The prevalence of psoriasis in Spain was estimated to be 1.4% before the advent of biologic agents. Fifteen years later, new therapeutic options based on biologic agents have led to greater awareness of the disease and better understanding; case detection and diagnosis may have improved as a result.
ObjectiveTo investigate the current prevalence of psoriasis in Spain and compare the results with those of an earlier study that used the same methodology.
Material and methodsPopulation-based cross-sectional survey. Information was collected through computer-assisted telephone interviews with a randomly selected representative sample of the Spanish population (12,711 individuals from 4,754 households). Interviews were conducted by trained personnel using a questionnaire.
ResultsThe prevalence was 2.3% and there were no statistically significant differences between the sexes. Prevalence increased with age (range with highest prevalence, 60-69 years). Central Spain—a region with a cold, dry climate—had the highest prevalence, but differences between regions were not significant.
ConclusionsPsoriasis is substantially more prevalent in Spain than was previously estimated. The increase in prevalence may reflect greater awareness and better diagnosis of the disease rather than a true increase in number of cases.
La prevalencia de la psoriasis en España en la era prebiológica se estimó en el 1,4%. Quince años después la amplia difusión y mejor conocimiento de la enfermedad, generada por las nuevas perspectivas terapéuticas aportadas por los agentes biológicos, pueden haber mejorado el diagnóstico e identificación de la enfermedad.
ObjetivoInvestigar la prevalencia de la psoriasis en España en el momento actual y comparar los resultados con los obtenidos en un estudio previo realizado con la misma metodología.
Material y métodosEstudio transversal de base poblacional, utilizando como fuente primaria de información el individuo, a través de una muestra estrictamente aleatoria y representativa de la población española (12.711 sujetos de 4.754 hogares) con recogida de información a través de una entrevista telefónica asistida por ordenador realizada por personal entrenado y utilizando un cuestionario predeterminado.
ResultadosLa prevalencia estimada fue del 2,3%, sin diferencias estadísticamente significativas entre sexos. La prevalencia en los distintos grupos de edad siguió una curva ascendente hasta los 60-69 años. La prevalencia más alta correspondió a la zona central del país de clima frío y seco, aunque sin diferencias significativas con otras regiones.
ConclusionesLa cifra de prevalencia de la psoriasis en España es sensiblemente superior a la estimada en estudios previos. Este incremento podría reflejar un mejor conocimiento y diagnóstico de la enfermedad más que un aumento real de la prevalencia.
The prevalence of a specific skin disease is very important: it enables us to prioritize resources, favors the design of epidemiological and clinical studies, and makes it possible to calculate the impact of the disease and its treatment on costs.1
The results of a study performed 15 years ago showed the prevalence of psoriasis in Spain to be 1.4%.2 In the last 10 years, the advent of biologics has revolutionized the treatment of psoriasis by improving the outlook for safety and efficacy with respect to previous treatments.3 The widespread use and acceptance of these new therapeutic options, which have developed in line with knowledge of the pathogenesis of the disease, are reflected in the exponential growth in information on psoriasis in both the scientific literature and the general press. Consequently, the number of visits for psoriasis has increased, the disease is more easily recognized in primary care, and access to specialists has improved.
We performed a study of the prevalence of psoriasis in the Spanish population. We also investigated variations according to sex, age group, and geographic distribution (autonomous communities) by comparing our findings with those of the first study on psoriasis in Spain, which was performed 15 years ago,2 immediately after the advent of biologics.
Material and MethodsThe study was performed following the design of population studies and health surveys, that is, by interview. We performed a population-based cross-sectional study using the individual as the primary source of information. The sample was strictly random and representative of the Spanish population. The study was performed between May 21 and September 23, 2013 with the help of the market research company Demométrica Investigación de Mercados y Opinión Pública, Madrid, Spain. Demométrica collected the data according to the requirements for processing and custody of data in Spain's Organic Law on the protection of personal data.
The target population comprised households in Spain. No age limit was imposed, and information was collected by computer-assisted telephone interview. Data were entered into a computerized database, and the results were expressed as absolute values and percentages.
By assuming a prevalence of psoriasis of approximately 2%, we calculated the initial sample size to be 4750 households, which were randomly selected from each stratum of the autonomous community and habitat.
Stratified random sampling was used. The main criterion for stratification was the geographic area (autonomous community, 17 strata) and the size of the town of residence (5 strata: <10 000 inhabitants, 10 000 to 50 000 inhabitants, 50 000 to 100 000 inhabitants, 100 000 to 500 000 inhabitants, and>500 000 inhabitants). Sample allocation was proportional to the size of the population in each stratum formed by the cross between autonomous community and size of the town. The unit of analysis was the household.
