There is a spectrum of sebaceous neoplasms, ranging from indolent lesions to sebaceous carcinoma. The nomenclature used in the literature is somewhat controversial, and to date no standardized classification scheme exists.1 Sánchez Yus and coworkers2 suggested that sebaceous adenoma and sebaceoma represent 2 extremes of a spectrum of benign neoplasms with sebaceous differentiation and differing degrees of maturation, with higher and lower percentages of mature cells, respectively, and proposed the term sebomatricoma to describe this spectrum. We present 2 cases that illustrate the usefulness of reflectance confocal microscopy (RCM) for the diagnosis and characterization of sebomatricoma.
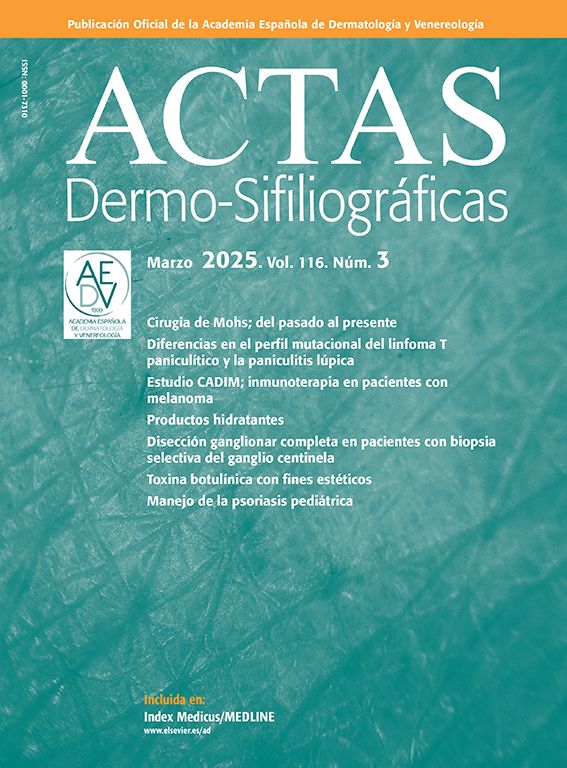
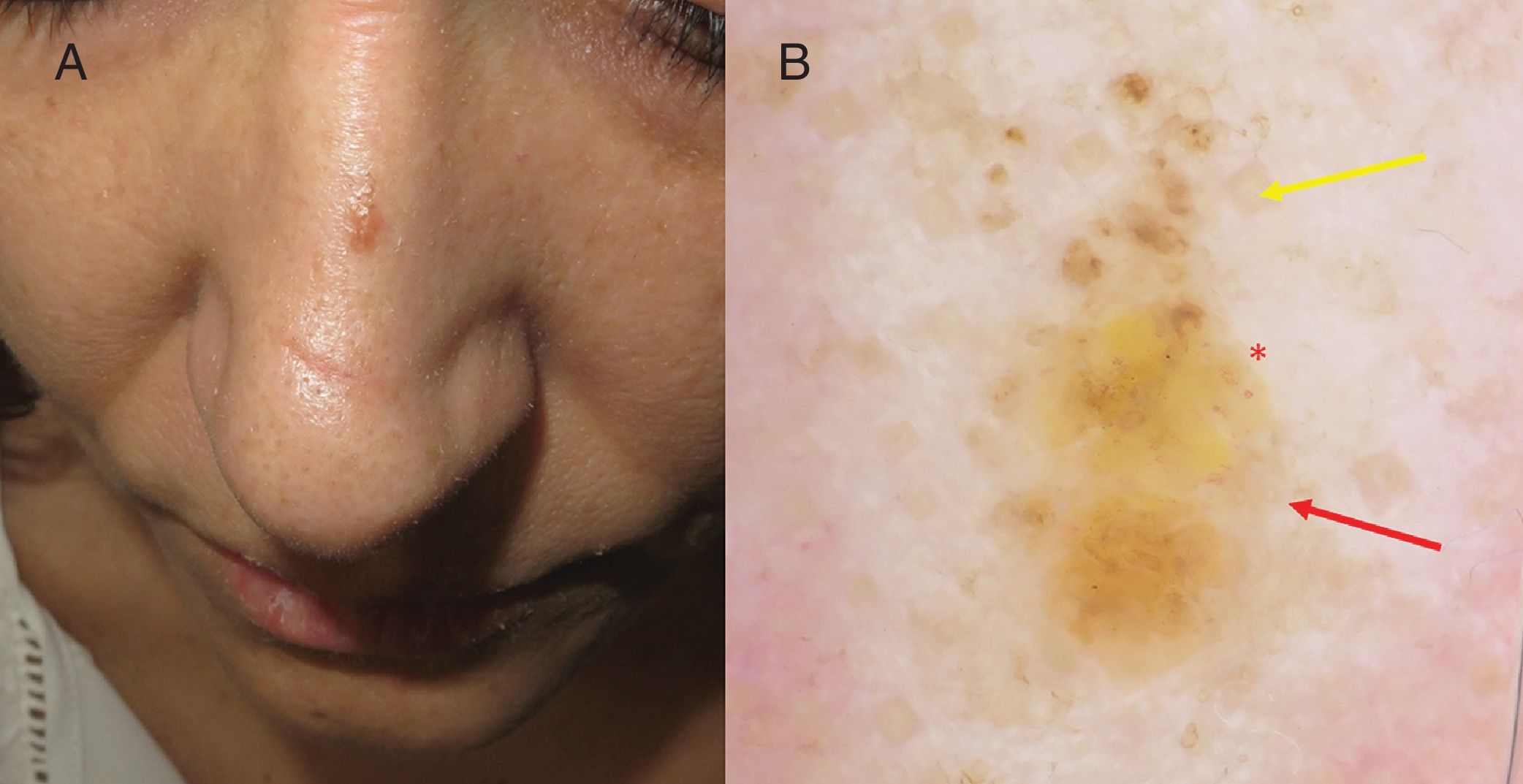
