The keystone flap is a fasciocutaneous flap supplied by perforating arteries. It is used in dermatology to repair surgical defects in areas with low skin extensibility (the upper and lower limbs and the back). We review the clinical experience gained with keystone flap reconstruction at our hospital and report on the surgical outcomes.
Material and methodsDescriptive retrospective study of patients with malignant skin tumors on the lower limbs who underwent keystone flap reconstruction.
ResultsEighteen patients (mean age, 77.83 years) underwent keystone flap reconstruction using the Behan technique in 17 cases and the modified Moncrieff technique in one. Basal cell carcinomas accounted for 38.8% of the tumors excised, squamous cell carcinomas 33.3%, and malignant pigmented tumors 27.7%. Cardiovascular risk factors were observed in 72.2% of patients. Minor complications occurred in 38.8% of patients, and there were no cases of partial or total flap necrosis.
ConclusionsWe consider the keystone flap to be a good alternative to other flaps and grafts for the surgical reconstruction of lower limb defects. The success rate was high, and the cosmetic and functional outcomes were good.
El colgajo de keystone es un colgajo fasciocutáneo cuya vascularización proviene de las arteriolas perforantes musculares. Su aplicación en dermatología es para cubrir defectos en zonas de piel poco distensible (miembros inferiores, superiores y de la espalda). Presentamos nuestra experiencia clínica y los resultados quirúrgicos del centro.
Material y métodosEstudio descriptivo retrospectivo de pacientes con tumores cutáneos malignos en miembros inferiores en los que se realizó el colgajo de keystone.
ResultadosSe operaron 18 pacientes con una edad media de 77,83 años. Se realizaron 17 mediante la técnica propuesta por Behan y uno con la técnica modificada de Moncrieff. El 38,8% de los tumores extirpados fueron carcinomas basocelulares, el 33,3% carcinomas epidermoides y el 27,7% tumores malignos pigmentados. El 72,22% presentaba algún factor de riesgo cardiovascular. Se observó un 38,8% de complicaciones menores y ningún caso de necrosis parcial o total del colgajo.
ConclusionesConsideramos que el colgajo de keystone es una buena alternativa terapéutica a otros colgajos e injertos para la reconstrucción de defectos en miembros inferiores. Los resultados estéticos y funcionales son buenos, con una tasa de éxito elevada.
The keystone flap was first described in 2003 by Behan1 as an alternative to skin grafts and other flaps used to cover medium and large skin defects. The flap is a fasciocutaneous flap irrigated by vascular perforators. The name is borrowed from the architectural term keystone, referring to the central stone that supported the weight of Roman arches.
We present our clinical experience in the use of this flap to cover medium-sized defects on the legs.
Materials and MethodsIn this descriptive, retrospective study, 18 patients with malignant skin tumors on the legs underwent keystone flap reconstruction. The technique was performed in the University Hospital Rey Juan Carlos, in Mostoles (Madrid), Spain between July 2013 and May 2017. No patient was excluded from the study. The clinical and demographic characteristics of the patients are described, along with the histopathological findings of tumor biopsy, the defect size, and associated side effects.
