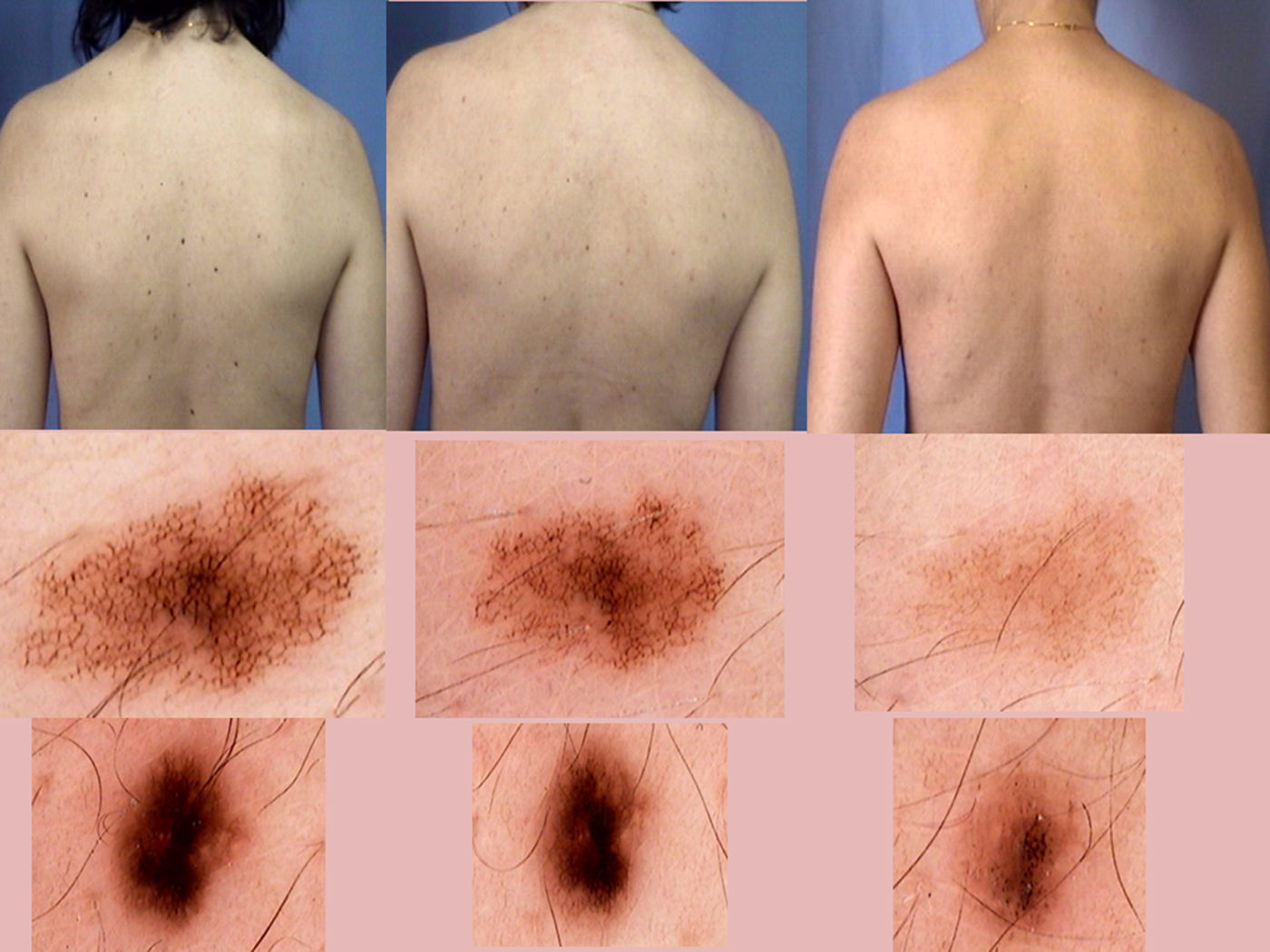
During digital follow-up of a 42-year-old woman with atypical nevi using a MoleMax II video dermoscopy system (Derma Medical, London, UK), the patient's melanocytic lesions progressively disappeared and were practically absent by the end of a 3-year period (Fig. 1). She presented with several autoimmune processes, including HLA-B27-positive sacroiliitis, ANA-positive peripheral arthritis, and autoimmune hypothyroidism that was treated with supplemental L-tyrosine. She had no personal or family history of melanoma. There was no evidence of a halo phenomenon or any other reaction around the nevi at any time. Several potential explanations can account for the disappearance of melanocytic nevi. Progressive disappearance in adulthood is a described feature of acquired melanocytic nevi (AMN).1
However, the rapid disappearance of AMN in young adults, as in the present case, is unusual. This involution can be caused by certain specific reactions. The halo or Sutton nevus can progressively fade and ultimately disappear, leaving a depigmented halo surrounding the site of the original nevus. Histologically, the condition is characterized by the presence of lymphocytic infiltrate with predominance of CD8+ T lymphocytes. This infiltrate results in progressive destruction of the melanocytes via a mechanism similar to that observed in vitiligo. This is the most common mechanism by which nevi disappear.2,3 Isolated reports have also described the disappearance of congenital melanocytic nevi, with or without a halo. In some cases histology has revealed the persistence of melanocytes despite apparent clinical disappearance.4 A completely different form of nevus disappearance involves an eccematoid reaction around the nevus (Meyerson nevus) followed by nevus involution, and is characterized by eczema-like histological findings.5 Because AMN and melanoma induce the expression of similar antigens, AMN can disappear in melanoma patients, a consequence of an immune system reaction that occurs spontaneously or is induced by immunotherapy with anti-CTL01A4 and anti-PD-1 agents.6,7 Although less common, the disappearance of nevi in patients with neither eczema nor halo nevi has been described, although few of those cases involved involution of practically all nevi, as occurred in our patient.8,9
The literature describes 3 dermoscopic patterns associated with the disappearance of melanocytic nevi: halo phenomena; blue regression (peppering), caused by the action of melanophages, and white regression, characterized by a white fibrotic area with a pseudo-cicatricial appearance; and lesion disappearance with neither halo nor regression. In the case of the third pattern, which was observed in our patient, the lesions undergo a progressive loss of pigment and the dermoscopic pattern fades until lesion disappearance.10
Given our patient's history of autoimmune diseases, the mechanism underlying nevus disappearance in this case was most likely immune in nature, although this was not histologically verified.
It is important to be familiar with the different ways in which melanocytic lesions can evolve, since clinical lesion disappearance does not always imply histological disappearance, and to remember that digital dermoscopy is a useful method by which to monitor these patients.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Álvarez-Chinchilla PJ, Poveda Montoyo I, Encabo-Durán B, Bañuls Roca J. Desaparición simultánea de nevus en un paciente con procesos autoinmunes asociados. Actas Dermosifiliogr. 2018;109:927–928.