Benign skin lesions are a common reason for visits to primary care physicians and dermatologists. However, access to diagnosis and treatment for these lesions varies considerably between users, primarily because no explicit or standardized criteria for dealing with these patients have been defined. Principally with a view to reducing this variability in the care of patients with benign cysts or tumors, the Andalusian Regional Section of the Spanish Academy of Dermatology and Venereology (AEDV) has created a Process of Care document that describes a clinical pathway and quality-of-care characteristics for each action. This report also makes recommendations for decision-making with respect to lesions of this type.
Las lesiones cutáneas benignas representan un motivo de consulta frecuente, tanto en atención primaria como en las consultas de dermatología. Sin embargo, existe una amplia variabilidad en el acceso de los usuarios al diagnóstico y tratamiento de las lesiones cutáneas benignas, debido principalmente a que no se establecieron criterios explícitos y homogéneos para el abordaje de los pacientes con lesiones benignas. Con el objetivo principal de reducir la variabilidad en la atención a las personas con lesiones quísticas o tumorales benignas la Sección Territorial Andaluza de la AEDV ha desarrollado un proceso de atención en el que se describen el recorrido del paciente, las características de calidad de las actuaciones y las recomendaciones para la toma de decisiones en este tipo de lesiones.
Benign skin lesions are a common reason patients consult both primary care physicians and dermatologists. The impact of these consultations on caseloads in public medicine has not been studied in depth, but Macaya and coworkers1 did report that 25% of visits to a dermatologist were related to requests for aesthetic procedures for acrochordons, intradermal melanocytic nevi, seborrheic keratoses without inflammation, solar lentigines, ruby points, or wrinkles. We note that lesions of this type potentially generate a high level of demand for services: melanocytic nevi, for example, can be present in 100% of patient populations.
Minor outpatient surgery has been included in the portfolio of services provided at the primary care level during the last 10 years. At the same time, priority has been placed on oncologic processes at the level of hospital care, and as a result the organization and function of health care services have had to be redesigned. Clients’ access to diagnostic and therapeutic procedures for benign skin lesions has therefore come to vary greatly across the system, mainly because explicit, standardized criteria have not been established to guide the handling of these cases.2,3 In the absence of clinical criteria, some centers have applied Royal Decree 63/1995 on the organization of health care services in the Spanish National Health Service (NHS). Article 2.3c of that decree states that “attention, care, or services to improve aesthetic or cosmetic problems shall not be covered.”4,5 Later, Royal Decree 1030/2006 established a portfolio of common NHS services and the procedures for updating the list; among the exclusions from that portfolio were therapies “such as the use of waters, spas, or residential facilities or similar that are directed toward leisure activities, recreation, comfort, sports or aesthetic or cosmetic improvements.”6 In any case, from the clinical and organizational point of view, this normative framework should be reflected explicitly in the clinical pathway that patients follow and the decisions taken in specific situations at each care level (in primary care centers and clinical management units [CMUs] for dermatology).
In addition to the issue of variability of access to services, and the consequent risk of unequal care, there is also a clinical concern of particular importance: some types of benign lesions are especially difficult to diagnose, notably with respect to distinguishing benign melanocytic lesions from melanoma. This consideration should be reflected in any guidelines or recommendations intended to standardize the care of persons presenting with benign skin lesions.
In 2014, the Andalusian Regional Section of the Spanish Academy of Dermatology and Venereology (AEDV) created a working group to develop a portfolio of services for application by CMUs coordinating medical and surgical procedures in dermatology and sexually transmitted infections within the Andalusian NHS.7 The first step in the portfolio's development process consisted of defining functional units (nonmelanoma skin cancer, psoriasis, melanoma, sexually transmitted infections, etc.) and areas of care (general dermatology, dermatologic surgery, etc.). Next, relevant diseases were identified and grouped under the functional units, and the diagnostic and/or therapeutic procedures undertaken by dermatologists at each organizational level were specified. Finally, care processes were identified or developed for conditions that had priority or those for which no documentary support was in place (namely atopic dermatitis, urticaria, sexually transmitted infections, and benign cysts or tumors).
The Care Process: Concept and ObjectivesA document describing a care process, or clinical pathway, specifies the who-when-where-how governing a patient's receipt of care for a condition or a set of related ones. The document lists each intervention or other process required for care, situating them sequentially in time and throughout the pathway the patient follows during the various phases of a disease. It also identifies the professionals responsible for care at each point. The main reason for organizing and describing a care process is to ensure continuity of care at all times regardless of which primary- or tertiary-care professionals might be involved. Incorporated into the description will be aspects and dimensions of quality of care, such as clinical efficacy, safety, and the provision of information for patients or their caregivers. The main components of a documented care process are as follows: the patient's clinical pathway, quality-of-care criteria for interventions, critical safety points (CSPs), and indicators for monitoring quality.8
Persons with benign cysts or tumors are not homogeneous: they seek care through a variety of routes, have various motivations, and have seen different types of health care professionals about their problem. However, the present care process plan focuses on arriving at consensus in making decisions and treating patients in primary care centers and CMUs for dermatology, given the degree to which these 2 settings are currently at the opposite poles of care management.