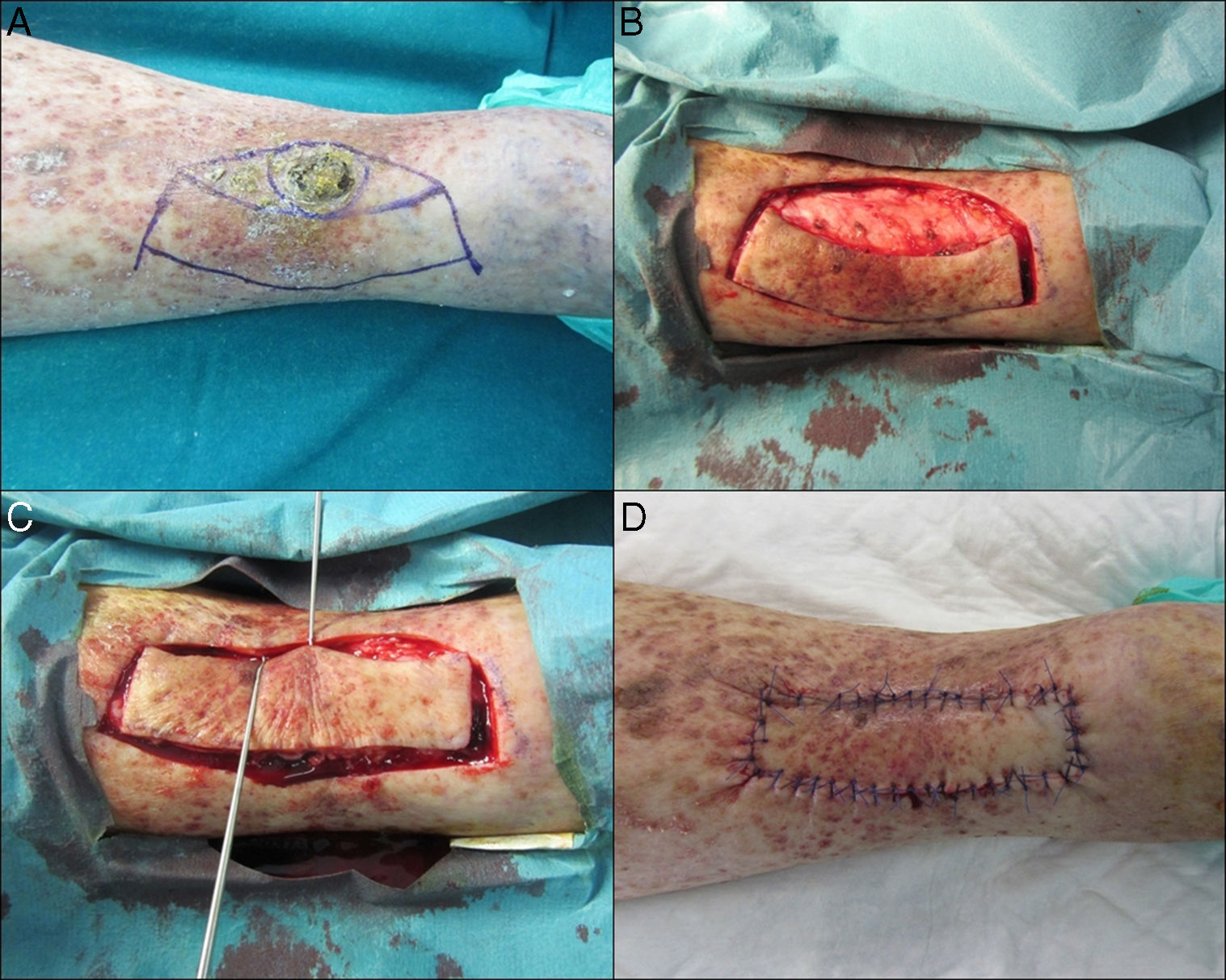
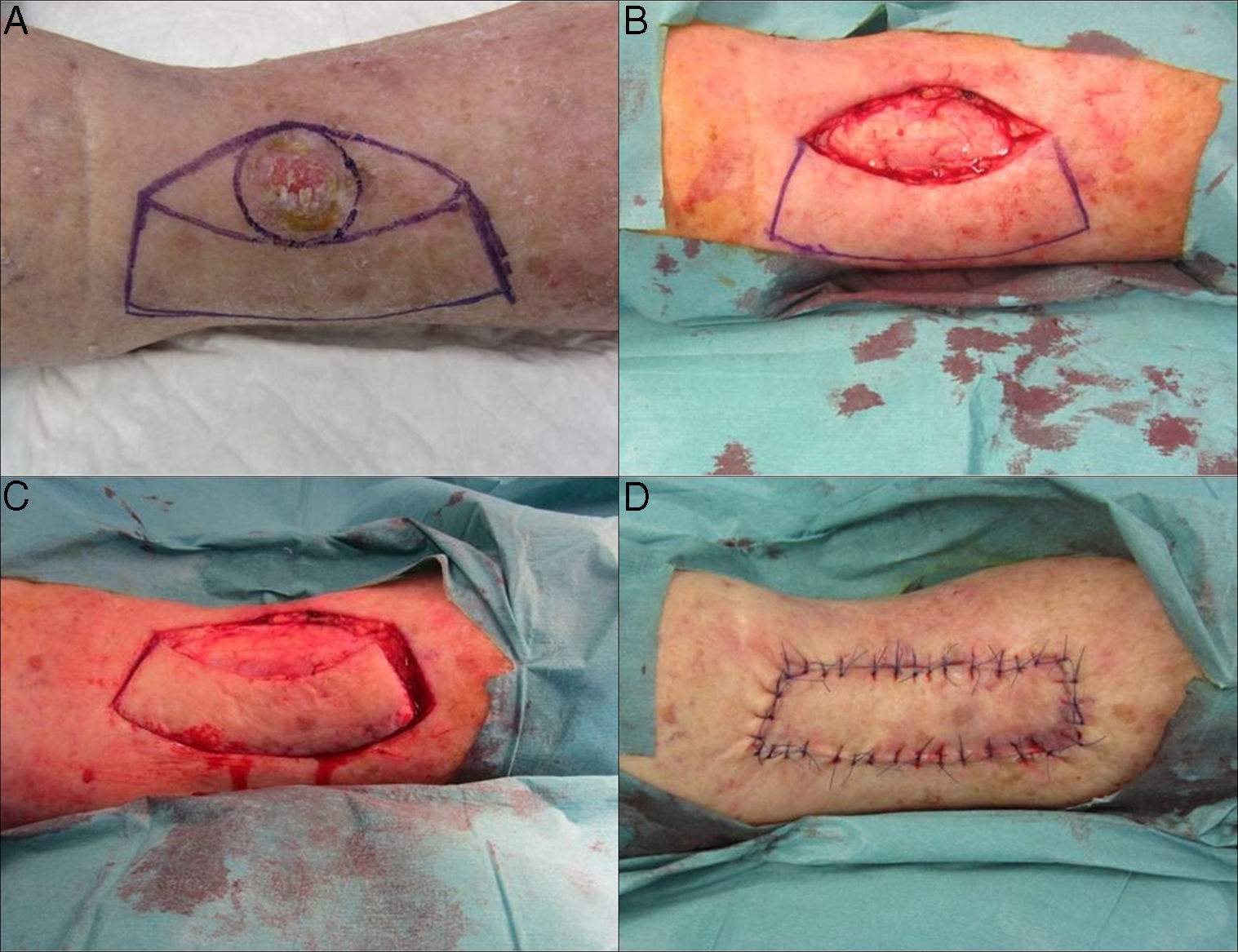
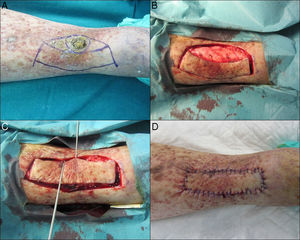
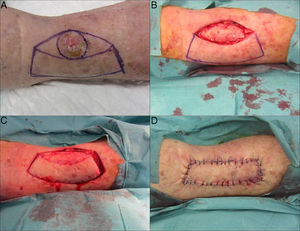
TechniqueWe performed 17 keystone flap reconstructions according to the classic Behan technique1 (Figs. 1 and 2), and 1 according to the modified Moncrieff technique.2 After application of mepivacaine 2% to the area as local anesthetic, local primary tumors were removed by fusiform excision and the flap was constructed, sparing the vascular perforators. From the anatomical area with greatest mobility, in most cases from the posterior compartment of the leg, a flap of the same width as the defect was marked. Each corner of the flap formed a 90° angle. The final shape of the flap was an arched trapezoid like a keystone. Simple suture was used with nonresorbable 3/0 and 2/0 stitches. In some cases, V-Y advancement of each end of the flap was needed for full closure.
In the case of the modified keystone flap procedure, partial dissection only was performed of the arch, leaving a central area of healthy skin that contributed to dermal vascularization.
All surgical procedures were performed in the outpatient setting; admission to hospital was not required for any patients.
As these flaps required substantial tension, a regimen of 7-10 days of antibiotics was started after surgery. Amoxicillin-clavulanic acid was the treatment of choice if there were no contraindications. Patients were recommended relative rest, and no antithrombotic prophylaxis was required.
In all cases, the first dressing change was performed in hospital 48-72hours after surgery to ensure flap viability. The stitches were removed after 14-18 days. The duration of patient follow-up varied depending on the malignant tumor that had been excised.