The head of the household, his/her partner, or another valid person was contacted to record the age, sex, educational level, and employment status of each member of the household. Cases of psoriasis were then identified by an affirmative response to the following question: “Could you tell me whether any member of your household has been diagnosed with a disease called psoriasis by a doctor?” Each person identified as a valid case of psoriasis answered a specific predetermined questionnaire to ascertain the following: type of specialist who diagnosed the disease (dermatologist, general practitioner, or other), characteristics of the disease (type of psoriasis, age at onset, location of the lesions, degree of activity, severity, treatment received, and response to treatment), and impact of the disease on quality of life using the Dermatology Life Quality Index. This phase of the interview only applied to the person diagnosed with psoriasis. Responses were not permitted from other members of the household. If the person diagnosed with psoriasis was a minor, the father, mother, or guardian was interviewed.
If the response to the first question was negative, the interviewee received a description of the signs of the disease as “reddish patches or excessive flaking of the skin mainly on the elbows, knees, or scalp” and was asked whether any member of the household had had any of these signs during the previous 12 months. If the answer was “yes,” the person was asked whether he/she had visited the doctor, and, if the answer was “yes” again, the patient was asked what diagnosis was made.
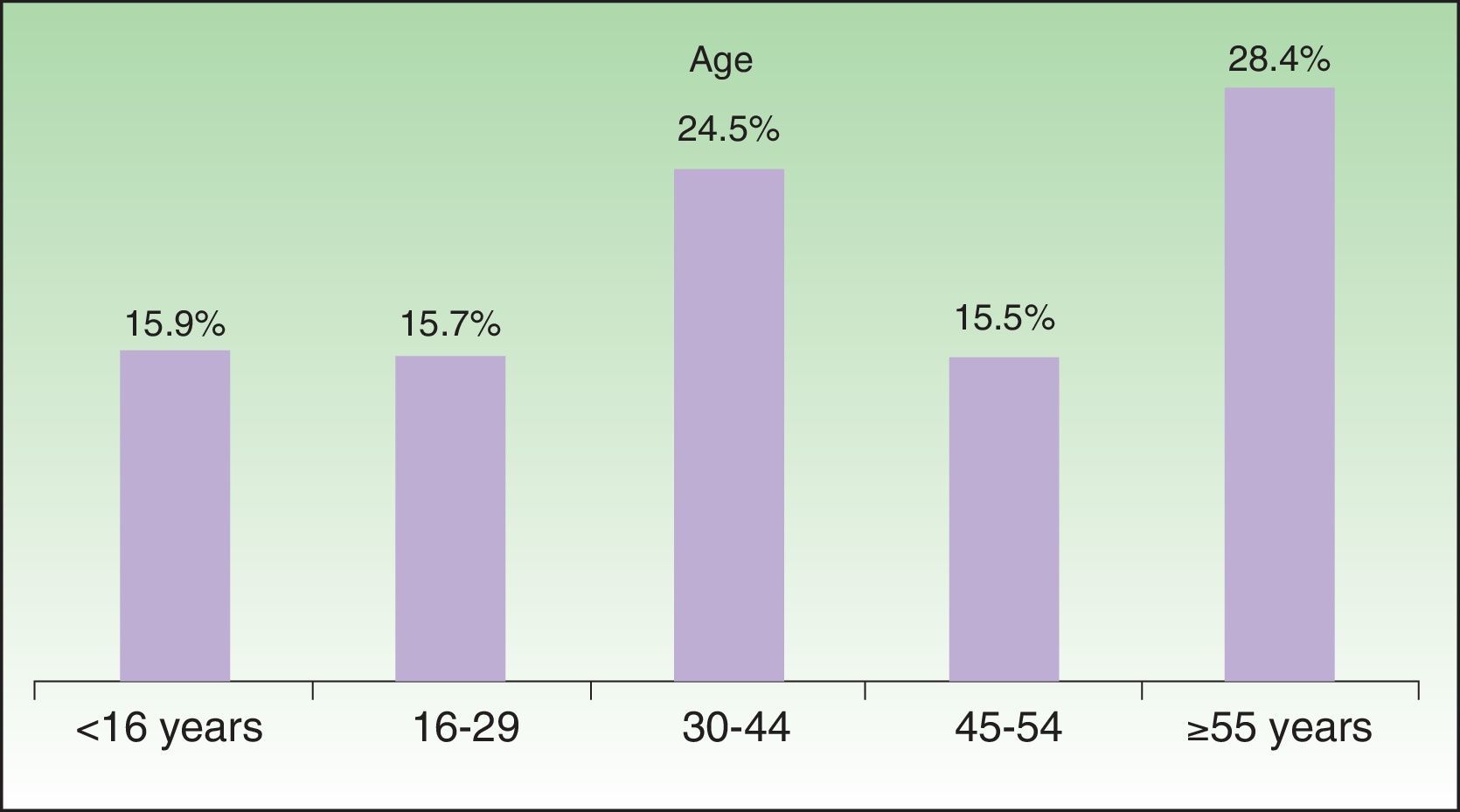
ResultsThe final valid sample comprised 4754 households with a mean size of 2.7 persons per household and a total of 12 711 persons (57.5% were male and 42.5% were female). The distribution by age group is shown in Figure 1. The sample is representative of the Spanish population, with no differences in terms of age or sex.