Thus, the main purpose in planning this patient care process is to limit variability in how we attend persons with benign cysts or tumors, through the application of consensus-based recommendations endorsed by the Andalusian Regional Section of the AEDV. To meet that aim we applied the following precepts of the Fourth Andalusian Health Plan9:
- •
Seek to have an effect on health, avoiding therapeutic interventions that have no benefits on individual or public health.
- •
Pursue efficiency, giving priority to actions that have an effect on health and disregarding those with no intrinsic value.
- •
Respond to the demands of clients in the immediate and surrounding communities whenever possible.
Finally, rather than serving to restrict access to services, care process planning for persons with benign cysts or tumors should aim to guarantee that patients receive all procedures required for a proper diagnosis and that treatment is recommended whenever it is indicated.
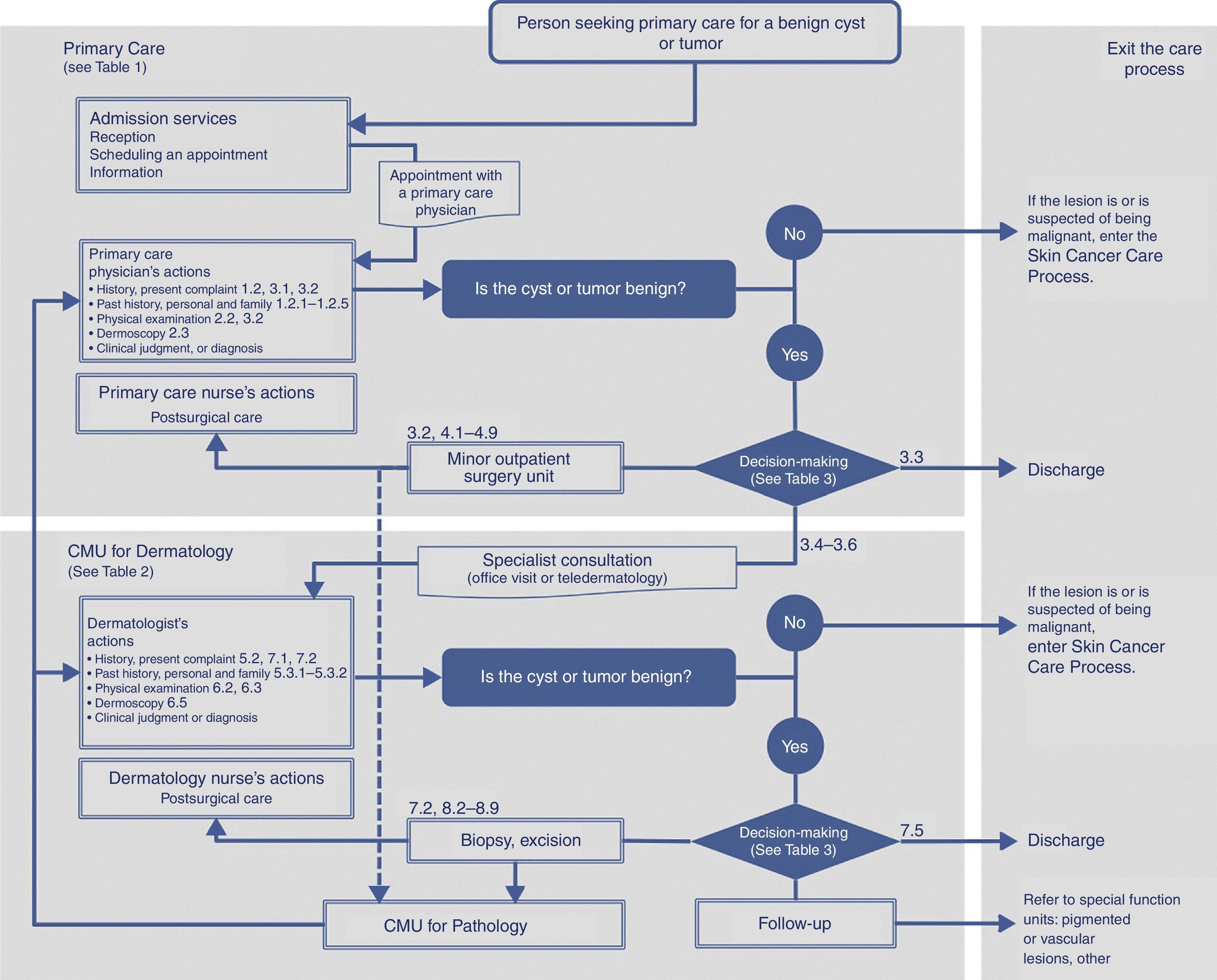
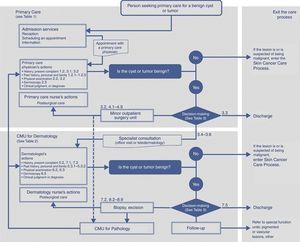
The Clinical Pathway and Characteristics Relevant to Quality of Care and Decision-MakingThe stages in care for persons with benign lesions and the settings where care takes place are shown in Figure 1. More complete information about the clinical pathway these patients follow is presented in Tables 1 and 2, which describe steps to take in primary care centers and dermatology CMUs, respectively. The quality-of-care characteristics mentioned in the tables cover such actions as taking the patient's medical history and performing a physical examination. Also identified are the CSPs listed by the health service of the government of Andalusia (the Junta),10 along with aspects relevant to adequately informing patients or their caregivers.