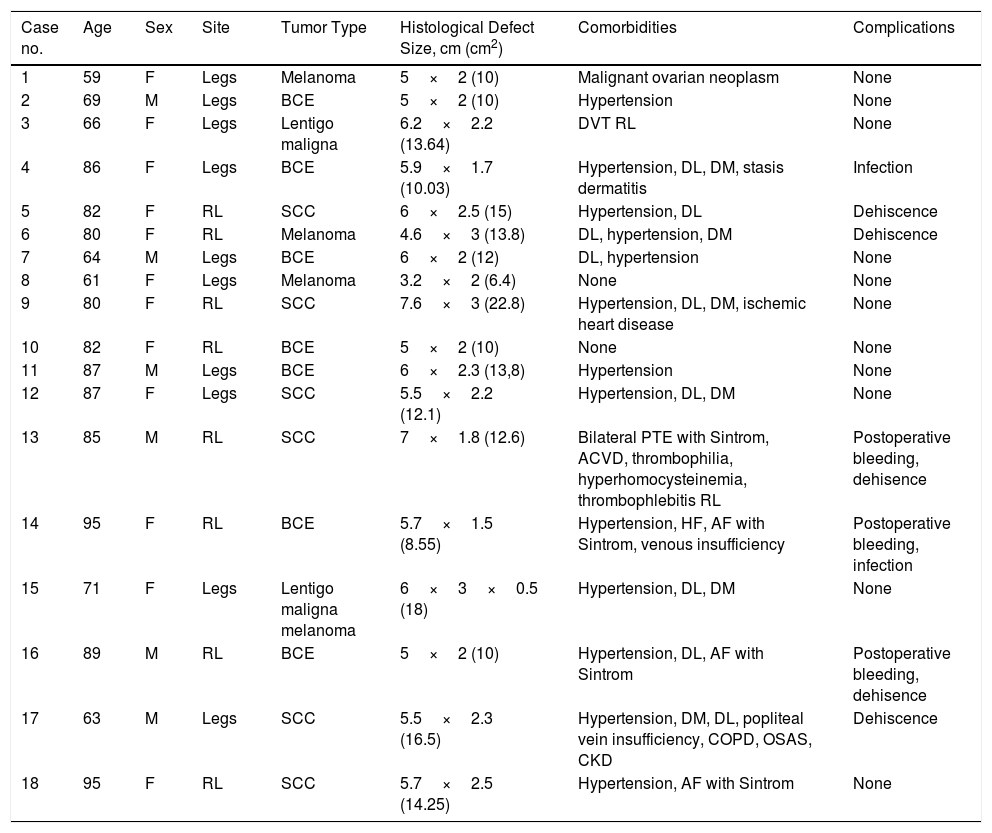
ResultsA total of 18 flap procedures were performed (Table 1). Twelve of these were in women and 6 in men (ratio 2:1). The oldest patient was aged 95 years and the youngest 59 years, with a mean age of 77.83 years. The malignant tumors excised were as follows: 7 basal cell epitheliomas, 6 squamous cell carcinomas, and 5 malignant pigmented tumors (malignant melanoma, lentigo maligna, and lentigo maligna melanoma). All lesions were located on the legs.
Epidemiological Characteristics of the Patients and Tumor Type, Size, and Complications.
| Case no. | Age | Sex | Site | Tumor Type | Histological Defect Size, cm (cm2) | Comorbidities | Complications |
|---|---|---|---|---|---|---|---|
| 1 | 59 | F | Legs | Melanoma | 5×2 (10) | Malignant ovarian neoplasm | None |
| 2 | 69 | M | Legs | BCE | 5×2 (10) | Hypertension | None |
| 3 | 66 | F | Legs | Lentigo maligna | 6.2×2.2 (13.64) | DVT RL | None |
| 4 | 86 | F | Legs | BCE | 5.9×1.7 (10.03) | Hypertension, DL, DM, stasis dermatitis | Infection |
| 5 | 82 | F | RL | SCC | 6×2.5 (15) | Hypertension, DL | Dehiscence |
| 6 | 80 | F | RL | Melanoma | 4.6×3 (13.8) | DL, hypertension, DM | Dehiscence |
| 7 | 64 | M | Legs | BCE | 6×2 (12) | DL, hypertension | None |
| 8 | 61 | F | Legs | Melanoma | 3.2×2 (6.4) | None | None |
| 9 | 80 | F | RL | SCC | 7.6×3 (22.8) | Hypertension, DL, DM, ischemic heart disease | None |
| 10 | 82 | F | RL | BCE | 5×2 (10) | None | None |
| 11 | 87 | M | Legs | BCE | 6×2.3 (13,8) | Hypertension | None |
| 12 | 87 | F | Legs | SCC | 5.5×2.2 (12.1) | Hypertension, DL, DM | None |
| 13 | 85 | M | RL | SCC | 7×1.8 (12.6) | Bilateral PTE with Sintrom, ACVD, thrombophilia, hyperhomocysteinemia, thrombophlebitis RL | Postoperative bleeding, dehisence |
| 14 | 95 | F | RL | BCE | 5.7×1.5 (8.55) | Hypertension, HF, AF with Sintrom, venous insufficiency | Postoperative bleeding, infection |
| 15 | 71 | F | Legs | Lentigo maligna melanoma | 6×3×0.5 (18) | Hypertension, DL, DM | None |
| 16 | 89 | M | RL | BCE | 5×2 (10) | Hypertension, DL, AF with Sintrom | Postoperative bleeding, dehisence |
| 17 | 63 | M | Legs | SCC | 5.5×2.3 (16.5) | Hypertension, DM, DL, popliteal vein insufficiency, COPD, OSAS, CKD | Dehiscence |
| 18 | 95 | F | RL | SCC | 5.7×2.5 (14.25) | Hypertension, AF with Sintrom | None |
Abbreviations: ACVA, acute cerebrovascular accident; AF, atrial fibrillation; BCE, basal cell epithelioma; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; DL, dyslipidemia; DM, diabetes mellitus; DVT, deep vein thrombosis; F, female; HF, heart failure; M, male; OSAS, obstructive sleep apnoea syndrome; PTE, pulmonary thromboembolism; RL, right leg; SCC, spindle-cell carcinoma.
The largest lesion excised was 2.5cm in diameter (6.25cm2) and the smallest 0.8×0.7cm (0.56cm2), with a mean area of 2.98cm2. The maximum resulting defect size after flap design was 7.6×3cm (22.8cm2) and the minimum defect size was 3.2×2cm (6.4cm2), with a mean area of 12.74cm2.