Psoriasis was diagnosed by a physician in 307 cases (70% by a dermatologist, 28% by a family physician, and 2% by another specialist or a doctor whose specialty the patient could not remember).
Of these 307 persons with psoriasis, 294 subsequently replied to the specific questionnaire on the characteristics of the disease and perceived quality of life. The calculation of prevalence was performed using only these 294 persons.
Based on these data and the calculations performed during the design of the study, prevalence was estimated at 2.3% (95% confidence interval [CI], 2.0-2.6). An additional 2.5% of interviewees answered “yes” to the question on the signs of the disease (patches or excessive flaking of the skin on the elbows, knees, or scalp), even when they denied having received a medical diagnosis of psoriasis. However, 2% had seen a doctor and been diagnosed with a skin disease other than psoriasis. The remaining 0.5% reported that they had never seen a doctor and, therefore, did not have a diagnosis; they were not included in the calculation of prevalence.
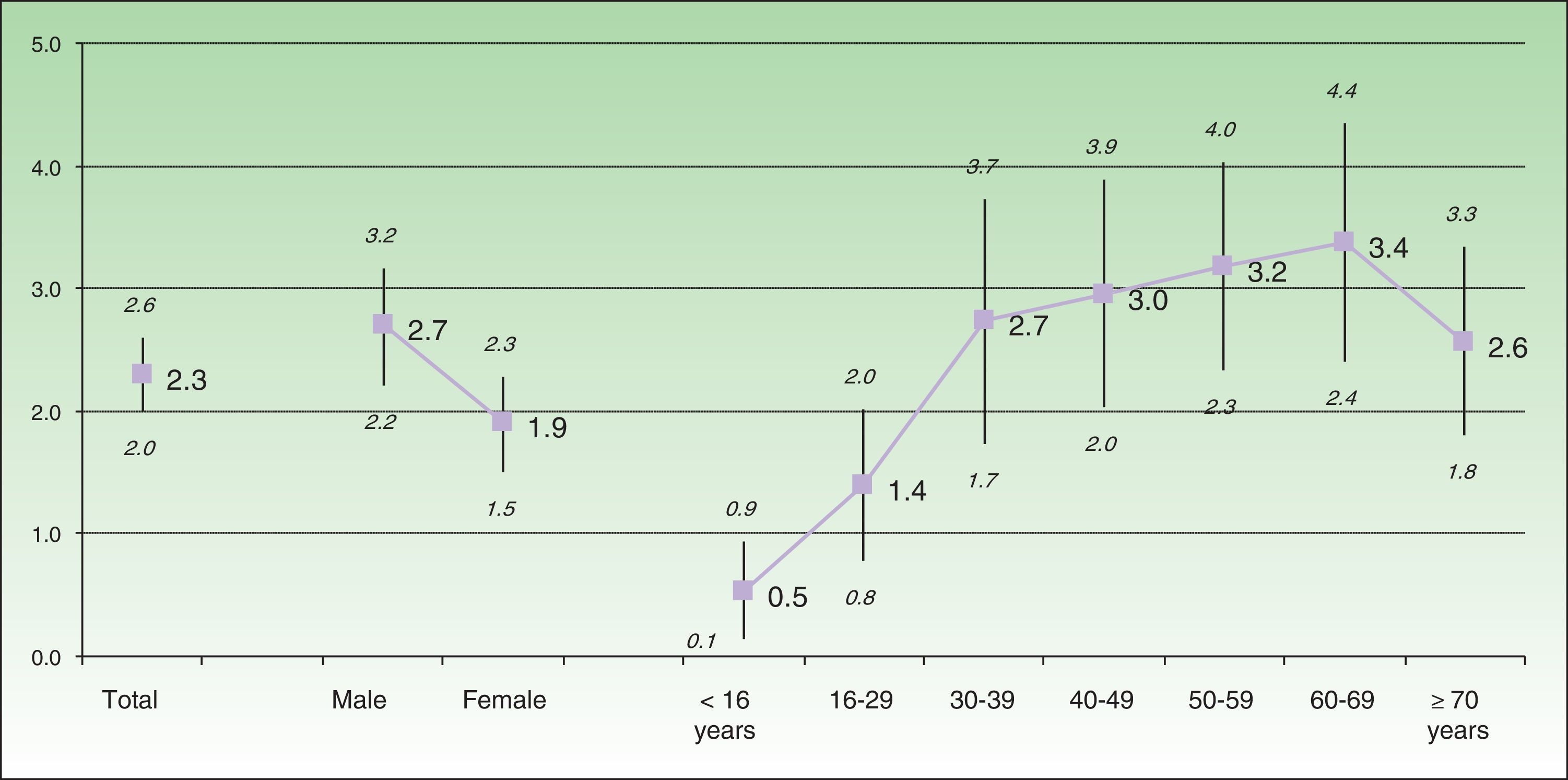
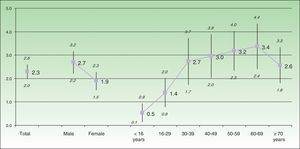
The estimated prevalence was greater for males (2.7% [95% CI, 2.2%-3.2%]) than for females (1.9% [95% CI, 1.5%-2.3%]), with differences in the limit of statistical significance. Figure 2 presents the differences in prevalence between the age groups by decade. Values increase until 60-69 years, when they start to decrease.
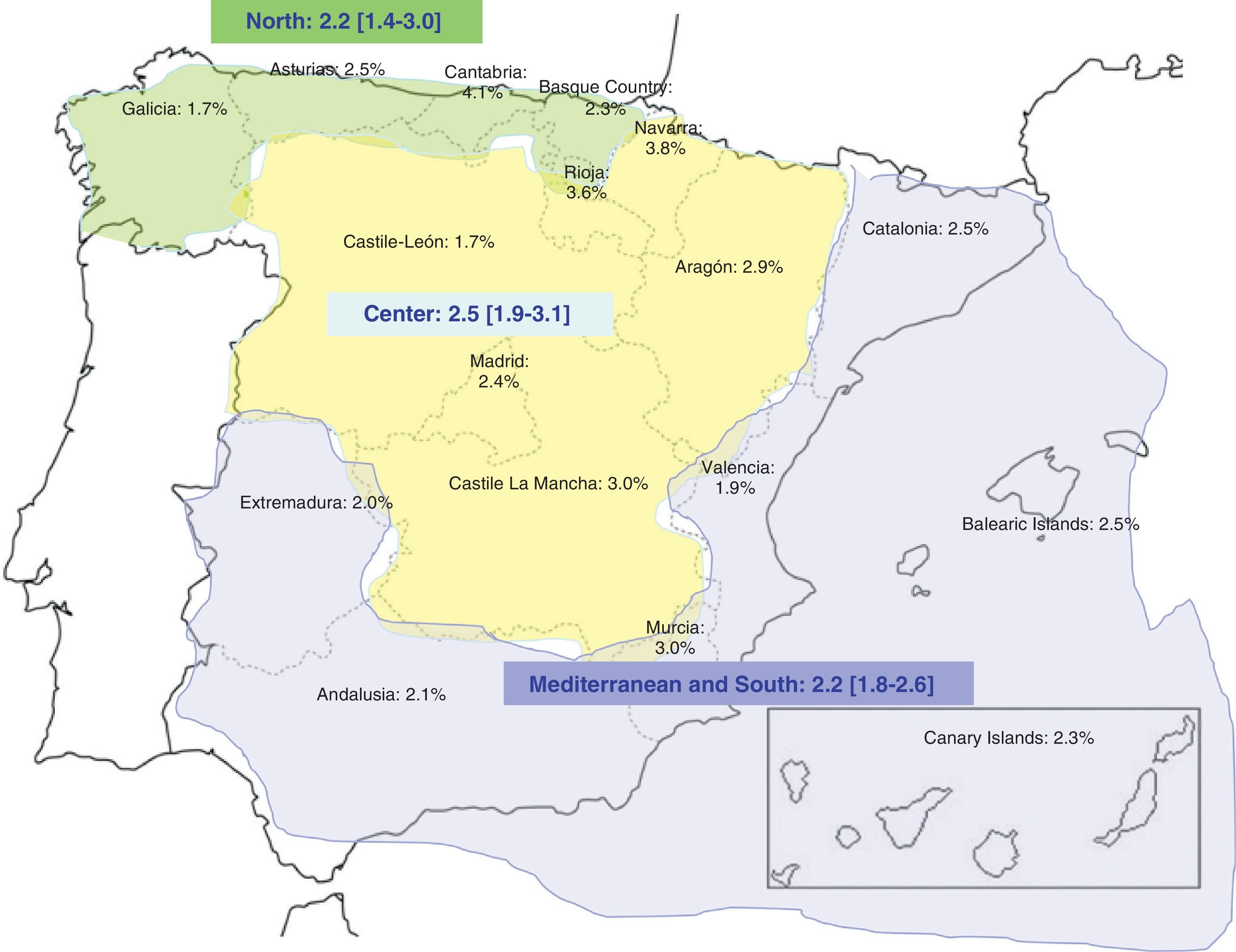