Clinical pathway showing how the patient with a benign cyst or tumor moves through the various care settings. Numerical references refer to Tables 1 or 2, which list quality-of-care characteristics to apply in primary care centers and dermatology CMUs, respectively. Patients treated in a minor outpatient surgery unit or in the dermatology CMU will be referred back to the family practitioner or dermatologist at the primary care center who first attended the patient so that the referring physician can see the results of pathologic examination. CMU refers to clinical management unit.
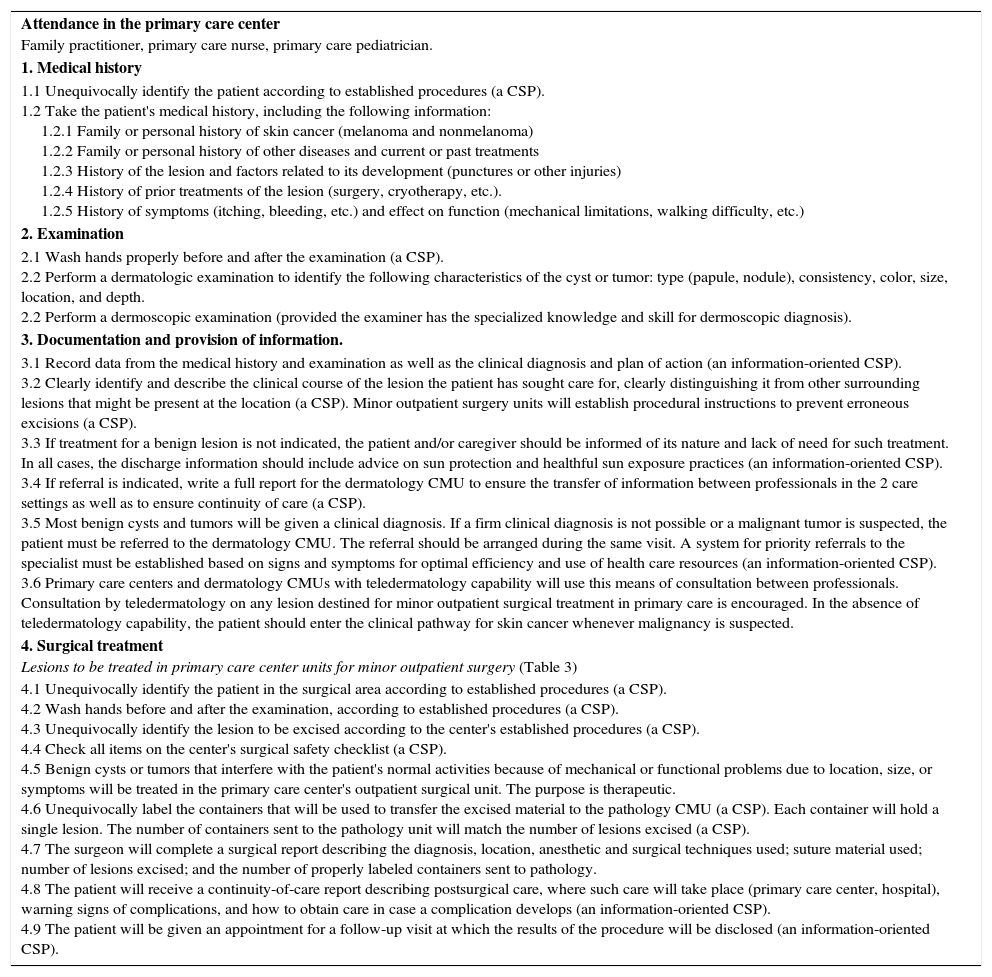
Quality-of-Care Characteristics to Apply When Attending Persons With Benign Cysts or Tumors in Primary Care Centers.
