Skin conditions are among the main reasons for seeking primary health care. Primary care physicians (PCPs) must diagnose skin conditions and determine their impact, and must therefore incorporate the relevant knowledge and skills into their education. The present study analyzes the reasons for primary care referral to dermatology (referral demand) as well as diagnostic agreement between PCPs and dermatologists informed by pathology where appropriate.
Material and methodsData were collected for 755 patients and 882 initial dermatology appointments from February 1, 2012 through April 30, 2012 following primary care referral. Data obtained included age, sex, occupation, reason for referral, primary care diagnosis, and dermatologic diagnosis. Statistical analysis of the data for each diagnosed condition identified frequency, reasons for referral, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and the κ statistic for diagnostic agreement.
ResultsThe most common diagnoses were seborrheic keratosis, melanocytic nevus, actinic keratosis, and acne. The main reason for referral was diagnostic assessment (52.5%). For skin tumors, sensitivity of primary care diagnosis was 22.4%, specificity 94.7%, PPV 40.7%, and NPV 88.3%, with a κ of 0.211. For the more common diagnoses, primary care sensitivity was generally low and specificity high.
ConclusionsAccording to our results, primary care physicians are better qualified to rule out a given skin condition in a patient (high specificity) than to establish an accurate clinical diagnosis (poor sensitivity). This suggests that knowledge and skills training should be organized for primary care physicians to improve management of skin conditions—especially skin cancer, because of its impact. A more responsive system would ensue, with shorter waiting lists and better health care.
Las enfermedades cutáneas constituyen uno de los principales motivos de consulta en atención primaria (AP), motivo por el que el médico de AP está obligado a conocer su diagnóstico y su importancia e integrar estos conocimientos y aptitudes en su formación. En este estudio realizamos un análisis de los motivos de derivación desde AP a asistencia especializada (demanda derivada) y de la concordancia diagnóstica entre médico de AP y dermatología/anatomía patológica.
Material y métodosSe recogieron datos de 755 pacientes y 882 primeras consultas de Dermatología procedentes de AP, en el periodo comprendido entre el 1 de febrero de 2012 hasta el 30 de abril de 2012, a los que aplicamos un protocolo de recogida de datos (edad, sexo, profesión, motivo de derivación, diagnóstico de AP y de dermatología). Con los datos realizamos un estudio estadístico para conocer frecuencias, motivos de derivación, sensibilidad y especificidad y los valores predictivos positivos (VPP), valores predictivos negativos (VPN) e índices kappa de concordancia diagnóstica.
ResultadosLos diagnósticos más frecuentes fueron queratosis seborreicas, nevus melanocíticos, queratosis actínicas y acné. El motivo más frecuente de derivación fue la valoración diagnóstica (52,5%). La sensibilidad (S) y especificidad (E) del diagnóstico en tumores cutáneos fueron de S=22,4%, E=94,7%, VPP=40,7% y VPN=88,3%, κ=0,211 y en los diagnósticos más frecuentes la S en general es baja y la E bastante alta.
ConclusionesEl médico de AP, de acuerdo con nuestros resultados, está más capacitado para afirmar que el paciente no padece determinada enfermedad cutánea (E alta) que para establecer el verdadero diagnóstico clínico (S baja), lo que nos sugiere la necesidad de planificar acciones formativas que se traduzcan en una aumento de los conocimientos y aptitudes necesarias para el correcto manejo de las enfermedades cutáneas, especialmente por su trascendencia del cáncer de piel. Sin duda redundaría en una mayor agilidad del sistema, menos listas de espera y una mejor atención sanitaria.
Skin diseases are one of the main reasons for seeking primary health care,1 thus reflecting their high prevalence in the community.2–4 Frequency varies from 5.5% to 22.5% between studies.2,4,5 However, subsequent studies estimate prevalence to be around 7% to 8%.6,7 Skin diseases are the sixth and seventh most common diseases in primary care,1,5,8 and up to 60% are resolved by nonspecialists.2,6,9
Primary care physicians must recognize the importance of skin diseases, accept the role they occupy in health care, and include them in their medical training, since many skin diseases are easily treated and generally do not require complex diagnostic techniques.10 Primary care physicians are the patient's first contact with the health system and should be able to correctly diagnose the most common skin diseases in their setting. They should also know the criteria for referral to a specialist and the drugs most frequently used in the treatment of these diseases. The increasing incidence of skin cancer requires primary and secondary prevention strategies to reduce incidence and mortality. The very low diagnostic agreement among primary care physicians recorded in some studies, together with delays in initiating appropriate treatment, can create considerable problems in health care.11,12
Referral of patients from primary care to specialized care accounts for a considerable part of primary care activity, since it is key to reducing costs and increasing the safety, efficacy, and effectiveness of health care.13–16
In the present study, we aim to know the most common reasons for referral to dermatology in primary care in Spain, the characteristics of referral demand, and the diagnostic agreement between primary care physicians and dermatologists. The data collected could be used to design specific training activities.17–19
ObjectivesTo determine diagnostic agreement between primary care physicians and dermatologists and to compare the sensitivity and specificity of diagnoses by the former with those of the latter.
