A 37-year-old man, with no personal or family history of interest presented with a 2-month history of asymptomatic lesions on his upper lip. He denied the occurrence of any hemorrhages and had not seen any ulcers in the lesions.
Physical examination revealed the presence of an erythematous nodule of a smooth surface and semi-solid consistency on the upper lip (fig. 1A), along with an additional asymptomatic papular lesion on the same mucosa (fig. 1B). Dermoscopy (fig. 1C) revealed the presence of a homogeneous red pattern with whitish areas surrounded by dilated tortuous vessels, some resembling a forked vascular pattern.
Smooth-surfaced erythematous nodule located on the upper lip of angiomatous appearance (A), erythematous papule in the upper lip internal mucosa (black arrow) (B). Homogeneous erythematous pattern with whitish areas and dilated tortuous vessels (Dermlite® DL4, Dermlite LLC, United States) (C).
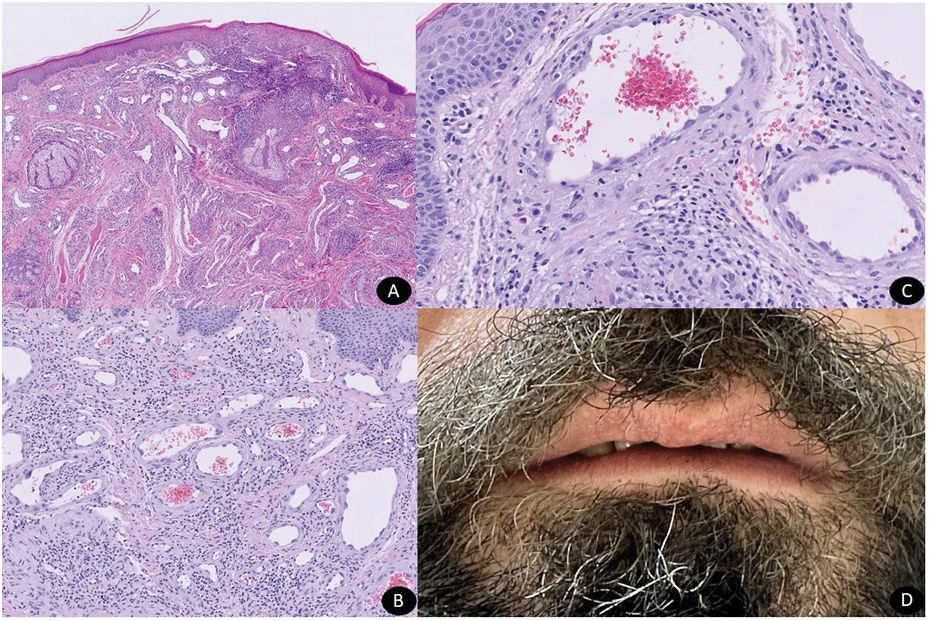
Histopathological examination of a 4mm punch biopsy confirmed the presence of an intradermal tumor lesion composed of a vascular proliferation of prominent endothelium, along with a predominantly lymphocytic inflammatory infiltrate with few interspersed eosinophils.
No additional tests were performed for diagnostic purposes.
What is the diagnosis?
Diagnosis and commentsThe diagnosis achieved was angiolymphoid hyperplasia with eosinophilia (ALHE).
Disease progression and treatmentAlthough the patient was informed about the possibility of spontaneous lesion resolution, he insisted on being treated, and received 2 sessions (595nm, 7mm diameter, 7J/cm2 fluence, and 0.5ms pulses; 2 pulses per lesion; air cooling) of pulsed dye laser (PDL), achieving complete resolution with an almost perfect aesthetic appearance (fig. 2A-C). The skin alterations did not relapse 6 months into treatment (fig. 2D).
Intradermal proliferation of lobulated vascular structures with prominent endothelium and inflammatory infiltrate (panoramic Hematoxylin & Eosin) (A). Prominent endothelial cells with abundant eosinophilic cytoplasm (H&E x10) (B). Prominent endothelial cells with abundant eosinophilic cytoplasm mainly surrounded by lymphocytes and a few isolated eosinophils (H&E x20) (C). Complete resolution of erythematous nodules after laser treatment.
ALHE is a subtype of epithelioid hemangioma, within benign angiolymphoproliferative processes, which is associated with a greater inflammatory component. It is a rare entity more prevalent in middle-aged women characterized by the appearance of erythematous-violaceous papules and nodules and is usually located on the head and neck. Lip or oral mucosa involvement is a rare finding,1 as it predominantly affects the periauricular area (36.3%), face (28.2%), and scalp (17.3%).2 Although these papules and nodules often remain asymptomatic, they may be associated with pruritus.2 Additionally, although their etiopathogenesis is unknown to this date, they could be due to reactive vascular proliferation in response to infections, hormonal factors, or trauma.3 The occurrence of ALHE after getting a tattoo done supports this latter hypothesis.4 Histological examination shows the proliferation of vascular structures of varying calibers with prominent epithelioid endothelial cells, along with a lymphocytic infiltrate and the presence of eosinophils.1
Differential diagnosis includes entities such as cutaneous epithelioid angiomatoid nodule (CEAN), cutaneous sarcoidosis, pyogenic granuloma, cutaneous lymphoma, Kaposi's sarcoma, and various types of epithelioid neoplasms. Among these, ALHE should be distinguished from other vascular epithelioid lesions such as epithelioid hemangioendothelioma, pseudomyogenic hemangioendothelioma, and epithelioid angiosarcoma (EA).
Histopathological characteristics and the use of an immunohistochemical panel are used to distinguish one entity from the other. Although ALHE generally expresses the switch regulatory protein 3 FosB,5 conditions such as pseudomyogenic hemangioendothelioma can also express it. Superficial location, good delimitation, and the absence of an infiltrative pattern with a low degree of nuclear atypia and mitotic figures, and negativity for podoplanin and avian myelocytomatosis viral oncogene homolog, distinguish ALHE from EA.5
The management of ALHE is not standardized. Excision is usually performed to treat single lesions, while therapies with variable results include topical and intralesional corticosteroids, cryocoagulation, pentoxifylline, or various laser modalities are used to treat multiple lesions.3,6 In published cases, PDL7 has turned out to be a safe therapy that improves symptoms and the aesthetic appearance of lesions, even leading to their disappearance, as it happened with our case. The mechanism of action of PDL induces photothermolysis, which eventually leads to the selective destruction of vascular lesions, thus reducing damage to surrounding structures, and facilitating faster healing compared with other therapies such as carbon dioxide.7 This has turned PDL into an attractive option for the management of ALHE since this is a benign condition that tends to recur frequently despite previous therapies.
FundingNone declared.
Conflicts of interestNone declared.