| Attendance in the primary care center Family practitioner, primary care nurse, primary care pediatrician. |
| 1. Medical history |
| 1.1 Unequivocally identify the patient according to established procedures (a CSP). 1.2 Take the patient's medical history, including the following information: 1.2.1 Family or personal history of skin cancer (melanoma and nonmelanoma) 1.2.2 Family or personal history of other diseases and current or past treatments 1.2.3 History of the lesion and factors related to its development (punctures or other injuries) 1.2.4 History of prior treatments of the lesion (surgery, cryotherapy, etc.). 1.2.5 History of symptoms (itching, bleeding, etc.) and effect on function (mechanical limitations, walking difficulty, etc.) |
| 2. Examination |
| 2.1 Wash hands properly before and after the examination (a CSP). 2.2 Perform a dermatologic examination to identify the following characteristics of the cyst or tumor: type (papule, nodule), consistency, color, size, location, and depth. 2.2 Perform a dermoscopic examination (provided the examiner has the specialized knowledge and skill for dermoscopic diagnosis). |
| 3. Documentation and provision of information. |
| 3.1 Record data from the medical history and examination as well as the clinical diagnosis and plan of action (an information-oriented CSP). 3.2 Clearly identify and describe the clinical course of the lesion the patient has sought care for, clearly distinguishing it from other surrounding lesions that might be present at the location (a CSP). Minor outpatient surgery units will establish procedural instructions to prevent erroneous excisions (a CSP). 3.3 If treatment for a benign lesion is not indicated, the patient and/or caregiver should be informed of its nature and lack of need for such treatment. In all cases, the discharge information should include advice on sun protection and healthful sun exposure practices (an information-oriented CSP). 3.4 If referral is indicated, write a full report for the dermatology CMU to ensure the transfer of information between professionals in the 2 care settings as well as to ensure continuity of care (a CSP). 3.5 Most benign cysts and tumors will be given a clinical diagnosis. If a firm clinical diagnosis is not possible or a malignant tumor is suspected, the patient must be referred to the dermatology CMU. The referral should be arranged during the same visit. A system for priority referrals to the specialist must be established based on signs and symptoms for optimal efficiency and use of health care resources (an information-oriented CSP). 3.6 Primary care centers and dermatology CMUs with teledermatology capability will use this means of consultation between professionals. Consultation by teledermatology on any lesion destined for minor outpatient surgical treatment in primary care is encouraged. In the absence of teledermatology capability, the patient should enter the clinical pathway for skin cancer whenever malignancy is suspected. |
| 4. Surgical treatment Lesions to be treated in primary care center units for minor outpatient surgery (Table 3) |
| 4.1 Unequivocally identify the patient in the surgical area according to established procedures (a CSP). 4.2 Wash hands before and after the examination, according to established procedures (a CSP). 4.3 Unequivocally identify the lesion to be excised according to the center's established procedures (a CSP). 4.4 Check all items on the center's surgical safety checklist (a CSP). 4.5 Benign cysts or tumors that interfere with the patient's normal activities because of mechanical or functional problems due to location, size, or symptoms will be treated in the primary care center's outpatient surgical unit. The purpose is therapeutic. 4.6 Unequivocally label the containers that will be used to transfer the excised material to the pathology CMU (a CSP). Each container will hold a single lesion. The number of containers sent to the pathology unit will match the number of lesions excised (a CSP). 4.7 The surgeon will complete a surgical report describing the diagnosis, location, anesthetic and surgical techniques used; suture material used; number of lesions excised; and the number of properly labeled containers sent to pathology. 4.8 The patient will receive a continuity-of-care report describing postsurgical care, where such care will take place (primary care center, hospital), warning signs of complications, and how to obtain care in case a complication develops (an information-oriented CSP). 4.9 The patient will be given an appointment for a follow-up visit at which the results of the procedure will be disclosed (an information-oriented CSP). |
Abbreviations: CMU, clinical management unit; CSP, critical safety point affecting patients as listed by the health service of the government of Andalusia (the Junta).