Materials and MethodsData were collected prospectively at the Dermatology Clinic of Hospital Santa Ana de Motril, Motril, Spain a center with a catchment population of 104 000 inhabitants in the Granada Sur health district, which includes towns on the Granada coast and in the Alpujarra. Data were collected for 755 patients and 882 initial dermatology appointments from February 1, 2012 through April 30, 2012 following primary care referral.
The primary care diagnosis was made based on symptoms; the dermatology diagnosis was based on symptoms in inflammatory conditions and histopathology in cutaneous tumors and in skin diseases in which the diagnosis was unclear. The data collected from each patient included personal details, age, sex, occupation, reason for referral, diagnosis in primary care, and final diagnosis. Data were analyzed using the SPSS statistical software package version 15. Diagnoses were coded according to the International Classification of Diseases (ICD), Tenth Revision.20 Occupations were classified according to the International Standard Classification of Occupations,21 to which we added the categories homemaker, retiree, unemployed, and student. First, we performed a descriptive analysis of the sample. In order to determine the most frequent diagnoses, we analyzed frequencies, percentages, and the cumulative percentage of all the diagnoses made both by primary care physicians and by dermatologists. For the analysis, we drew up contingency tables and calculated the κ statistic for diagnostic agreement. We calculated the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) to compare the value of the primary care physician's diagnosis with that of the dermatologist.
ResultsAge ranged from 1 to 92 years (mean, 45.55); 40.5% were men and 59.5% women. The most common occupation was homemaker (18.5%), followed by student (13.51%), and farmer (13.11%). Most of the remaining patients worked in the services sector.
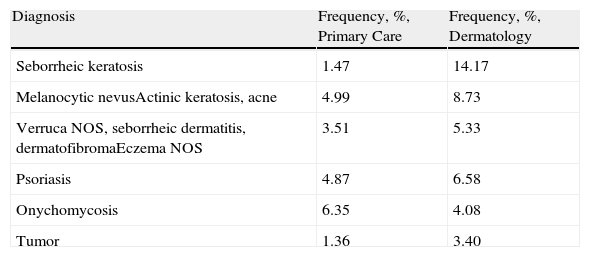
The main reason for referral from primary care to dermatology was diagnostic assessment (52.5%). In the remainder, the reason for referral was not specified (22.2%), a diagnosis was not provided (25%), and the referral was only accompanied by a description of the disease (18.1%). The most frequent diagnoses in primary care and dermatology are shown as percentages in Table 1.
Main Diagnoses (%) in Primary Care and Dermatology.
| Diagnosis | Frequency, %, Primary Care | Frequency, %, Dermatology |
| Seborrheic keratosis | 1.47 | 14.17 |
| Melanocytic nevusActinic keratosis, acne | 4.99 | 8.73 |
| Verruca NOS, seborrheic dermatitis, dermatofibromaEczema NOS | 3.51 | 5.33 |
| Psoriasis | 4.87 | 6.58 |
| Onychomycosis | 6.35 | 4.08 |
| Tumor | 1.36 | 3.40 |
Abbreviation: NOS, not otherwise specified.
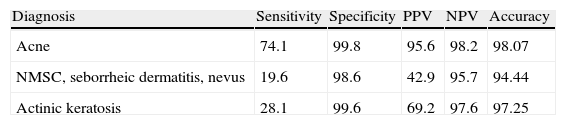
We calculated the sensitivity, specificity, PPV, NPV, and total diagnostic accuracy of the primary care physician for the main diagnoses (Table 2). The sensitivity of the clinical diagnosis was 46.48% for the most common conditions. In the case of skin tumors, including nonmelanoma skin cancer and melanoma, the sensitivity of the primary care diagnosis was 22.40%, with a specificity of 94.7%, PPV of 40.7%, and NPV of 88.3%. We drew up a contingency table for tumors to establish diagnostic agreement between primary care and dermatology. The κ statistic was 0.211, indicating poor agreement.
Values for the Diagnosis of the Most Common Skin Diseases in Primary Carea
| Diagnosis | Sensitivity | Specificity | PPV | NPV | Accuracy |
| Acne | 74.1 | 99.8 | 95.6 | 98.2 | 98.07 |
| NMSC, seborrheic dermatitis, nevus | 19.6 | 98.6 | 42.9 | 95.7 | 94.44 |
| Actinic keratosis | 28.1 | 99.6 | 69.2 | 97.6 | 97.25 |
Abbreviations: NMSC, nonmelanoma skin cancer; NPV, negative predictive value; PPV, positive predictive value.