Figure 3 shows the prevalence by autonomous community. Values ranged from 1.7% in Castile-León and Galicia to 4.1% in Cantabria. If we group the autonomous communities into 3 regions according to climate (Mediterranean and south, temperate climate [Canary Islands, Andalusia, Extremadura, Murcia, Valencia, Catalonia, and Balearic Islands]; center, dry and cold climate [Aragón, Castile-León, Castile-La Mancha, Navarre, and La Rioja]; and north, wet and cold climate [Asturias, Cantabria, Galicia, Basque Country]), the estimated prevalence was 2.2%, 2.5%, and 2.2%, respectively, with no statistically significant differences between the regions.
DiscussionThe world prevalence of psoriasis stands at about 2%; however, figures vary widely between countries and geographical areas.4
In addition to the influence of genetic, racial, climatic, and environmental differences, the variation in findings is clearly affected by the different study methodologies applied (questionnaires, clinical examination, combination of questionnaire and clinical examination, registry data), the type of prevalence studied (point prevalence, period prevalence, cumulative prevalence), the characteristics of the study sample (eg, children only, adults only, and any age group), and the case definition (self-reported, physician-diagnosed).
The present study is based on a representative sample of the Spanish population with no age restrictions. The study was performed following the design of population studies and health surveys, that is, by interview. In studies of this type, the quality of the data depends essentially on the observer, the content, and the source used. The estimated prevalence obtained, 2.3%, indicates that around 1 080 000 persons in Spain have been diagnosed with psoriasis.
The methodology applied is subject to a series of limitations. First, it is important to take into account reporting bias—some patients do not know they have the disease, others do know but deny having it—which is common in skin diseases; this limitation is inherent to the method used and cannot be quantified. Second, the study is also subject to classification bias, since the disease is not reported spontaneously by the patient, but only when he/she is asked whether they have physician-diagnosed psoriasis. Nevertheless, the reliability and validity of the results are guaranteed by the sample size and reinforced by the fact that the informant was always the head of the household or the homemaker. In addition, almost all those cases reported as “physician-diagnosed psoriasis” (293 of 307 [95.4%]) were subsequently interviewed using a specific questionnaire on the clinical and epidemiologic characteristics of the disease and their perceived quality of life. Thus, the final prevalence value includes only those persons with physician-diagnosed psoriasis who had responded to the disease-specific questionnaire. In other words, the first contact served as a screening stage and was later contrasted with the person diagnosed with psoriasis.
The results of population-based studies in Europe similar to the present study and including persons of all ages show that cumulative prevalence varies between 0.7% in Scotland5 and 2.9% in Italy,6 with most countries having a prevalence greater than 1%.7 These figures are consistent with those found in the present study.