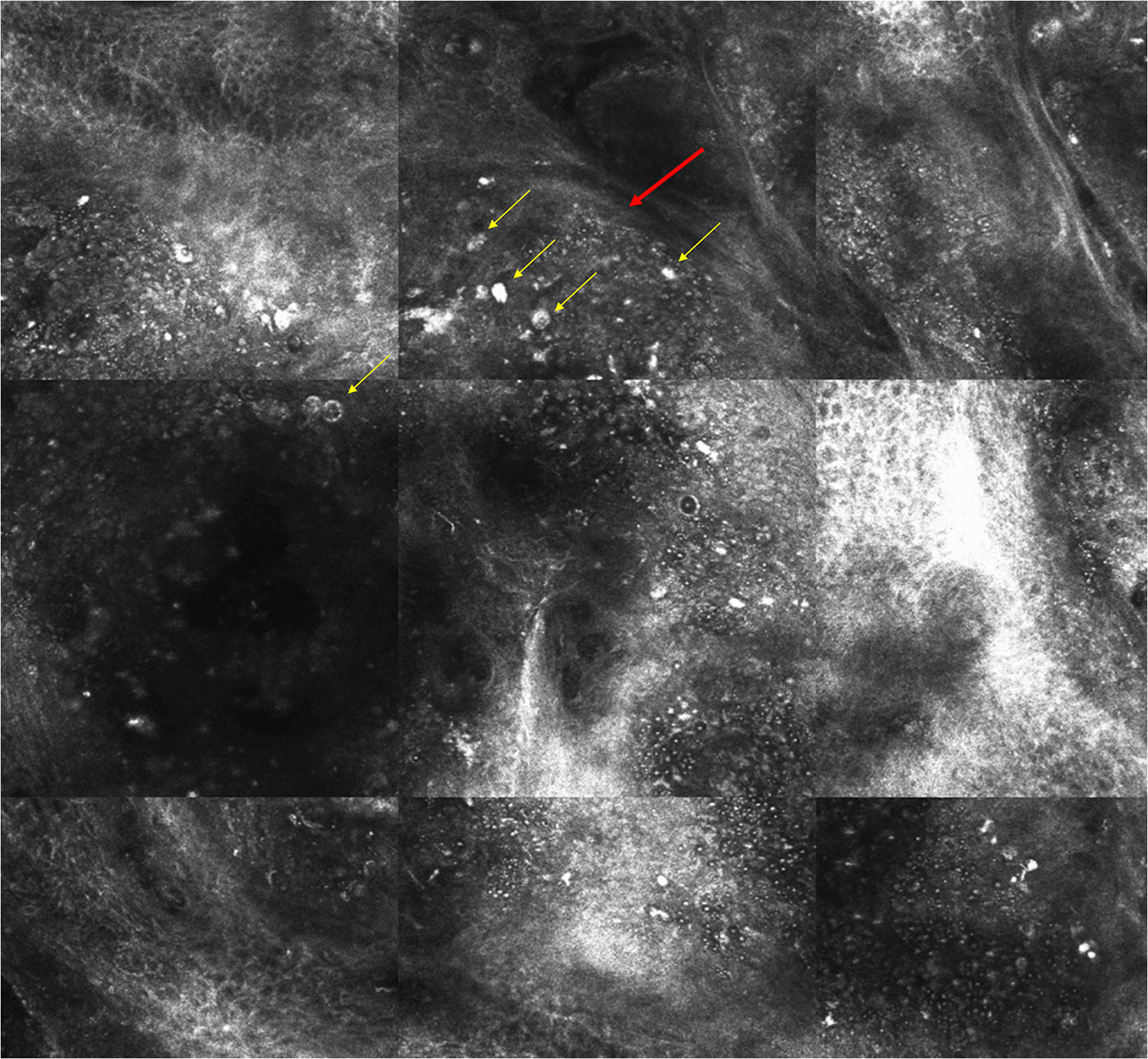
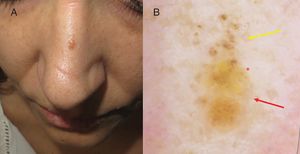
Case 1The patient was a 48-year-old woman with hypothyroidism who was seen for a slow-growing lesion on the nasal dorsum that had appeared several years earlier. Dermoscopic examination of the 4-mm, skin-colored papule revealed brown globules predominating in the upper half, yellowish unstructured areas in the lower half, and regular linear vessels (Fig. 1). RCM revealed the presence of ovoid cells with a dark, round, central nucleus and abundant bright granular cytoplasm with very well-defined borders, features typical of sebocytes. There were few very large, bright speckled cells (mature sebocytes) and a predominance of less reflective cells with less abundant