Eosinophilic fasciitis is a rare scleroderma-like disorder that mainly affects the muscle fascia. It usually occurs in adults between the ages of 20 years and 70 years.1
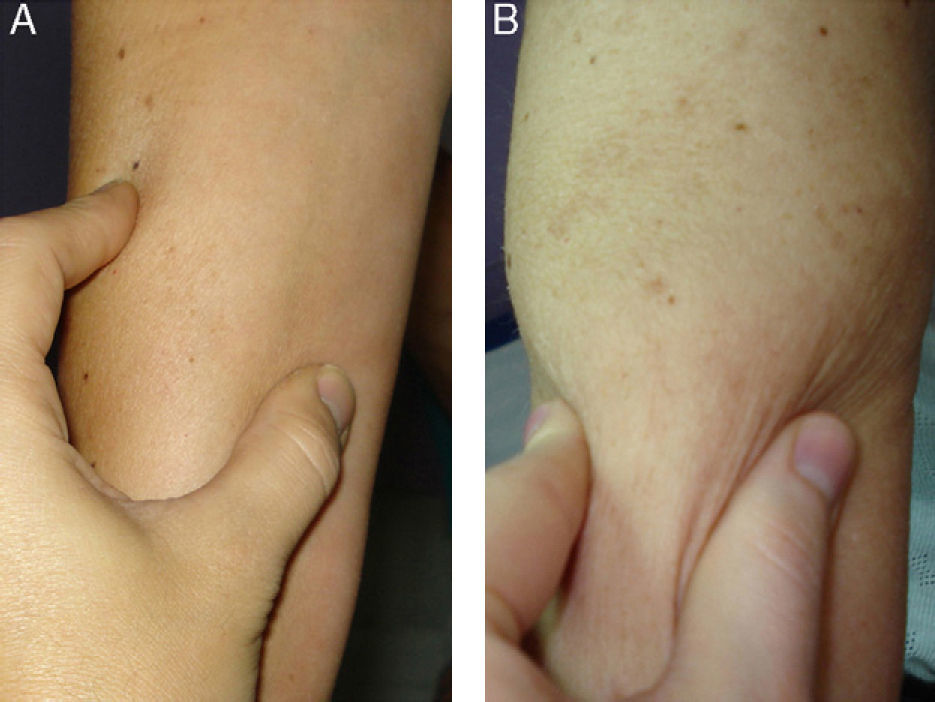
We present the case of a 54-year-old patient with no past medical history of interest, who came to the clinic because of a rapidly progressive induration of the limbs, abdomen and lower back 1 month after an accidental fall (Fig. 1A). The condition had started as edema and erythema of the lower limbs, spreading to other areas, with the subsequent appearance of induration. The diagnoses considered were eosinophilic fasciitis, scleroderma, scleredema, and scleromyxedema. The patient did not present Raynaud phenomenon, dysphagia, or sclerodactyly.
Complete blood count showed a raised white cell count with marked eosinophilia (3.10×103/μL, 22%). Other laboratory tests, including the erythrocyte sedimentation rate, antinuclear antibodies and rheumatoid factor, were normal or negative.
