Medical errors are an important cause of mortality, even greater than traffic accidents or breast cancer. Surgical fires are rare, but they can lead to significant morbidity and mortality in patients. Although it is estimated that between 200 and 240 surgical fires occur out of the 65million surgical procedures performed each year in the United States, the actual incidence remains unknown.1 Below are the main characteristics of surgical fires and how to prevent them.
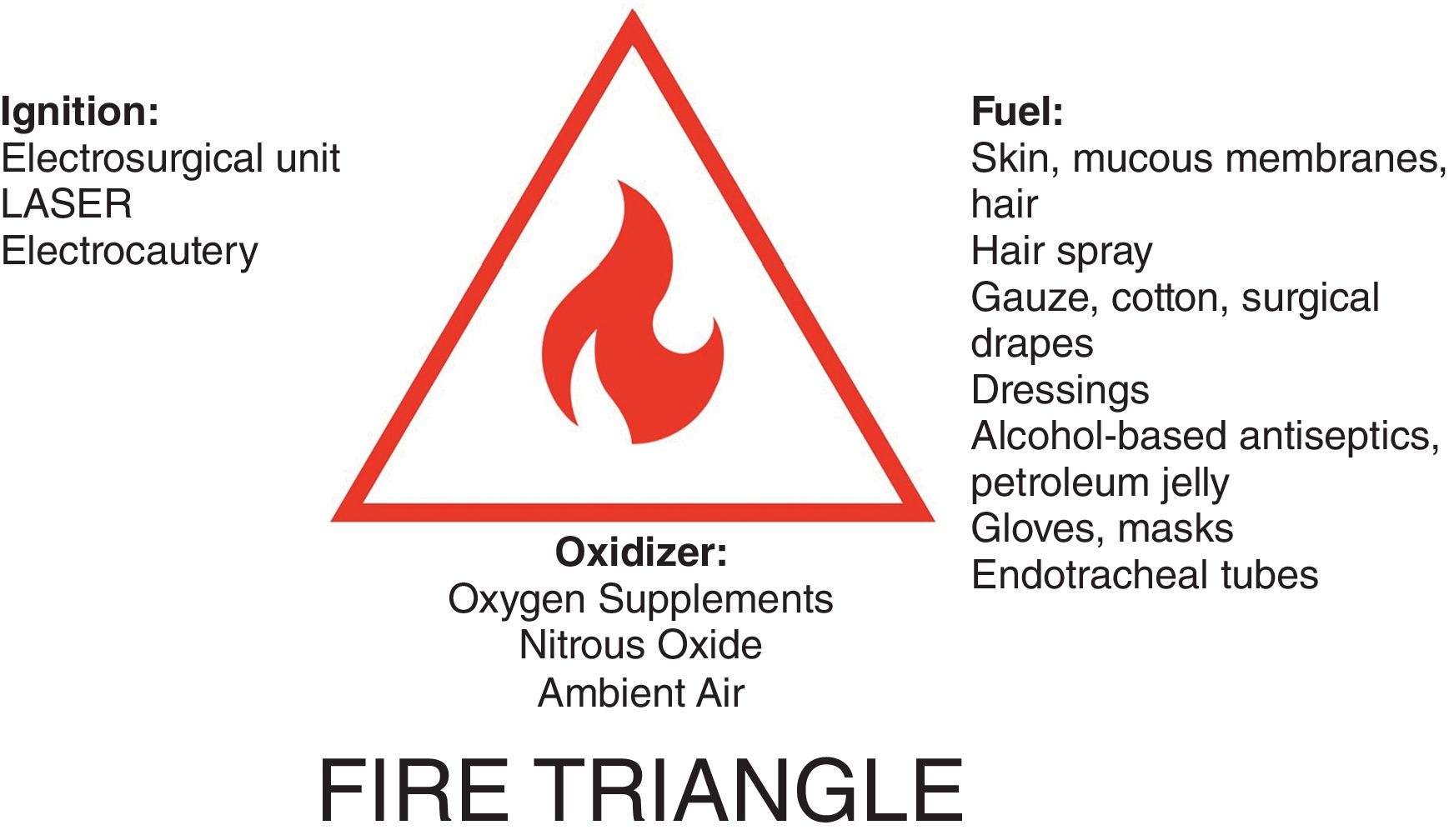
Causes of surgical fires. Fires occur at the intersection of 3 components that form the “fire triangle”2: (a) fuel (skin, mucosa, hair, alcohol, gauze, dressings, petroleum jelly, etc.), (b) oxidizer (ambient air, supplemental oxygen, and nitrous oxide), and (c) ignition source (electrosurgical units, portable battery-powered thermal electrocautery machine, and lasers) (Fig. 1).