cytoplasm (immature sebocytes) that were aggregated within nodules. RCM also revealed circular hyporeflective spaces (ducts with sebaceous differentiation), rounded, hyperreflective structures surrounded by a dark halo (corneal cysts), and abundant bright, cotton-like cells with no visible nucleus, irregular morphology, and poorly-defined borders that were gathered in small groups (macrophages). A diagnosis of sebaceoma was proposed based on the RCM findings, and was confirmed by histology (Fig. 2).
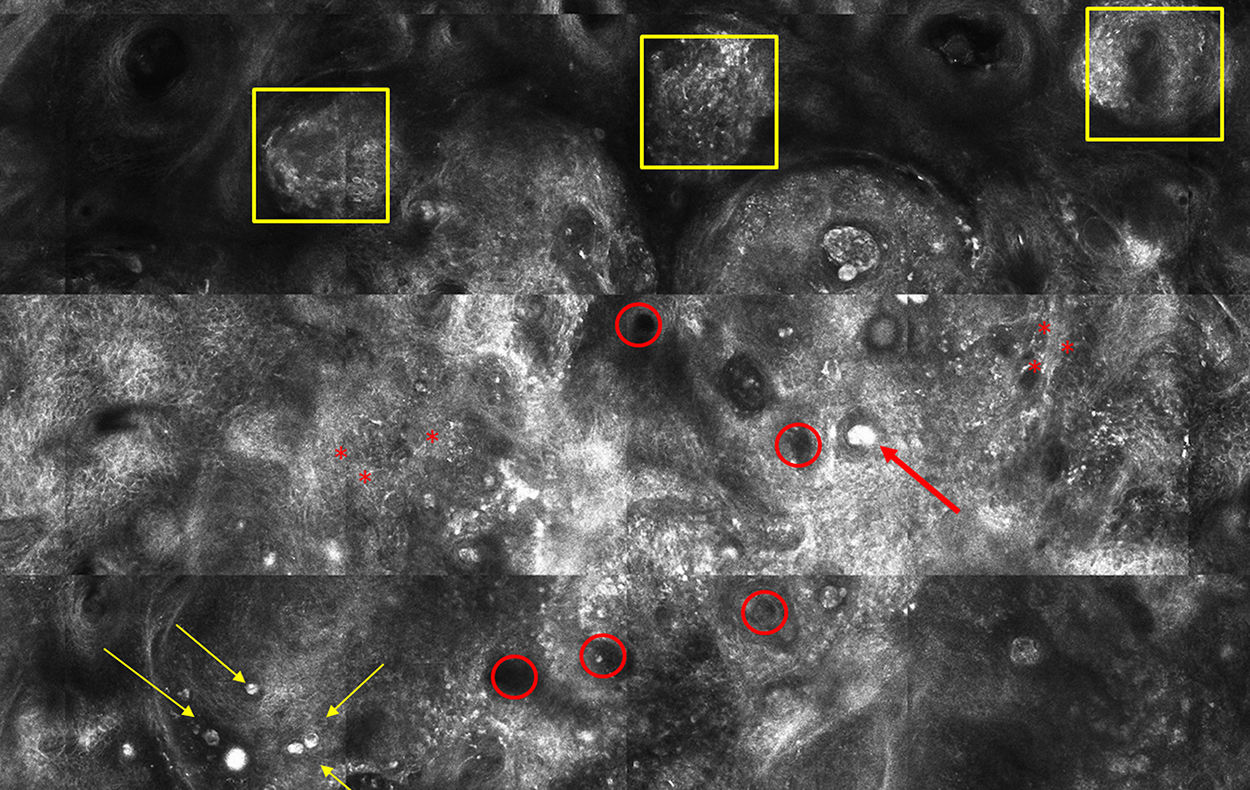
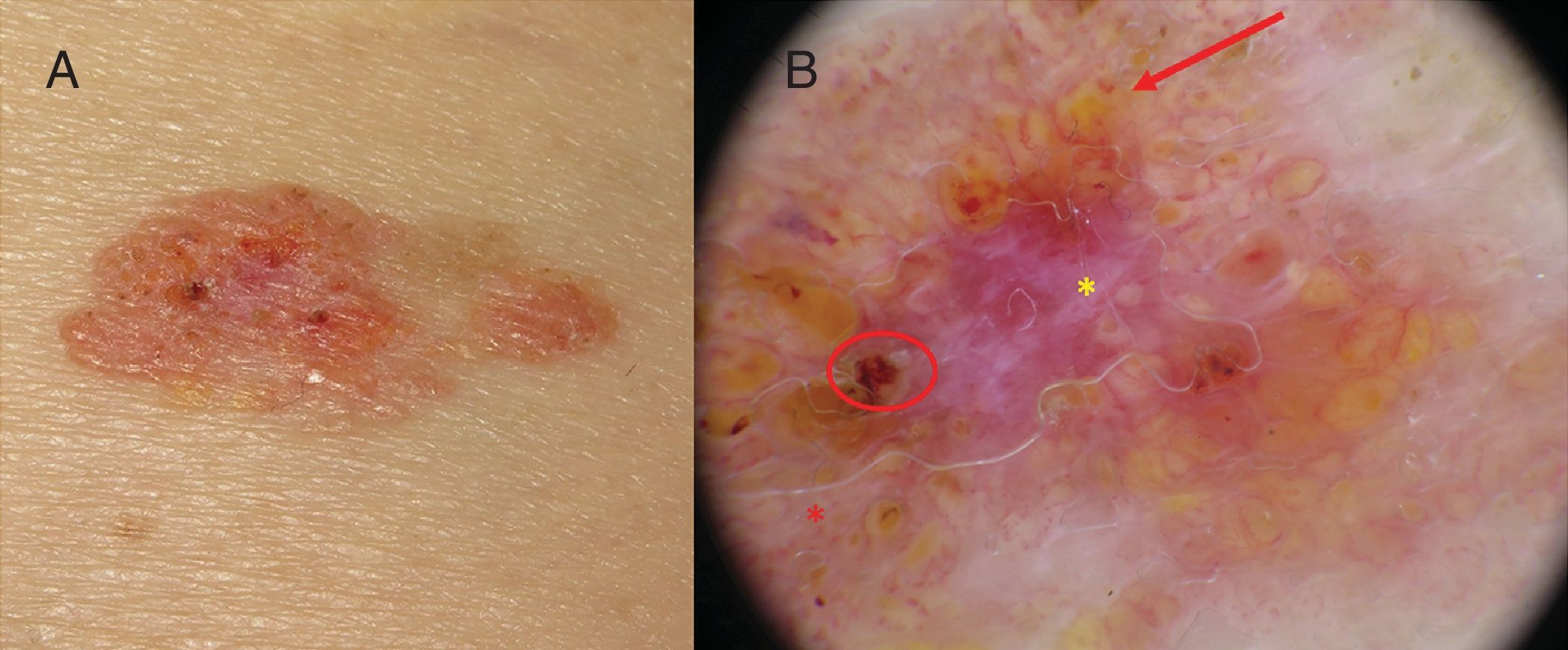
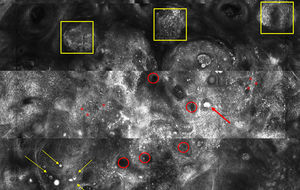
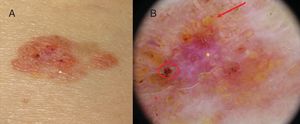
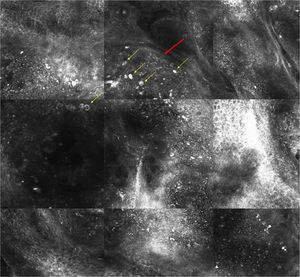
The patient was an 81-year-old woman with dyslipidemia and no past history of interest. She was seen for a lesion on the abdomen that had appeared 1 year earlier. The lesion was an orange, erythematous plaque of 2.5 × 1.5 cm with well-defined borders. Dermoscopy revealed an erythematous-white background with abundant yellowish globular structures, erosions, and branched vessels (Fig. 3). RCM revealed many ovoid cells containing abundant cytoplasm filled with hyperreflective granules (mature sebocytes) that were separated by narrow, dark, intercellular spaces and formed nodules delimited by a thin wall of cells with less abundant cytoplasm and lower reflectance (immature sebocytes) (Fig. 4). Sebaceous ducts were also evident. A diagnosis of sebaceoma was proposed based on the RCM findings, and was confirmed by histology.