The results showed that the mean age of patients referred from primary care to dermatology during the study period was 45.5 years. This finding is consistent with those published by Macaya-Pascual et al.22 (45.7 years) in their study on the reasons for consultation in primary care and is close to that of Valcayo et al.,7 (45.7 years). Mean age was close to that reported by Gil et al.23 (49 years) in their study on dermatologic emergencies. Consequently, patients consulting for skin complaints are generally aged around 45 to 50 years.
As for distribution by sex, 40.4% were men and 59.5% women. This finding is consistent with those of Valcayo et al.7 (43.6% for men and 56% for women), Macaya-Pascual et al.22 (39.4% men and 60.6% women), and González et al.24 (43.3% men and 56.6% women). We found that a higher percentage of women consult for skin complaints; therefore, the number of referrals to dermatology was greater. These differences could be due to a greater concern for body image on the part of women, as evidenced in other studies.23–29
The most common occupations of the patients are clearly the result of the socioeconomic and demographic factors that are typical of the area where the study was carried out, namely, the Granada coast and the Alpujarra, where the population is predominantly rural. Consequently, and given that both seborrheic keratosis and melanocytic nevus are the most common diagnoses referred for evaluation and actinic keratosis and verrucae not otherwise specified are the most common diagnoses referred for specific treatment, we can conclude that a more in-depth knowledge of these conditions and the application of relatively simple and rapid treatments could significantly reduce demands on dermatology stemming from primary care and thus help to reduce waiting lists and relieve the overload in dermatology departments.
It is noteworthy that no reason for referral was given in 22.2% of cases, thus directly affecting the quality of the referral. This finding could be explained by time restrictions affecting family physicians, although it is key to a fluid relationship between both care levels. In addition, it would directly affect not only the patient's care, but also the patient's perception of the health care received.24
As for the association with the quality of the referral, it is also noteworthy that on the referral form, 25% of primary care physicians do not provide an accurate diagnosis and only 18.1% describe the lesion. This is understandable, given that the patient is often referred because no clear diagnosis has been reached. In addition, the diagnoses made by the family practitioner generally correspond to a more generic ICD diagnosis, which may be admissible if the condition is considered a syndrome. However, in 6.9% of cases, in which no presumptive diagnosis was made, it does seem reasonable to think that the quality of the referral is reduced. The study by Porta et al.11 reveals somewhat different figures, stating that descriptive referral forms were found in 32.7% of cases, whereas those providing a suspected diagnosis were more numerous (59.67% of the total). Physicians from old-style clinics that had not yet been converted to health centers were the professionals who least often included a suspected diagnosis.
According to some studies,11,30,31 overall diagnostic agreement between family practitioners and dermatologists is between 40% and 60%. Studies such as that of Porta et al.,11 on the other hand, reveal κ indices of 1 and PPVs of 100% in the case of specific diagnoses such as acne, distension striae, hyperhidrosis, impetigo, hirsutism, burns, or leukoplasia; nevertheless, they do report low κ indices for other diseases such as basal cell carcinoma (0.198), seborrheic keratosis (0.19), and molluscum contagiosum (0.221). The results for tumors (basal cell carcinoma, squamous cell carcinoma, and melanoma), whose diagnosis is particularly important, show low agreement (0.211) between the primary care physician and the dermatologist. In the diagnoses set out above, the PPV for primary care physicians is 40.7% (percentage of patients diagnosed by a primary care physician whose diagnosis is confirmed by a dermatologist) and the NPV is 88.3%. The data reveal low sensitivity (22.4%) and high specificity (94.7%): the primary care physician is more confident ruling out those cases that are not tumors, yet is more doubtful with respect to cases that are true positives. As for pigmented tumors, primary care physicians diagnosed 4 cases of melanoma, only 1 of which was confirmed. Melanocytic nevi are one of the most common diagnoses made by the dermatologist; in other words, some cases of melanocytic nevi are referred from primary care probably to ensure a correct diagnosis and thus rule out melanoma. Therefore, the primary care physician tries to increase sensitivity for melanoma so that no cases go undiagnosed and potentially serious mistakes are not made. The study data show that this is particularly true when the κ statistic is very high for the dermatologist (0.795) in the diagnosis of basal cell carcinoma, squamous cell carcinoma, and melanoma compared with pathology reports. Furthermore, the dermatologist has a PPV for the above-mentioned diagnoses of 88.2% and an NPV of 91.3%.
In any case, identification of the main diagnoses referred from primary care seems to be a good starting point in terms of programming continued training in dermatology for primary care physicians. Such an approach will better optimize the health system and improve patient care.
Ethical DisclosuresProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Castillo-Arenas E, Garrido V, Serrano-Ortega S. Motivos dermatológicos de consulta en atención primaria. Análisis de la demanda derivada. Actas Dermosifiliogr. 2014 105:271–275.