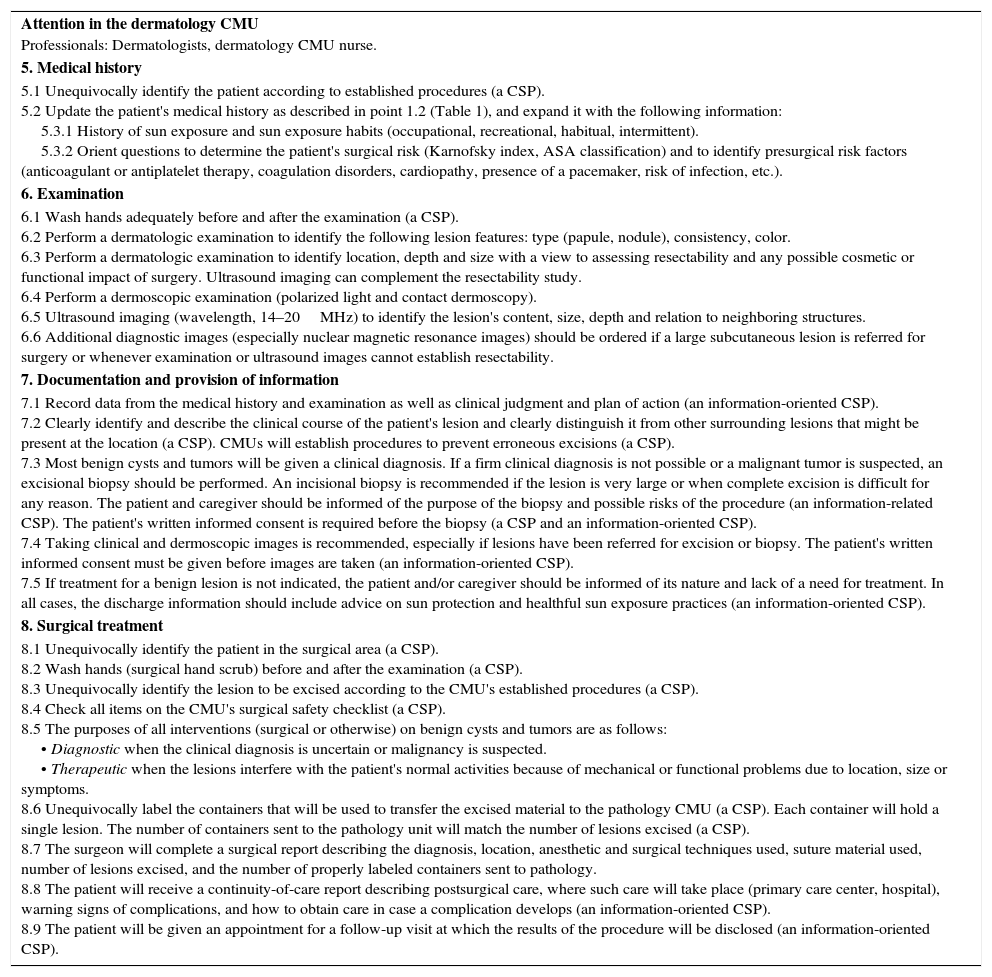
Quality-of-Care Characteristics to Apply When Attending Persons With Benign Cysts or Tumors in Dermatology CMUs.
| Attention in the dermatology CMU Professionals: Dermatologists, dermatology CMU nurse. |
| 5. Medical history |
| 5.1 Unequivocally identify the patient according to established procedures (a CSP). 5.2 Update the patient's medical history as described in point 1.2 (Table 1), and expand it with the following information: 5.3.1 History of sun exposure and sun exposure habits (occupational, recreational, habitual, intermittent). 5.3.2 Orient questions to determine the patient's surgical risk (Karnofsky index, ASA classification) and to identify presurgical risk factors (anticoagulant or antiplatelet therapy, coagulation disorders, cardiopathy, presence of a pacemaker, risk of infection, etc.). |
| 6. Examination |
| 6.1 Wash hands adequately before and after the examination (a CSP). 6.2 Perform a dermatologic examination to identify the following lesion features: type (papule, nodule), consistency, color. 6.3 Perform a dermatologic examination to identify location, depth and size with a view to assessing resectability and any possible cosmetic or functional impact of surgery. Ultrasound imaging can complement the resectability study. 6.4 Perform a dermoscopic examination (polarized light and contact dermoscopy). 6.5 Ultrasound imaging (wavelength, 14–20MHz) to identify the lesion's content, size, depth and relation to neighboring structures. 6.6 Additional diagnostic images (especially nuclear magnetic resonance images) should be ordered if a large subcutaneous lesion is referred for surgery or whenever examination or ultrasound images cannot establish resectability. |
| 7. Documentation and provision of information |
| 7.1 Record data from the medical history and examination as well as clinical judgment and plan of action (an information-oriented CSP). 7.2 Clearly identify and describe the clinical course of the patient's lesion and clearly distinguish it from other surrounding lesions that might be present at the location (a CSP). CMUs will establish procedures to prevent erroneous excisions (a CSP). 7.3 Most benign cysts and tumors will be given a clinical diagnosis. If a firm clinical diagnosis is not possible or a malignant tumor is suspected, an excisional biopsy should be performed. An incisional biopsy is recommended if the lesion is very large or when complete excision is difficult for any reason. The patient and caregiver should be informed of the purpose of the biopsy and possible risks of the procedure (an information-related CSP). The patient's written informed consent is required before the biopsy (a CSP and an information-oriented CSP). 