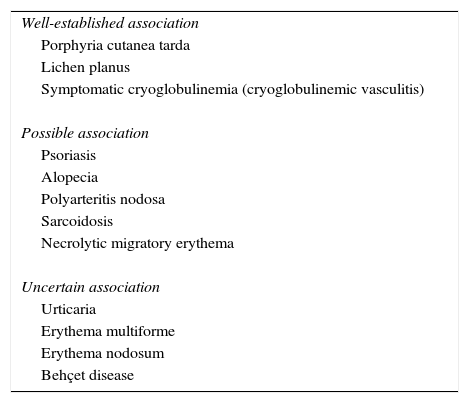
The hepatitis C virus (HCV) is one of the most common causes of chronic liver disease worldwide. The virus increases the risk of liver cirrhosis and hepatocellular carcinoma. HCV is associated with numerous extrahepatic manifestations, such as type 2 diabetes mellitus, chronic kidney disease, cardiovascular disease, non-Hodgkin lymphomas, and various skin diseases (Table 1). Patients infected with HCV may have symptomatic mixed cryoglobulinemia (cryoglobulinemic vasculitis), which has an estimated prevalence of 4.9%, as well as porphyria cutanea tarda and lichen planus, with a relative risk 2 and 8 times that of the general population, respectively.1 Other skin disorders possibly associated with HCV are psoriasis, alopecia, pruritus, polyarteritis nodosa, sarcoidosis, and necrolytic migratory erythema. Urticaria, Behçet disease, erythema nodosum, and erythema multiforme have also been reported, although the association is less clear.
Skin Disorders Associated With Hepatitis C Virus Infection.
| Well-established association |
| Porphyria cutanea tarda |
| Lichen planus |
| Symptomatic cryoglobulinemia (cryoglobulinemic vasculitis) |
| Possible association |
| Psoriasis |
| Alopecia |
| Polyarteritis nodosa |
| Sarcoidosis |
| Necrolytic migratory erythema |
| Uncertain association |
| Urticaria |
| Erythema multiforme |
| Erythema nodosum |
| Behçet disease |
Source: Younossi et al.1
The recent introduction of the latest generation of direct acting antivirals (DAAs)—including sofosbuvir, ledipasvir, daclatasvir, asunaprevir, and others—has revolutionized the treatment of chronic HCV infection due to the very high effectiveness, excellent safety profile, and tolerability of these drugs.2 Current clinical guidelines (September 2016) suggest initiating treatment in all patients with chronic HCV infection except those with limited life expectancy.3
Recently there have been reports of improvement in skin diseases associated with HCV after successful treatment with DAAs. A prospective study in Spain of 64 patients with mixed cryoglobulinemia secondary to HCV infection, 35 of whom had manifestations of cryoglobulinemic vasculitis—including purpura (65%, 23 of 35 patients), joint or muscle pain (51%), and neurologic or renal involvement (70%)—found that complete clinical response was achieved in 71% of symptomatic patients after therapy with various combinations of DAAs. In the patients who had purpura, cutaneous involvement remitted after sustained virological response (SVR) in nearly all cases (21 of 23 patients).2 Nagao et al.4 presented a series of 7 patients with HCV and oral lichen planus—4 with erosive lichen planus (3 of whom were previously treated with topical corticosteroids)—who received daclatasvir-asunaprevir combination therapy with SVR; complete resolution of oral disease was achieved in 4 patients and partial improvement was achieved in 3. Finally, Tong et al.5 described 3 individuals diagnosed with porphyria cutanea tarda and HCV infection who were successfully treated with ledipasvir-sofosbuvir combination therapy. Remission of cutaneous symptoms was achieved in 2 patients, and a marked decrease in the number of erosive lesions was achieved in the third patient between 1 and 3 months after completion of antiviral therapy.
In conclusion, DAAs are highly effective and safe for the treatment of HCV infection. Some reports suggest that DAAs could also achieve improvement in some skin diseases associated with HCV and that these drugs could perhaps be a therapeutic option for patients with aggressive skin disorders or who do not respond to conventional treatments. Given that the use of these drugs is expected to increase, we will be able to see whether these effects occur in a larger number of patients and if the effects persist over time.
Please cite this article as: Morgado-Carrasco D, Fustà-Novell X, Podlipnik S, Giavedoni P. FR-¿Son los nuevos agentes antivirales de acción directa un tratamiento eficaz para las manifestaciones cutáneas de la hepatitis C?. Actas Dermosifiliogr. 2017;108:365–366.