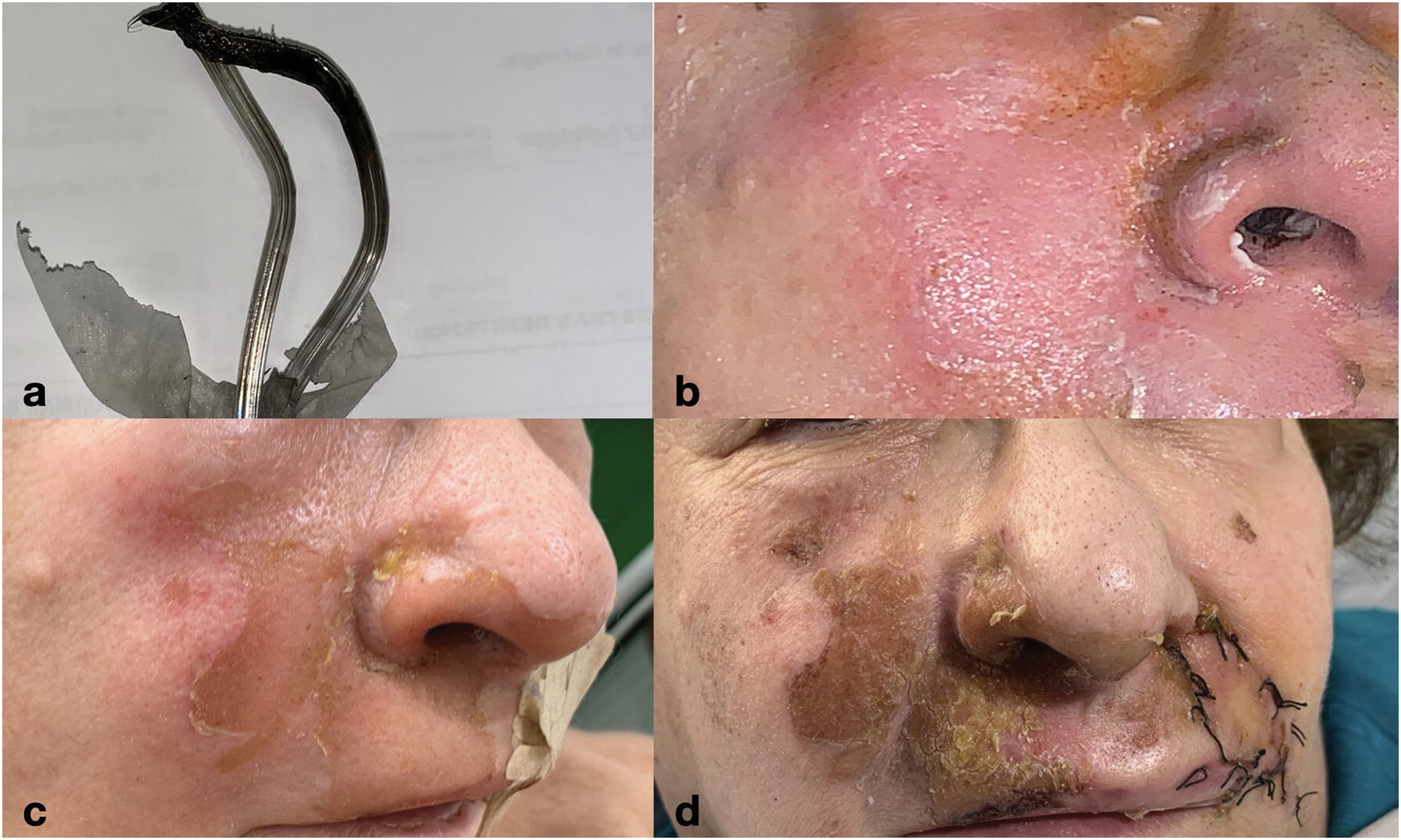
Ignition of gases is one of the main causes of deflagration.3 This occurs when the PaO2 is >22%. A closed surgical field, with a “tent effect,” can increase concentration up to 53.5% at 6L/min, with higher levels the closer it gets to the source. For this reason, it is recommended to place the source>10cm away. As examples to consider, a CO2 laser at 30W can ignite at 2L/min with the source<5cm away, and electrocautery at 20W ignites at 1cm from the nasal cannula (Fig. 2).
