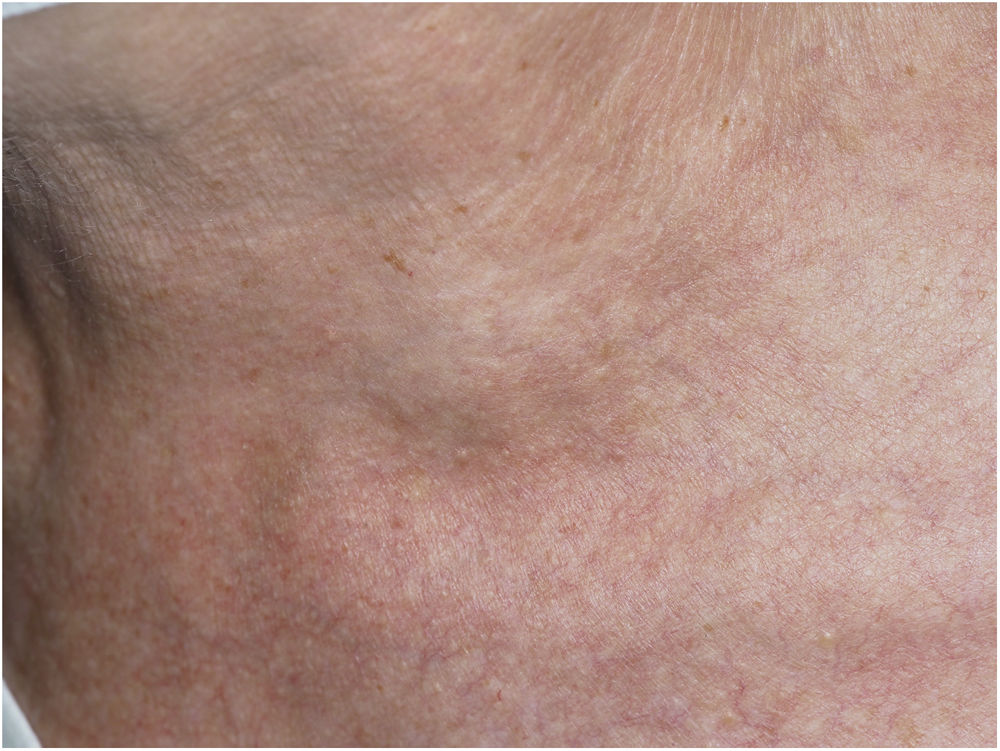
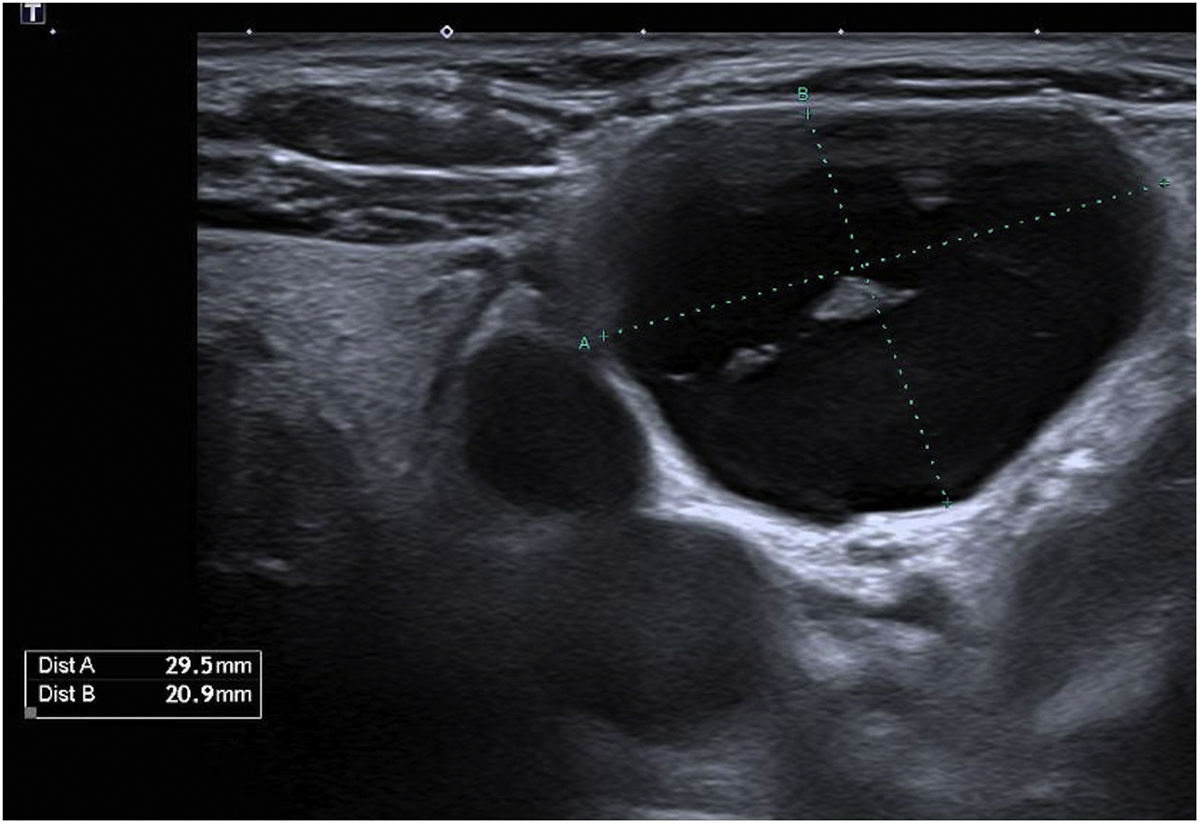
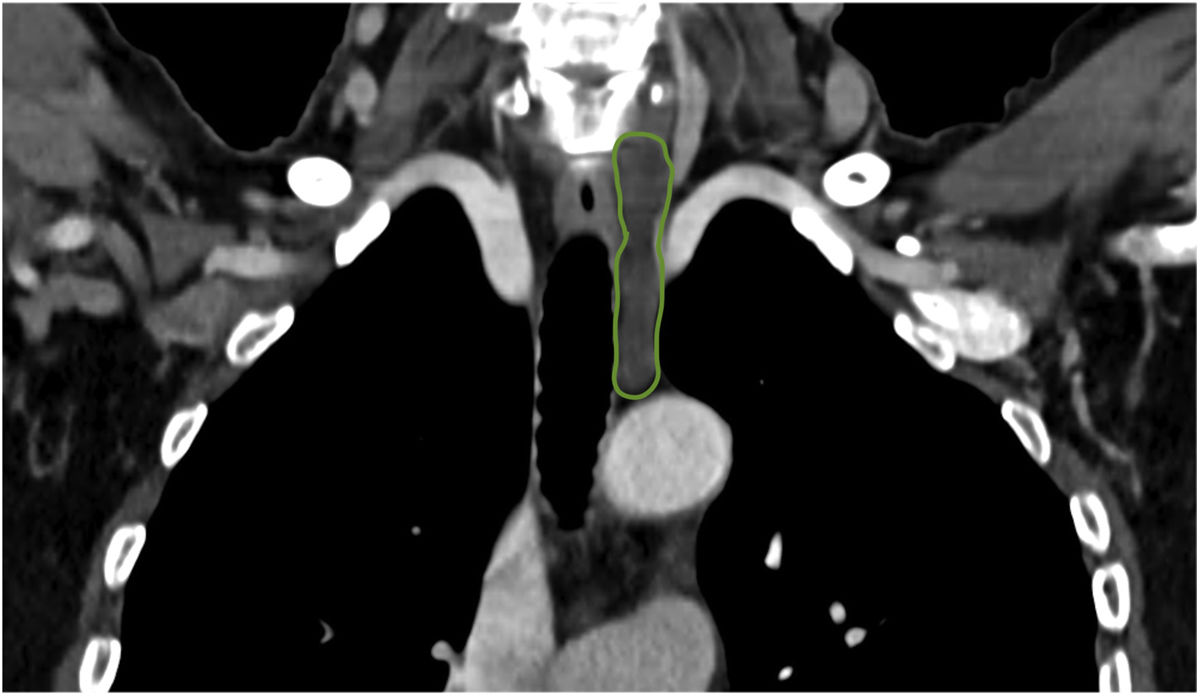
This is the case of a 66-year-old woman who presented to the dermatology office with a 6-month history of a lump on the left latero-cervical region without any accompanying symptoms. Her past medical story included thyroiditis and alfa-1 antitrypsin deficiency. The physical examination revealed the presence of a painless and non-inflamed 3cm nodule on the left latero-cervical region (Fig. 1). The neck ultrasound performed revealed the presence of a 3cm×2.1cm cyst with no peripheral or internal vascularity, which was consistent with a cyst (Fig. 2). The ultrasound-guided FNA and biochemical study of the content revealed the presence of elevated triglyceride levels (438mg/dL; normal range <150mg/dL), with normal cholesterol levels (82mg/dL; normal range <200mg/dL). To rule out any organic or treatable disease, a thoracic CAT scan was performed (Fig. 3).
What is your diagnosis?
DiagnosisSpontaneous cervical thoracic duct cyst (CTDC)
Evolution and treatmentConservative management was decided with the patient. This treatment was based on a low fat and medium-chain triglyceride diet. Only if these measures are not effective, we would suggest surgical treatment.