The term sebomatricoma was proposed by Sánchez Yus and coworkers2 to describe a spectrum of benign sebaceous neoplasms of varying degrees of maturation. Sebaceous adenoma and sebaceoma lie at either extreme of this spectrum, and are characterized by higher and lower percentages of mature cells, respectively.
Clinically, sebomatricoma usually presents as solitary yellowish papules or plaques (except in cases of Muir-Torre syndrome), predominantly affecting the cephalic pole. There is little information in the literature on the corresponding dermoscopic features, although a recent study described 2 main clinico-dermoscopic patterns for sebaceous adenoma3: nodules or papules with a central crater and elongated crown vessels arranged around an unstructured, whitish-yellow area that may be covered with blood crusts; and nodules or papules without a central crater (as in our patient), with a yellowish-white background, yellowish globular structures, and branching, arborizing vessels. The authors reported no other distinguishing features of sebaceoma. However, these characteristics are shared by several lesions, complicating differential diagnosis. For example, sebaceous hyperplasia and molluscum contagiosum typically feature yellowish globular structures with crown vessels; basal cell epithelioma characteristically contains branched vessels, albeit more focused than those of sebaceous adenoma; and spinocellular carcinoma, especially keratoacanthoma, can exhibit a central keratin crater with radial vessels.
Therefore, even when clinical and dermoscopic characteristics suggest a diagnosis of sebomatricoma, confirmation by histology has up to now been considered essential. However, RCM, which offers cellular resolution comparable to that of conventional histology, has made noninvasive diagnosis possible. There is little information in the literature on the RCM features of sebomatricoma. Thanks to the excellent correlation between RCM and histological findings in sebomatricoma, this technique enables assessment of the degree of cell maturation, and therefore allows in vivo diagnosis of sebomatricoma and characterization of sebomatricoma subtype, as illustrated in the 2 cases reported here. RCM of sebaceoma (in which immature sebocytes predominate) reveals nests of small, basaloid cells with isolated, bright, large mature sebocytes, in addition to ducts with sebaceous differentiation. By contrast, RCM of sebaceous adenoma reveals lobes of large, rounded or cuboid cells with hyperreflective cytoplasmic granules and a dark central nucleus, delimited by a thin wall of basaloid cells.4
Sebaceous adenoma and sebaceoma are benign lesions. However, Muir-Torre syndrome, which was ruled out in both our cases, must be ruled out to establish diagnosis. Considered a phenotypic variant of Lynch syndrome, Muir-Torre syndrome follows an autosomal dominant pattern of inheritance and is characterized by tumors of the sebaceous gland that are associated with early malignant visceral neoplasms (mainly affecting the digestive system), which may appear before or after the cutaneous neoplasms.5 Given its important clinical implications, accurate diagnosis of sebomatricoma is essential. To this end, RCM constitutes a noninvasive alternative to histology.
The authors thank the patients for providing written consent to the publication of the images included in this letter.
Please cite this article as: Burillo-Martínez S, Gamo R, Pinedo F, López-Estebaranz JL. Utilidad de la microscopía confocal de reflectancia para el diagnóstico in vivo de los sebomatricomas. Actas Dermosifiliogr. 2019;110:176–179.