In contrast, a noteworthy difference was found between the data reported here and those recorded in Spain using a similar methodology 15 years ago, when the estimated prevalence was 1.4%.2 Such a large difference in only 15 years cannot be accounted for by the increasing trend in the incidence of psoriasis reported elsewhere8 or in its prevalence, as reported in the United States of America9 and in some European countries.10 Thus, in Norway, the prevalence doubled in an adult cohort followed for 30 years (1979-2008).10 The increased prevalence of psoriasis in a single country has also been pointed out in recent comparisons between previous studies, although in these cases it can be attributed, at least in part, to the different methodologies used.11,12
Our methodology was almost identical to that of the previous study; the diagnostic criteria of the disease have not changed in recent decades, and it would be very difficult to maintain that changes in lifestyle and environmental factors have contributed to an increase in prevalence in such a short time. Although the increase may not be real, it could reflect greater awareness of the disease among physicians and the general public. In this sense, perhaps the most important contributing factor is the development and widespread prescription of biologic agents and their efficacy in treating psoriasis. The increasing use of health care services by the population may also have played a role, albeit a smaller one.
The development of biologics has led to numerous scientific publications and general press articles, as well as refresher courses for dermatologists, family and community medicine physicians, and pharmacists. All of these professionals have considerably improved their knowledge of psoriasis, its diagnosis, and therapeutic options. Consequently, many cases of psoriasis that once went undiagnosed and remained abandoned owing to the lack of genuinely efficacious treatment are now visible. Cases not reported by the patient because of the fear of incomprehension of their disease and the paucity of therapeutic options could also be taken into consideration.13
Prevalence was higher in men than in women; this was not the case in the study performed in 2001,2 where prevalence was similar in both sexes, as in most of the population-based studies that do not apply age restrictions.7,14 However, this difference between the sexes did not reach statistical significance, although it came very close. Few studies of this type have shown statistically significant differences in one sense or another.15,16
Since life expectancy is only affected by severe forms of psoriasis, prevalence increased continuously, as expected, from the age of 16 years, with values greater than 2.5% after 30 years until 60-69 years, when it began to decrease. The bimodal distribution in age at onset17 and the increase in late-onset psoriasis highlighted in the literature8 could play a role in this increased prevalence in older age groups. However, a careful analysis of the prevalence and confidence intervals found for the different age groups in our study reveals a certain degree of stability between 40 and 69 years, although an increasing tendency that is not statistically significant is observed. These findings are closer to those of the previous study, in which the maximum prevalence was found in patients aged 30 to 40 years.2
The prevalence between the different autonomous communities varied between 1.7% in Castile-León and Galicia and 4.1% in Cantabria. However, prevalence was greater than 3% in only 3 autonomous communities, which were those whose sample comprised fewer than 200 interviews (Cantabria, Navarre, and La Rioja). In these cases, estimation of prevalence is subject to high sampling error; therefore, the results should be interpreted with extreme caution. The nonhomogeneous distribution of prevalence between the different regions of a single country, which is observed mainly in studies from the north of Europe, has been attributed to genetic differences and climatic factors.15,18 Given that it is difficult to determine such differences between the various Spanish autonomous communities, we grouped autonomous communities into 3 large regions according to their common climatic characteristics. The highest prevalence (2.5%) was observed in the central region, which has a dry and cold climate, although the difference between this region and the other 2 regions, which had a similar prevalence, was not statistically significant.
This increase of 0.9 percentage points in the prevalence of psoriasis in Spain could have major cost repercussions for the National Health System, considering that it occurred alongside the advent of biologic therapy. It is also important to remember that 20% to 30% of patients with moderate-to-severe psoriasis will require systemic treatment and that many of them will be prescribed biologics during the course of their disease, since the threshold doses after which the risk of organ-specific toxicity becomes considerable are reached in just a few years with traditional systemic treatment. The cost of comorbid conditions associated with moderate-to-severe psoriasis must also be taken into account.19
In conclusion, 2 similar studies (one performed in 1998, immediately before the advent of biologics, and the other 15 years later in 2013) show markedly different values for overall prevalence in Spain. Nevertheless, the comparison of values between age groups and between geographic areas classified according to climate suggests that prevalence remains unchanged.
The increase in prevalence could probably be attributed to the greater visibility of existing cases of psoriasis through comprehensive coverage of the disease in the specialized and general press as a result of widespread use of biologics and appreciation of their therapeutic potential. The increase could also be attributed to better knowledge of the disease among nonspecialist physicians and increased awareness among patients.
Ethical DisclosuresProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors are grateful to Janssen Cilag for sponsoring the collection and processing of data. The authors confirm that Janssen Cilag did not participate in the preparation of this manuscript.
Please cite this article as: Ferrándiz C, Carrascosa JM, Toro M. Prevalencia de la psoriasis en España en la era de los agentes biológicos. Actas Dermosifiliogr. 2014;105:504–509.