TNFα inhibitors revolutionized the treatment of immune-mediated inflammatory diseases (IMIDs). Due to their immunosuppressive nature, these therapies increase susceptibility for new infections and may alter the natural course of latent infections.1,2
Occult HBV infection is defined as the persistence of viral genome in the liver tissue of individuals serologically negative for HBV surface antigen (HBsAg).3 Patients with positive antibodies to HBV core antigen (anti-HBc) and negative HBsAg and HBV-DNA, with or without antibodies to HBV surface antigen (anti-HBs) are potential occult HBV carriers3 and may reactivate under immunosuppressive therapy.1,2 Studies in subjects with past HBV infection treated with anti-TNFα therapy for inflammatory bowel disease (IBD) and rheumatic diseases estimated a reactivation rate between 1.7% and 5% of patients.1,2
The aim of this retrospective study was to evaluate the rate of reactivation in anti-HBc positive/HBsAg negative patients treated with TNFα inhibitors for psoriasis, rheumatologic diseases and IBD.
Patients treated with TNFα inhibitors for IMIDs from January 2000 to December 2014, for at least one month were retrospectively included. Information regarding patients’ HBV screening serology (HBsAg, anti-HBc and anti-HBs antibodies) and HBV-DNA (in anti-HBc positive patients) prior to the initiation of TNFα inhibitors as well as HBsAg seroconversion, HBV-DNA de novo detection and ALT/AST levels during anti-TNF therapy were collected. HBV reactivation was defined as titer elevation up to 2–3 times the upper limit of normal ALT, in combination with de novo detection of HBV-DNA or HBsAg seroconversion. Furthermore, patients’ demographic, clinical and therapeutic characteristics were recorded. This study was approved by the hospital's Institutional Review Board.
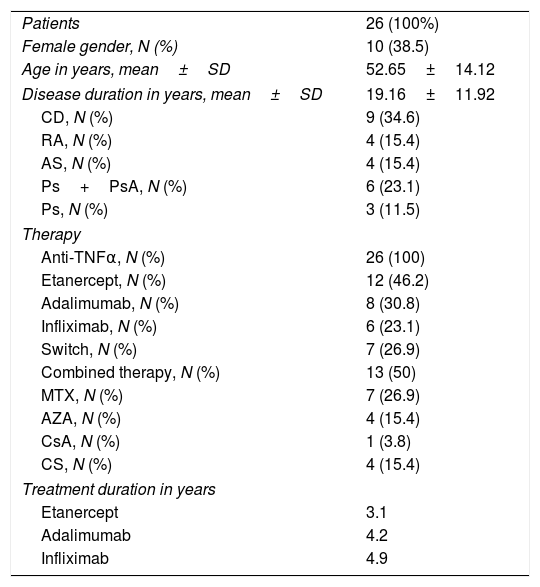
From 389 patients treated with TNFα inhibitors during the study period, 26 (9%) patients were anti-HBc positive/HBsAg negative and one patient presented with a serologic profile compatible with chronic hepatitis B. The mean observation time was 43.6±28.7 months. Subjects’ demographic and clinical data are reported in Table 1. Nineteen (73.1%) patients were anti-HBs positive in the pre-treatment screening. HBV-DNA levels were available in 7 (26.9%) patients, being undetectable in all of them. Additionally, during follow-up, HBV-DNA levels were measured in 7 additional patients (that had not been measured before treatment) amounting to 53.8% patients with undetectable HBV-DNA levels. In these patients, HBV-DNA levels were measured every 6months for a 2-years period. No rise of the aminotransferases values was observed in any patient during follow-up. At the end of the observational period, no case of reactivation was observed regardless of anti-HBs positivity.