7.4 Taking clinical and dermoscopic images is recommended, especially if lesions have been referred for excision or biopsy. The patient's written informed consent must be given before images are taken (an information-oriented CSP). 7.5 If treatment for a benign lesion is not indicated, the patient and/or caregiver should be informed of its nature and lack of a need for treatment. In all cases, the discharge information should include advice on sun protection and healthful sun exposure practices (an information-oriented CSP). |
| 8. Surgical treatment |
| 8.1 Unequivocally identify the patient in the surgical area (a CSP). 8.2 Wash hands (surgical hand scrub) before and after the examination (a CSP). 8.3 Unequivocally identify the lesion to be excised according to the CMU's established procedures (a CSP). 8.4 Check all items on the CMU's surgical safety checklist (a CSP). 8.5 The purposes of all interventions (surgical or otherwise) on benign cysts and tumors are as follows: • Diagnostic when the clinical diagnosis is uncertain or malignancy is suspected. • Therapeutic when the lesions interfere with the patient's normal activities because of mechanical or functional problems due to location, size or symptoms. 8.6 Unequivocally label the containers that will be used to transfer the excised material to the pathology CMU (a CSP). Each container will hold a single lesion. The number of containers sent to the pathology unit will match the number of lesions excised (a CSP). 8.7 The surgeon will complete a surgical report describing the diagnosis, location, anesthetic and surgical techniques used, suture material used, number of lesions excised, and the number of properly labeled containers sent to pathology. 8.8 The patient will receive a continuity-of-care report describing postsurgical care, where such care will take place (primary care center, hospital), warning signs of complications, and how to obtain care in case a complication develops (an information-oriented CSP). 8.9 The patient will be given an appointment for a follow-up visit at which the results of the procedure will be disclosed (an information-oriented CSP). |
Abbreviation: CMU, clinical management unit; ASA, American Society of Anesthesiologists; CSP, critical safety point affecting patients as listed by the health service of the government of Andalusia (the Junta).
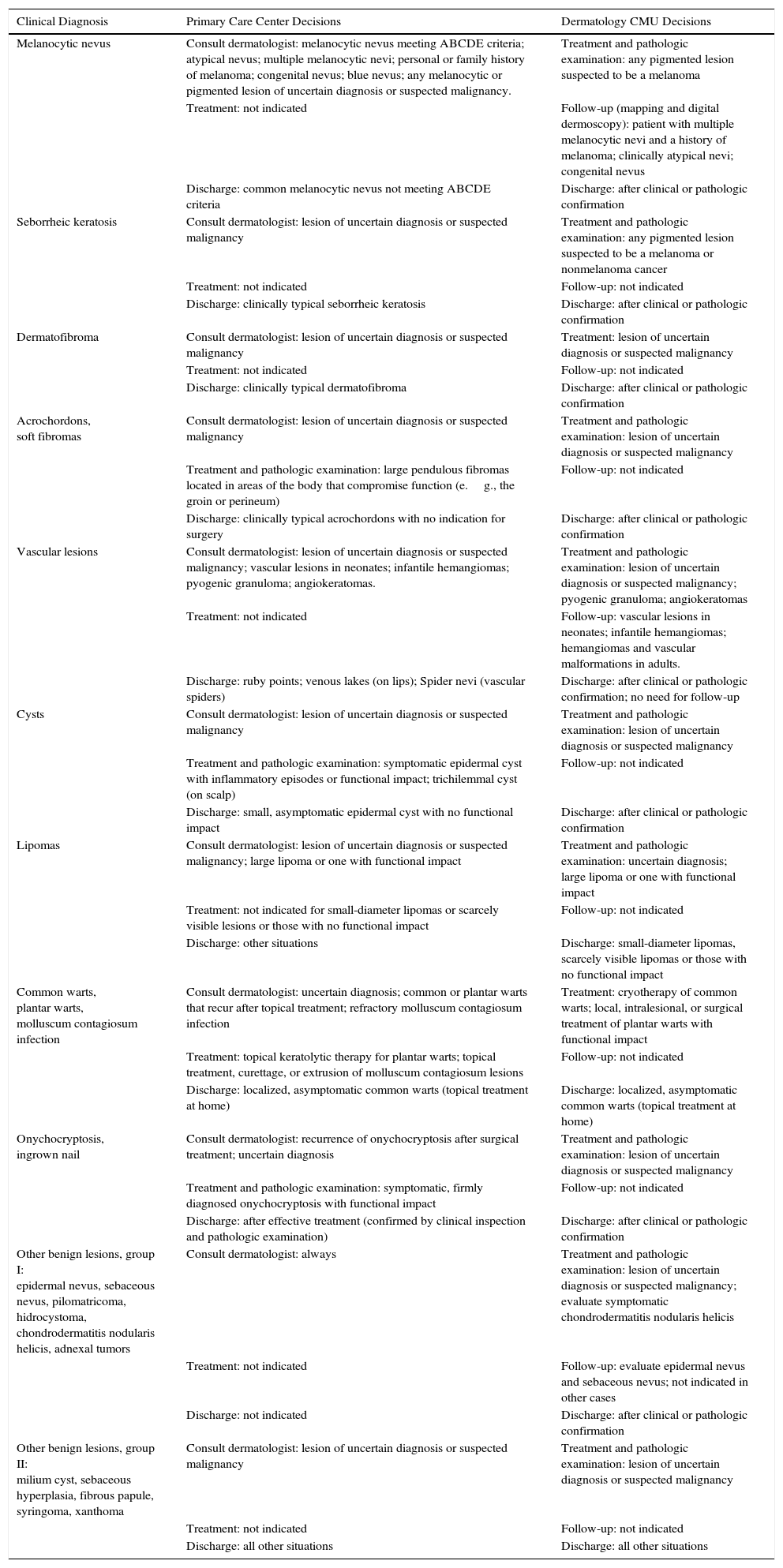
Table 3 describes decision-making recommendations to apply when a person consults a physician regarding a benign cyst or tumor in each of the care settings in the NHS. The recommendations can be summarized as follows:
- •
Refer to a dermatologist any patient who has a lesion that has not been firmly diagnosed.
