese individuals and has been seen to commonly involve the T11 dermatome.4 This muscle paralysis is hypothesised to occur as a result of the direct spread of the virus from the dorsal root ganglia to the ventral horn cells and motor nerve roots.2,3 The prognosis is generally favourable with full clinical recovery in 55–78% of cases.5,6 This entity has been described in very few dermatological journals. Since many cases come for follow up to the dermatology clinic, it is important to keep in mind the risk of developing pseudo-hernias in elderly individuals. Keen observation and detailed history can help in the clinical diagnosis of this condition, thus avoiding unnecessary diagnostic studies and surgical intervention. Watchful waiting is the best therapeutic option for such cases along with abdominal strengthening exercises.
Conflict of interestsThe authors declare that they have no conflict of interest.