DiscussionCTDC represents a rare clinical problem with a relatively unclear etiology possibly associated with congenital wall weakness, the duct distal obstruction, and wall degeneration or trauma.1–3
Thoracic duct is a long, whitish-gray conductor with thin, flexible walls. It is formed by the union of the two lumbar lymphatic trunks. From its origin, it runs along the right border of the aorta and follows the posteromedial surface of the left subclavian artery. It reaches the base of the neck and forms a concave downward curve that reaches systemic circulation at the venous angle of the left subclavian and internal jugular vein.4 This location – where the duct empties into the internal jugular and left brachiocephalic vein – is where CTDC often appears.5
CTDC often presents as a painless and asymptomatic cystic mass on left supraclavicular region. However, it can cause swelling, discomfort, vague neck pain, dyspnea, cough, mild dysphagia, palpitations, arm swelling and sore throat following the compression of proximal structures.1
Imaging modalities like ultrasonography, computerized tomography, and magnetic resonance imaging help us achieve the diagnosis and trim down some of de differential diagnosis. Cystic lesions are characterized by a well-demarcated round or oval with lack of nodularity, septations, or contrast enhancement. The most important Imaging modality for diagnostic purposes is the ultrasound-guided fine needle aspiration (FNA) of the cystic mass. Fluid with lymphocyte predominance and very high levels of triglycerides and chylomicrons (fat content, 0.4–4%) are highly suspicious for lymphatic cyst.1,2,4 Lymphangiography is the “gold standard” regarding imaging modalities and the diagnosis of thoracic duct malformations. However, with the ease and availability of high-resolution imaging and FNA, lymphangiography is often not attempted.2
Options for the management of CTDC include conservative measures, and surgical intervention. Despite being a benign asymptomatic lesion, the most common approach is surgical excision with ligation of the thoracic duct. Conservative treatment is used in several patients with asymptomatic masses including observation, dietary changes (limiting medium-chain fatty acids), and external compression. Other options are sclerotherapy, repeated aspirations, embolization,1 or cyst-venous anastomosis.2
The presence of a new-onset supraclavicular mass should be studied because it elicits a wide range of differential diagnoses from benign to malignant lesions.1
Spontaneous and asymptomatic supraclavicular thoracic duct cysts on the neck are rare. However, this entity must be considered as a possibility. No gold standard has been stablished for the management of CTDC so a decision should be made along with the patient.
Conflict of interestThe authors declare that they have no conflict of interest.