- •
Offer surgical treatment for any lesion the dermatologist cannot diagnose firmly in order to rule out the possibility of malignancy.
- •
Refer the case to the CMU for pathology for diagnostic confirmation whenever a lesion has been managed surgically (for diagnosis or with intention to treat) in any setting (primary care or a dermatology CMU).
Recommended Decisions for Use When Attending Patients With Benign Cysts or Tumors in Primary Care Centers and Dermatology CMUs.
| Clinical Diagnosis | Primary Care Center Decisions | Dermatology CMU Decisions |
|---|---|---|
| Melanocytic nevus | Consult dermatologist: melanocytic nevus meeting ABCDE criteria; atypical nevus; multiple melanocytic nevi; personal or family history of melanoma; congenital nevus; blue nevus; any melanocytic or pigmented lesion of uncertain diagnosis or suspected malignancy. | Treatment and pathologic examination: any pigmented lesion suspected to be a melanoma |
| Treatment: not indicated | Follow-up (mapping and digital dermoscopy): patient with multiple melanocytic nevi and a history of melanoma; clinically atypical nevi; congenital nevus | |
| Discharge: common melanocytic nevus not meeting ABCDE criteria | Discharge: after clinical or pathologic confirmation | |
| Seborrheic keratosis | Consult dermatologist: lesion of uncertain diagnosis or suspected malignancy | Treatment and pathologic examination: any pigmented lesion suspected to be a melanoma or nonmelanoma cancer |
| Treatment: not indicated | Follow-up: not indicated | |
| Discharge: clinically typical seborrheic keratosis | Discharge: after clinical or pathologic confirmation | |
| Dermatofibroma | Consult dermatologist: lesion of uncertain diagnosis or suspected malignancy | Treatment: lesion of uncertain diagnosis or suspected malignancy |
| Treatment: not indicated | Follow-up: not indicated | |
| Discharge: clinically typical dermatofibroma | Discharge: after clinical or pathologic confirmation | |
| Acrochordons, soft fibromas | Consult dermatologist: lesion of uncertain diagnosis or suspected malignancy | Treatment and pathologic examination: lesion of uncertain diagnosis or suspected malignancy |
| Treatment and pathologic examination: large pendulous fibromas located in areas of the body that compromise function (e.g., the groin or perineum) | Follow-up: not indicated | |
| Discharge: clinically typical acrochordons with no indication for surgery | Discharge: after clinical or pathologic confirmation | |
| Vascular lesions | Consult dermatologist: lesion of uncertain diagnosis or suspected malignancy; vascular lesions in neonates; infantile hemangiomas; pyogenic granuloma; angiokeratomas. | Treatment and pathologic examination: lesion of uncertain diagnosis or suspected malignancy; pyogenic granuloma; angiokeratomas |
| Treatment: not indicated | Follow-up: vascular lesions in neonates; infantile hemangiomas; hemangiomas and vascular malformations in adults. | |
| Discharge: ruby points; venous lakes (on lips); Spider nevi (vascular spiders) | Discharge: after clinical or pathologic confirmation; no need for follow-up | |
| Cysts | Consult dermatologist: lesion of uncertain diagnosis or suspected malignancy | Treatment and pathologic examination: lesion of uncertain diagnosis or suspected malignancy |
| Treatment and pathologic examination: symptomatic epidermal cyst with inflammatory episodes or functional impact; trichilemmal cyst (on scalp) | Follow-up: not indicated | |
| Discharge: small, asymptomatic epidermal cyst with no functional impact | Discharge: after clinical or pathologic confirmation | |
| Lipomas | Consult dermatologist: lesion of uncertain diagnosis or suspected malignancy; large lipoma or one with functional impact | Treatment and pathologic examination: uncertain diagnosis; large lipoma or one with functional impact |
| Treatment: not indicated for small-diameter lipomas or scarcely visible lesions or those with no functional impact | Follow-up: not indicated | |
| Discharge: other situations | Discharge: small-diameter lipomas, scarcely visible lipomas or those with no functional impact | |
| Common warts, plantar warts, molluscum contagiosum infection | Consult dermatologist: uncertain diagnosis; common or plantar warts that recur after topical treatment; refractory molluscum contagiosum infection | Treatment: cryotherapy of common warts; local, intralesional, or surgical treatment of plantar warts with functional impact |