Baseline characteristics of 26 anti-HBc positive/HBsAg negative patients.
| Patients | 26 (100%) |
| Female gender, N (%) | 10 (38.5) |
| Age in years, mean±SD | 52.65±14.12 |
| Disease duration in years, mean±SD | 19.16±11.92 |
| CD, N (%) | 9 (34.6) |
| RA, N (%) | 4 (15.4) |
| AS, N (%) | 4 (15.4) |
| Ps+PsA, N (%) | 6 (23.1) |
| Ps, N (%) | 3 (11.5) |
| Therapy | |
| Anti-TNFα, N (%) | 26 (100) |
| Etanercept, N (%) | 12 (46.2) |
| Adalimumab, N (%) | 8 (30.8) |
| Infliximab, N (%) | 6 (23.1) |
| Switch, N (%) | 7 (26.9) |
| Combined therapy, N (%) | 13 (50) |
| MTX, N (%) | 7 (26.9) |
| AZA, N (%) | 4 (15.4) |
| CsA, N (%) | 1 (3.8) |
| CS, N (%) | 4 (15.4) |
| Treatment duration in years | |
| Etanercept | 3.1 |
| Adalimumab | 4.2 |
| Infliximab | 4.9 |
CD, Chron's disease; RA, rheumatoid arthritis; AS, ankylosing spondylitis; Ps, psoriasis; PsA, psoriatic arthritis; TNF, tumor necrosis factor; MTX, methotrexate; AZA, azathioprine; CsA, cyclosporine A; CS, corticosteroids.
Patients with past HBV infection (anti-HBc positive/HBsAg negative patients) can arbor an occult infection, and be susceptible to reactivation when exposed to immunosuppression, including TNFα inhibitors. This risk is highly depends on the agent's target and mechanism of action.4,5 Although it is accepted that TNFα inhibitors may lead to HBV reactivation in these patients, the reactivation rates are much lower when compared to HBsAg positive patients.1 The prevalence of patients with past HBV (9%) found in this study was similar to other published studies in patients with IMIDs.6 A systematic review including 168 anti-HBc positive/HBsAg negative patients with RA, spondyloarthropathies, psoriasis and IBD found HBV reactivation 5.4% of patients1 while a meta-analysis including 468 anti-HBc positive/HBsAg negative patients treated with TNFα inhibitors for rheumatologic diseases, HBV reactivation was observed in 1.7% with a percentage of HBV reactivation ranging from 0 to 8.3%.2 As seen in other studies, including with patients with psoriasis, no cases of HBV reactivation were observed in this study.7,8
All patients that had HBV DNA measured during screening, maintained their levels below detection threshold during follow-up (measured every 6 months for 2 years and then yearly). However, detectable baseline viral loads have been found in this subset of patients.9
The title of anti-HBs may influence the risk of reactivation of HBV.9 In this study, 73.1% patients were anti-HBs positive in the pre-treatment screening, and may have been important decreasing the risk of HBV reactivation.
The main limitation of this study is its retrospective nature and the small and heterogenic sample, the long period of inclusion (as intra-hospital and international recommendations has changed along time) and the inexistence of HBV DNA data for some of the anti-HBc positive/HBsAg negative patients (preventing to determine HBV occult infection).
Current guidelines state that candidates for chemotherapy and immunosuppressive therapy who are anti-HBc positive/HBsAg negative, regardless of anti-HBs status and with undetectable serum HBV-DNA should be followed carefully by means of ALT and HBV-DNA testing and treated with nucleotide analogs therapy only upon confirmation of HBV reactivation before ALT elevation.10
Treatment with anti-TNFα agents is safe in anti-HBc positive/HBsAg negative patients. HBV reactivation is probably related to the presence of HBV in circulation rather than to the serologic status of previous exposure. Nonetheless, and as expressed in current guidelines, screening for HBV serologic markers prior to initiation of anti-TNFα therapy is of major importance since it may dictate if prophylactic treatment, vaccination or monitoring should be taken to minimize the risks related to hepatitis B flare/reactivation.
Conflict of interestsRui Pereira, Inês Lobo and Filipe Nery have no conflicts of interest to disclosure.
Tiago Torres has participated in clinical trials sponsored by AbbVie, Amgen, and Novartis and has received honoraria for acting as a consultant and/or as a speaker at events sponsored by AbbVie, Boehringer Ingelheim, Celgene, Janssen, Leo-Pharma, Eli-Lilly, MSD, Novartis, and Pfizer.
The authors thank Raquel Faria, MD and Paula Lago, MD the important collaboration in this study.