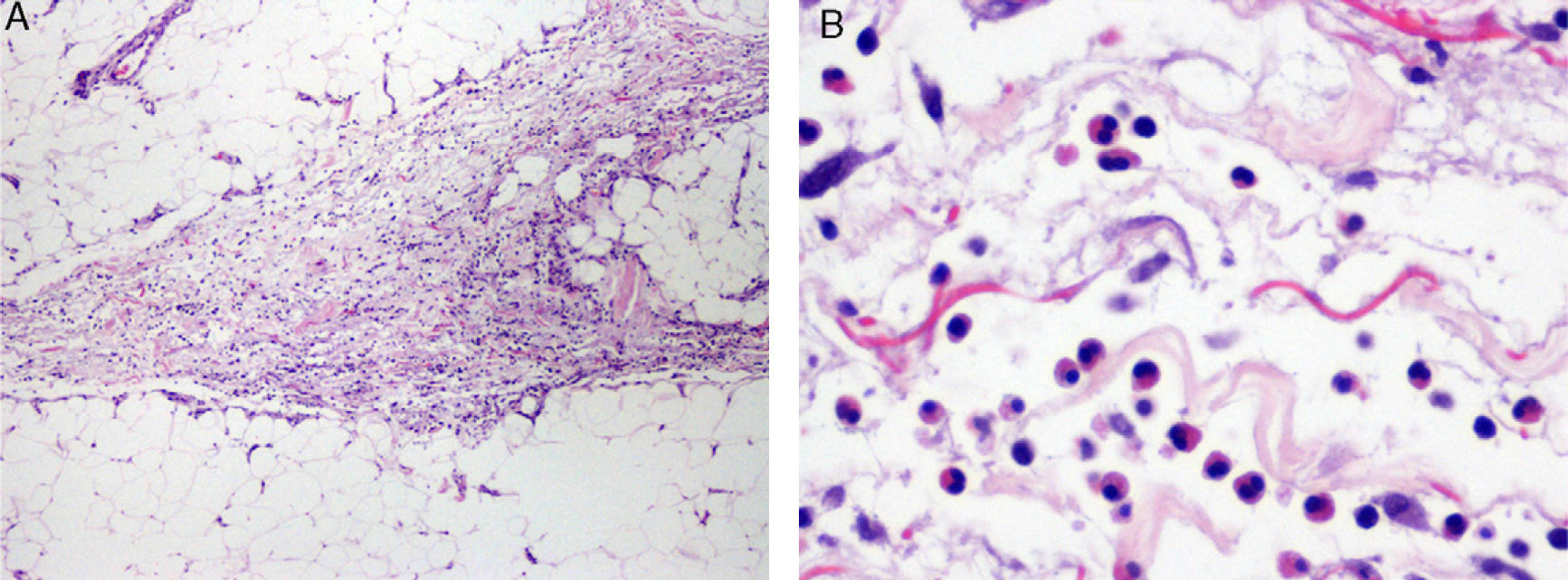
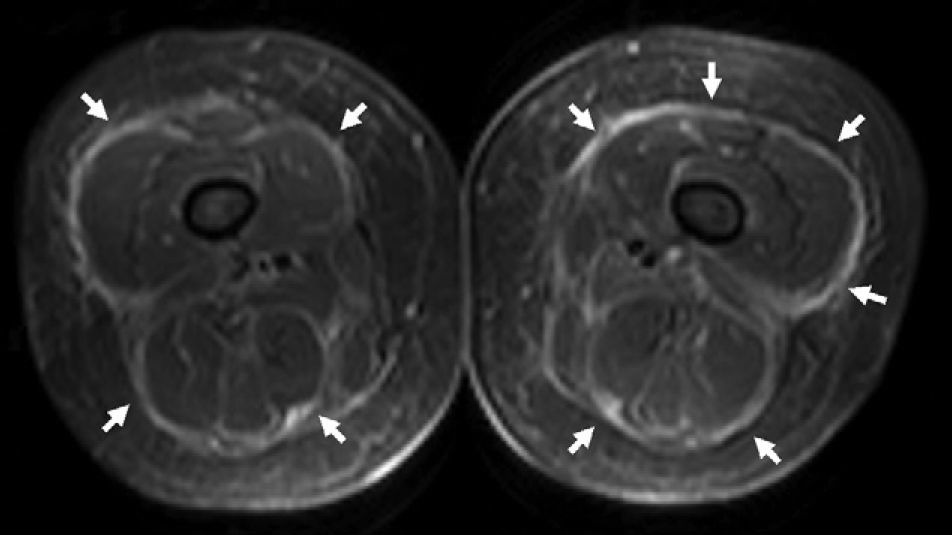
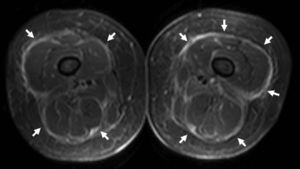
Histopathology of a deep biopsy of the forearm showed interlobular septal thickening and an inflammatory infiltrate with numerous eosinophils affecting the septa and adjacent subcutaneous tissue, which was moderately edematous (Fig. 2). There were no changes of note in the epidermis and dermis; the muscle fascia could not be assessed. Magnetic resonance imaging (MRI) of the lower limbs showed thickening of the muscle fascia with signal hyperintensity on short TI inversion recovery sequences, indicating inflammation (Fig. 3).