| Treatment: topical keratolytic therapy for plantar warts; topical treatment, curettage, or extrusion of molluscum contagiosum lesions | Follow-up: not indicated | |
| Discharge: localized, asymptomatic common warts (topical treatment at home) | Discharge: localized, asymptomatic common warts (topical treatment at home) | |
| Onychocryptosis, ingrown nail | Consult dermatologist: recurrence of onychocryptosis after surgical treatment; uncertain diagnosis | Treatment and pathologic examination: lesion of uncertain diagnosis or suspected malignancy |
| Treatment and pathologic examination: symptomatic, firmly diagnosed onychocryptosis with functional impact | Follow-up: not indicated | |
| Discharge: after effective treatment (confirmed by clinical inspection and pathologic examination) | Discharge: after clinical or pathologic confirmation | |
| Other benign lesions, group I: epidermal nevus, sebaceous nevus, pilomatricoma, hidrocystoma, chondrodermatitis nodularis helicis, adnexal tumors | Consult dermatologist: always | Treatment and pathologic examination: lesion of uncertain diagnosis or suspected malignancy; evaluate symptomatic chondrodermatitis nodularis helicis |
| Treatment: not indicated | Follow-up: evaluate epidermal nevus and sebaceous nevus; not indicated in other cases | |
| Discharge: not indicated | Discharge: after clinical or pathologic confirmation | |
| Other benign lesions, group II: milium cyst, sebaceous hyperplasia, fibrous papule, syringoma, xanthoma | Consult dermatologist: lesion of uncertain diagnosis or suspected malignancy | Treatment and pathologic examination: lesion of uncertain diagnosis or suspected malignancy |
| Treatment: not indicated | Follow-up: not indicated | |
| Discharge: all other situations | Discharge: all other situations |
Abbreviations: ABCDE, asymmetry, border, color, diameter, evolving; CMU, clinical management unit.
This paper was drafted to reflect the consensus reached by dermatologists with clinical and management knowledge and experience who participated in a working group organized according to the Metaplan approach. This method forms groups to discuss available evidence or proposals introduced by a moderator, who poses questions and encourages participants to express opinions. The final consensus is reached by selecting ideas that have been repeated most often during the group's discussions. The participating dermatologists came from all the provinces and health centers in the autonomous community of Andalusia. Support in applying the method was given by professionals from the Spanish Society for Quality in Health Care (SECA).
Because of the lack of literature on the group's topic of focus, recommendations were drafted based on the framework of the Andalusian NHS; the purpose was to facilitate the system's ability to resolve many incidents involving care for the large group of patients with benign cysts and tumors.
The lack of available evidence supporting treatment of these lesions, a protocol for referring patients to specialists, or any other relevant criteria obliged us to base our recommendations on consensus among professionals with appropriate clinical and management experience. This situation is the main limitation affecting the recommendations (evidence level IV).
ConclusionsOver the last 10 years, the discussion of how to organize care for patients with benign cysts and tumors has focused on defining the settings (primary care or dermatology CMUs) where these lesions should be managed. However, the NHS must currently give priority to doing procedures that have a clear impact on health. The tendency is to recommend that the system set aside interventions unrelated to health. This new paradigm obliges us to redirect the priorities of dermatology CMUs toward integrated care processes that affect patients’ health without neglecting the use of all means necessary to correctly diagnose any type of lesion the patient seeks care for.
We acknowledge the help of Professor Rosa Ortega, president of the Andalusian Regional Section of the AEDV.
Please cite this article as: Moreno-Ramírez D, Ruiz-Villaverde R, de Troya M, Reyes-Alcázar V, Alcalde M, Galán M, et al. Proceso de atención a las personas con lesiones quísticas y tumorales benignas. Documento de consenso de la sección territorial andaluza de la Academia Española de Dermatología Médico-Quirúrgica y Venereología. Actas Dermosifiliogr. 2016;107:391–399.