Regarding comorbidities in these patients, 13 (72.2%) had cardiovascular risk factors, 46.15% had diabetes, and 100% had hypertension. One patient had had at least one episode of ischemic heart disease and another had had cerebrovascular accident (15.38% of the total). Two patients had presented with an episode of thrombosis (deep vein thrombosis and pulmonary thromboembolism) and 4 patients (30.76%) were receiving treatment with acenocoumarol. One patient (7.69%) had a history of malignant neoplasm and only 3 patients had a history of chronic venous insufficiency or stasis dermatitis.
During follow-up (median duration, 19 months), 7 patients (38.8%) had a surgical wound complication. In 27.7% of patients, partial dehiscence of the surgical wound was observed. In 11.1%, some sign of infection after finishing the prophylaxis regimen was observed. In these patients, antibiotic treatment was administered according to susceptibility testing after taking a sample for culture. Three of the 4 patients who were in treatment with acenocoumarol experienced postoperative bleeding. Although none of these bleeding events was severe, acenocoumarol was replaced by low molecular weight heparin therapy. Those patients who were receiving antiplatelet therapy alone did not require any changes to their regimen. No cases of partial of total flap necrosis were observed.
Our patients experienced moderate postoperative pain that was controlled with usual analgesics. This pain resulted from the tension arising from skin displacement.
The 18 flaps had good cosmetic and functional outcomes. Those that showed partial dehiscence closed satisfactorily by second intent. No repeat operations were required.
DiscussionClosure of skin defects on the legs is a therapeutic challenge for dermatologists. In most cases, the patients are elderly with deterioration of peripheral vascularization and reduced skin mobility.
The reconstructive techniques used for closure of medium-large sized defects on the legs are skin grafts and skin flaps. Rotation, advancement, or transposition flaps can be used on the legs. The main problem is the lack of skin mobility, which is associated with a substantial increase in the risk of necrosis. On the other hand, full thickness skin grafting requires prolonged immobilization of the patient; is associated with higher rates of total/partial necrosis and postoperative dressing changes; and, at times, worse cosmetic outcomes.2–5
Behan1 therefore proposed the keyhole flap procedure as an alternative to these approaches. Vascular perforators pass through the muscular fascia, directly feeding the dermis and subcutaneous tissue. These vessels provide sufficient irrigation for the flap to survive and favor earlier wound healing.1,5
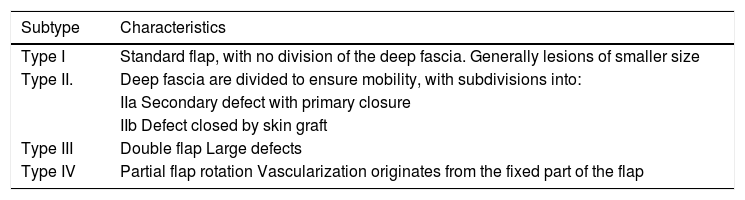
There are 4 main subtypes of keystone flap (Table 2). Type I is the standard one, used for medium-sized lesions. The 3 remaining types are modifications of the standard flap and are used to cover larger defects.1 In 2008, Moncrieff et al.2 designed the modified keystone flap. This approach was used in 1 of our cases. In this alternative, additional vascularization is provided through dermal vessels. In a series of 176 patients, the Moncrieff variant demonstrated a lower rate of complications than with the standard flap.3 The other keystone flap variants are the yin-yang flap,6 omega flap,7 and modifications to subtypeIV which cover larger defects.