Regarding antiseptics, most are alcohol-based.4,5 Chlorhexidine in 70% alcohol ignites at 900°C. In a 100% oxygen environment, it ignites at 30°C. The electrosurgical unit can ignite solutions with a 20% alcohol concentration. Additionally, the vapor produced by alcohol evaporation on contact with body heat can facilitate combustion. Therefore, it is important to dry the surgical field after antisepsis.6
Preventive measures for surgical fires. In the case of laser or electrocautery use, the following preventive measures should be taken7,8:
- –
All gauze, cotton, or clothing should be removed or continuously moistened throughout the procedure.
- –
Hair adjacent to laser fields should be shaved or continuously moistened with saline solution or water.
- –
Transparent/colorless masks, nasal cannulas, and other respiratory devices should be used.
- –
The patient's skin should not be cleaned with alcohol-based solutions. The patient should avoid using hair spray, colognes, or other personal care products containing alcohol before procedures.
- –
The inspired gas mixture should contain a minimum level of oxygen to maintain the patient's oxygen saturation, using gases (e.g., helium, nitrogen, compressed air) and inhaled anesthetics with the lowest flammability.
- –
Oxygen and other gases, such as nitrous oxide should never be directed toward the field.
- –
If procedures close to the respiratory tract require general anesthesia with endotracheal intubation, the endotracheal tube shafts should be made of safe metal or wrapped with aluminum tape or copper foil in a spiral. In this way, tube flexing should not expose bare areas to the laser or electrocautery. Endotracheal cuffs should be filled with saline instead of air.
- –
Laryngeal masks with spontaneous breathing are preferred over face masks due to reduced oxygen leakage. If a face mask is used, an oxygen analyzer can be used to ensure minimal leakage.
- –
Fluorocarbon cryogens are non-flammable, although ethyl chloride is.
So far, we have been reviewing preventive measures.
Actions in the event of a surgical fire. Below is a detailed response if a fire occurs in the operating room:
- –
An action plan for a fire should be pre-established and practiced by all operating personnel.
- –
Water or saline solution and a fire extinguisher should be available near the operating field. It is essential to always know the location of the nearest extinguisher.
- –
In the event of a fire, ventilation should be stopped, and gases should be disconnected, with removal of the endotracheal tube, mask, laryngeal mask from the airways, or nasal cannula.
- –
The protective goggles required for the laser make it more difficult to see the start of the fire and smoke, so they should be removed as soon as possible.
- –
Ice packs should be applied to the patient's skin after the fire has been put out to minimize thermal injury.
- –
A flexible nasal laryngoscope or bronchoscope can be used to examine the upper airways and laryngeal tissues for injury.
- –
Thorough rinsing with water and povidone–iodine soap should be used to remove carbonized debris from burned areas, and antibiotic creams should be applied to skin burns.
- –
Once the situation is under control, the corresponding intermediate authority, usually nursing supervision, should be contacted, and the safety incident should be reported, with close patient monitoring and specific review of the equipment used.
In conclusion, there are several factors in operating rooms that make them a high fire-risk environment. In addition to being oxygen-enriched, they contain flammable materials and equipment with available ignition sources. Although operating room fires are relatively rare events, the consequences are potentially severe and mostly preventable with proactive preventive measures.
Conflicts of interestNone declared.