Dupilumab is a biologic drug that blocks the receptor of interleukins IL-4 and IL-13, and which has shown its efficacy in the treatment of severe atopic dermatitis (AD).1–3 Although the results of dupilumab in real clinical practice are limited, our own experience has shown a behavior similar to that obtained in prior clinical trials.4,5 Other researchers, however, have observed a higher incidence of adverse effects (AEs), mainly eye disorders and transitory eosinophilia.6 Given this disagreement and because the mechanism of action is completely novel, we believe that is is useful to examine in greater depth the safety profile resulting from blocking this immune pathway.
In clinical trials, the most common AEs were infections and infestations, eye disorders, site-of-injection reactions, headache, and skin infection (non-herpes and herpes), although the incidence was, in general, low. Indeed, the incidence of severe AEs that led to suspension of the drug was less than in the placebo arm,1,2 which indicates that this mechanism of action has a favorable safety profile. Dupilumab appears to be linked to a reduction in the incidence of skin infections and eczema herpeticum in adults with moderate to severe AD. The underlying mechanism of this link is unclear, but it seems likely that it is associated with the improvement of the AD.6
Of the novel AEs observed in treatment with dupilumab, a greater incidence of ocular AEs, principally allergic conjunctivitis, was noted in the treatment groups. Most cases were moderate or severe and were self-limiting; no severe cases were recorded. The trials appear to show a tendency to greater severity of these eye disorders in older patients, with a longer duration of AD, who had a more active underlying disease and, especially, a prior history of eye disease.1–3
Some authors suggest that the cases of allergic conjunctivitis may in reality be cases of keratoconjunctivitis, often associated with the AD itself, in which blockade of IL-4 and IL-13 signalling may increase the activity of specific ligands involved in the atopic keratoconjunctivitis in the eye, which would suggest a mechanism dependent on the AD and not necessarily related to dupilumab. Furthermore, not all cases have been diagnosed by ophthalmologists, either in clinical trials or in clinical practice.7–10 Treatment of the conjunctivitis must include agents that can be administered for long periods of time and that have a favorable safety profile. Fluorometholone eye drops appear to be a safe option in the short term and 0.03% tacrolimus eye drops or ointment are a safe long-term option.
We analyzed a series of 30 patients from 5 hospitals in Andalusia, Spain, included in the extended use of dupilumab in Spain for adult patients with moderate to severe AD, for 52 weeks. The included population presented a significant disease load, with a mean time of 28.5 years since onset of the AD. The most frequent comorbidities in the baseline visit were allergic rhinitis (50%), conjunctivitis (38.8%), and extrinsic asthma (22.2%). All patients had received prior treatment with oral corticosteroids and 94.4% had been treated with cyclosporin.
The safety profile of dupilumab was evaluated at 4, 12, 24, and 52 weeks. The most frequent AE was conjunctivitis, with 5 (16%) reported cases. Other AE were cheilitis, a mild episode of AD, unilateral gynecomastia, and mouth ulcers. All the AEs were transitory and were successfully managed without the need to withdraw the drug.
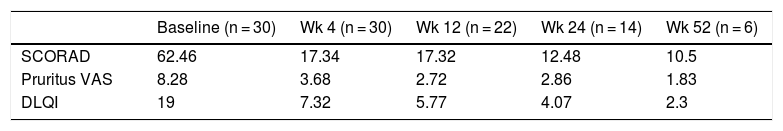
With regard to the effectiveness of treatment with dupilumab, in the baseline visit, the mean score was 59.4 on SCORAD scale, 8.3 on the pruritus VAS, and 19 on the DLQI. At week 52 of follow-up, the SCORAD score was 10.5 (a reduction of 82.3% compared to baseline), the pruritus VAS fell to 2.1 (a reduction of 74.4% compared to baseline), and the DLQI fell to 2 (a reduction of 89.5% compared to baseline). The results at the different cutoff points are shown in Table 1.
The clinical safety and the efficacy of dupilumab in our series were in line with those observed in the clinical trials. Conjunctivitis was considered to be the most frequent AE, but was treated by the dermatologists taking part in this study with ophthalmic corticosteroid eye drops and suspension of treatment was not required. Further, more extensive studies are required, with greater follow-up of the relationship between conjunctivitis and dupilumab to clarify its potential but ambiguous causal relationship, as this adverse event was not observed in studies of dupilumab for other indications, and it may be exclusive to the population with AD and, therefore, linked to the pathophysiology of the disease.
FundingThis study has not received funding of any kind.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ruiz-Villaverde R, Armario-Hita JC, Dominguez Cruz J, Pereyra-Rodriguez JJ. Análisis de seguridad de dupilumab en práctica clínica real. Experiencia a 52 semanas de cinco centros de referencia en Andalucía. Actas Dermosifiliogr. 2020. https://doi.org/10.1016/j.ad.2019.05.007