Subtypes of Keystone Flaps Proposed by Behan.
| Subtype | Characteristics |
|---|---|
| Type I | Standard flap, with no division of the deep fascia. Generally lesions of smaller size |
| Type II. | Deep fascia are divided to ensure mobility, with subdivisions into: |
| IIa Secondary defect with primary closure | |
| IIb Defect closed by skin graft | |
| Type III | Double flap Large defects |
| Type IV | Partial flap rotation Vascularization originates from the fixed part of the flap |
Keystone flaps should have certain specific characteristics to survive. The defect has to have the same width as the flap. This allows redistribution of skin tension and avoids dehiscence and necrosis. The main disadvantage of the standard keystone flap is that it is difficult to use in large defects. Although it is generally recommended for defects smaller than 3cm, it is important to take into account anatomical and individual patient characteristics, such as skin mobility or whether or not underlying diseases are present that may limit the use of this technique. In these cases, variants of the same procedure or other flaps or grafts could be used.3
Their longitudinal orientation preserves the vascular perforators and lymphatic vessels, reducing the risk of distal lymphedema. In the modified Moncrief flap, the skin bridge preserves this venous and lymphatic return.2
We have described keystone flaps for defects on the legs, but the literature has examples of other uses8: in ophthalmology for eyelid reconstruction,9 in maxillofacial surgery for parotid defects,10 in general and gynecological surgery for perineal and vulvar defects,11 and in neurosurgery for defects in the dorsolumbar and lumbosacral area.12,13
The most extensive series published was that of Behan1 in 2003. That series included 300 patients treated with this reconstructive technique in different anatomical areas. The success rate was 99.6% (success was understood to mean absence of major complications). Subsequently, multiple case series have been published. We review the most relevant that include reconstructions on the legs.14–18
In 2011, Khouri et al.14 reported a series of 28 patients with 14 keystone flap procedures on the legs. They obtained a complication rate of 35.7% and only 1 of the 14 procedures had total flap necrosis. Rao and Janna16 reported 20 patients who underwent keystone flap procedures on the legs. The complication rate was 15% and the success rate 95% with only 1 case of partial flap necrosis. Recently, in 2017, a series of 60 keystone flap procedures was published (41.7% on the legs) with an overall complication rate of 40%, most of which (76%) were on the legs.17 These results show an overall complication rate on the legs (between 15% and 40%) similar to ours (38.8%). In our series, the success rate was 100% and we did not observe partial or total flap necrosis in any patient.
We have only found 1 prospective study that compares keystone flaps with other skin flaps.18 In 39 patients, keystone flap procedures were performed, while in 22, a rhomboid transposition flap procedure was performed. Patients with a range of anatomical sites were included. No statistically significant differences were observed in the rate of dehiscence between the 2 types of flap.
The only comparative study of the class keystone flap variant and the modified variant was published by Moncrieff et al.2 Those authors observed a lower incidence of major complications in the modified variant and an overall success rate close to 99% (only 2 of the 176 patients treated had total graft necrosis).
In conclusion, the keystone flap procedure is a reconstructive option for medium-sized defects on the legs. It is an alternative to full-thickness skin grafts and classic flap procedures. The cosmetic and functional outcomes are good. It is associated with less secondary edema and lower morbidity, and decreases the risk of skin necrosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Aragón-Miguel R, Gutiérrez-Pascual M, Sánchez-Gilo A, Sanz-Bueno J, Vicente-Martin FJ. Aplicación del colgajo de keystone en dermatología. Experiencia clínica en 18 pacientes. Actas Dermosifiliogr. 2018;109:515–520.