Histopathology image of biopsy sample from the forearm. A, Interlobular septal thickening in the subcutaneous cellular tissue with inflammatory cells (hematoxylin-eosin, original magnification ×40). B, Higher magnification reveals the presence of numerous eosinophils in the subcutaneous cellular tissue adjacent to the septa (hematoxylin-eosin, original magnification ×400).
The patient was diagnosed with eosinophilic fasciitis on the basis of the peripheral eosinophilia, histological findings, and the fasciitis observed on MRI. Treatment was initiated with oral prednisone at a dose of 1mg/kg/d and hydroxychloroquine, with the subsequent addition of methotrexate to reduce the necessary dose of corticosteroids. The clinical course was favorable, with blood parameters returning to normal at 2 months and disappearance of the induration after 12 months of treatment (Fig. 1B).
Eosinophilic fasciitis was first described by Shulman in 1974 in patients with diffuse fasciitis and peripheral eosinophilia; it is clinically characterized by induration of the subcutaneous tissues, predominately affecting the limbs, preceded by an initial stage involving erythema and edema.1,2 Peripheral eosinophilia is a typical finding and is present in up to 80% of cases.1 In general, there is no visceral involvement, Raynaud phenomenon, or sclerodactyly.2
Its appearance has been associated with various triggers such as extreme physical exercise, insect bites, Borrelia infection, and the use of certain drugs such as statins. Toxic oil syndrome caused by adulterated rapeseed oil has also been associated with the disorder.1–4 To date, only 5 cases have been reported following an uncomplicated trauma.2,5,6 In our case, the close temporal association with the accidental fall and the absence of other predisposing factors suggests that this was the trigger. A similar case has been described in the literature, in which eosinophilic fasciitis developed 1 week after a fall.5 It has been suggested that in these patients the trauma could reveal antigenic properties of the fascia and subcutis, thus initiating the process.2If eosinophilic fasciitis is suspected, a full-thickness biopsy is needed to determine whether the muscle fascia is affected.2 Histology shows fibrous thickening of the fascia with a diffuse lymphoplasmocytic inflammatory infiltrate and varying numbers of eosinophils. These changes often extend locally into the interlobular septa of the adjacent adipose tissue and into the muscle layers.1–3
The role of MRI has become of increasing importance in the diagnosis of eosinophilic fasciitis and in its follow-up.7–10 Characteristic findings include thickening and increased signal intensity of the muscle fascia on T2-weighted and short T1 inversion recovery sequences, with enhancement following administration of contrast material on T1-weighted sequences; these changes correspond to the degree of microscopic inflammation.8,10
However, in some patients the biopsy is suboptimal or cannot be performed, and thus the findings from MRI are used to identify involvement of the fascia and reach a diagnosis.7,9 Our case provides a novel example of eosinophilic fasciitis that was diagnosed by MRI after biopsy proved inconclusive.
Therefore, although biopsy remains the diagnostic procedure of choice, MRI can be very useful to confirm inflammation of the muscle fascia in cases in which this cannot be assessed on the biopsy or when the findings are inconclusive.7,9 In addition, by confirming that the process mainly affects the fascia, MRI helps to distinguish eosinophilic fasciitis from other disorders such as polymyositis or scleroderma.10
Attention has also been drawn to its usefulness when selecting the optimal area from which to take a biopsy, and to identify improvement in fascial inflammation after starting treatment.8,10
In conclusion, the case presented demonstrates the usefulness of MRI in establishing a diagnosis of eosinophilic fasciitis in patients when histopathological findings are inconclusive. In addition, a history of an accidental fall in the absence of other precipitating factors supports the role of trauma as a possible trigger of the disease.
Please cite this article as: Armengot-Carbó M, et al. Fascitis eosinofílica asociada a traumatismo: utilidad diagnóstica de la resonancia magnética. Actas Dermosifiliogr.2011;102:641-2.