Amyloidosis describes a group of diseases characterized by deposition of a substance with an amorphous appearance that is stained by Congo red in various tissues and organs. The diseases can be differentiated from one another by the type of precursor protein for the amyloid substance. Primary amyloidosis is the most common form, with an annual incidence of 0.9 new cases per 100 000 inhabitants. Secondary forms include those resulting from hematologic disorders, renal disease, and autoimmune diseases.
There are more than 30 unrelated autologous proteins that can cause amyloidosis. Identifying the amyloid protein is crucial for correct diagnosis and, above all, appropriate treatment, which can range from autologous stem cell transplantation to liver transplantation.1
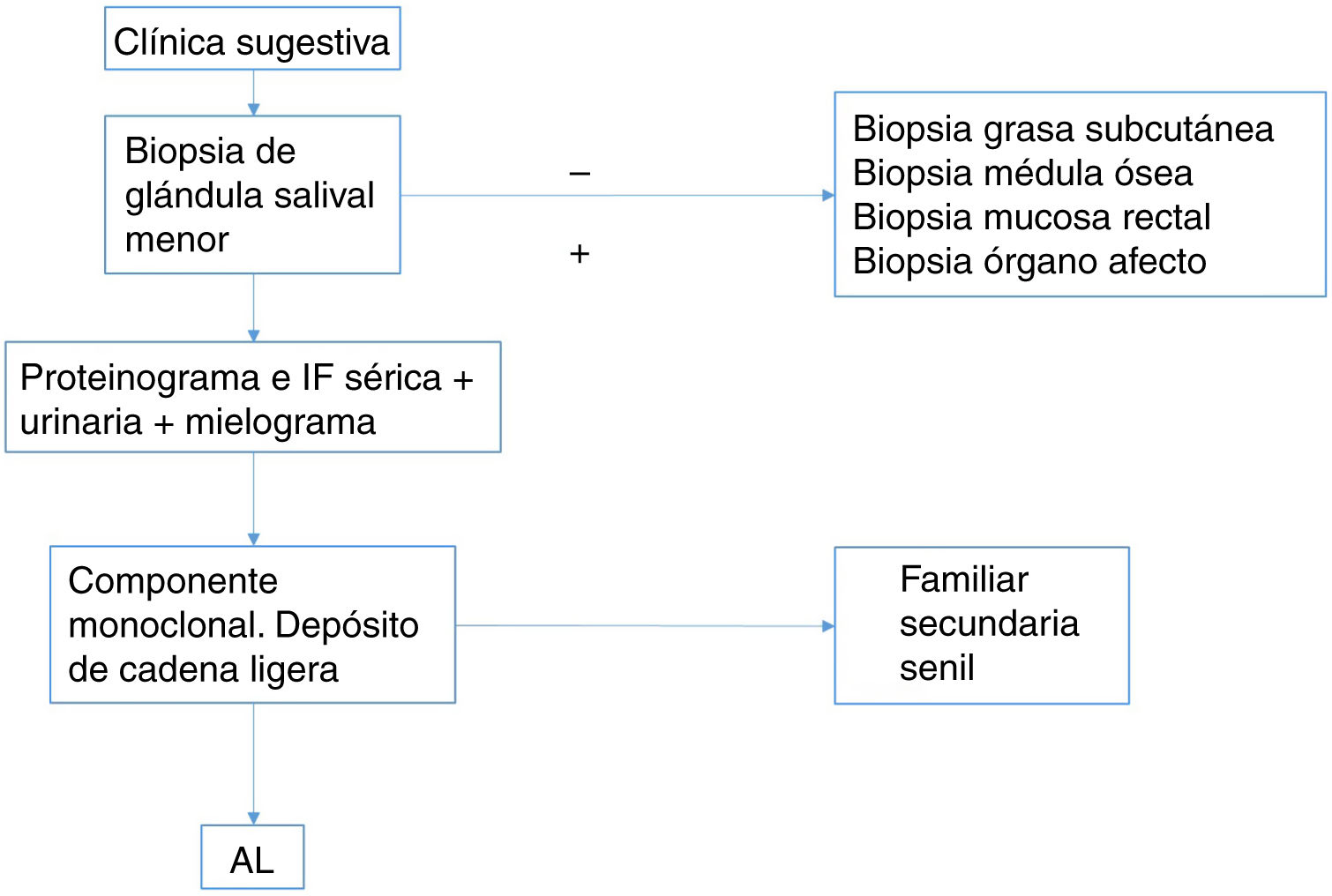
The initial step for diagnosis, as mentioned above, is detecting the presence of amyloid in a sample from the affected organ through Congo red staining, followed by a second step of exact typing of the implicated protein. It is not always possible to carry out a biopsy of the target organ given the potential risk of postoperative bleeding, infection, pain, and technical issues arising from difficulties with surgical access, and so it is necessary to resort to more accessible tissues.
Traditionally, rectal biopsy was the preferred method for screening, although biopsy of subcutaneous fat started to predominate from 1973 onwards. In most hospitals, biopsies were the responsibility of dermatologists. The sensitivity of rectal biopsy varies between 54% and 82%, depending on the series.2
In our experience, we found a positivity rate of just 1% in consecutive biopsy sampling of subcutaneous fat performed after consultation with the nephrology department (28/100) and autoimmune disease unit (72/100) in the context of different autoimmune diseases. This prompted us to systematically review the biopsy technique and sample processing, and we opted to combine 2 simultaneous biopsies, one of subcutaneous fat and the other of the minor salivary gland. We now found a positivity rate of 2% and 45%, respectively, in consecutive biopsy samples for amyloidosis screening in 50 patients from the nephrology department and autoimmune disease unit. All cases positive for biopsy of the salivary gland were positive in subcutaneous fat but not vice versa.
Biopsy of the minor salivary glands is therefore slowly becoming the most widespread method, with easy access and few associated complications for detection of amyloidosis. The presence of abundant parenchyma and secretory components along with a rich blood supply make it the site of choice for taking samples.3
Its sensitivity is close to that estimated for abdominal fat with percentages between 83% and 100%.4 It requires a minimal incision with very little risk of bleeding or nerve damage. It can be performed in an outpatient setting and without any apparent scarring, unlike abdominal fat biopsy.
For this reason, we propose the following diagnostic algorithm for screening for amyloidosis while awaiting more robust studies that compare the different techniques. Our conclusion is that the technique of choice should be salivary gland biopsy, and in cases with a high suspicion but with a negative result, abdominal fat biopsy or biopsy of the affected organ could be considered (Fig. 1).
Please cite this article as: Ródenas-Herranz T, Linares-Gonzalez L, Ruiz-Villaverde R. FR - Diagnóstico de amiloidosis: ¿biopsia de grasa subcutánea o de glándula salivar menor? Actas Dermosifiliogr. 2020;111:520–521.