Secondary syphilis is known as the great imposter because of its many mucocutaneous presentations. While oral lesions occur in up to 30% of patients, mucosal involvement only is rare. Oral lesions include plaques, macules and papules, nodules, and ulcers.1
We report a case of secondary syphilis with mucosal involvement only.
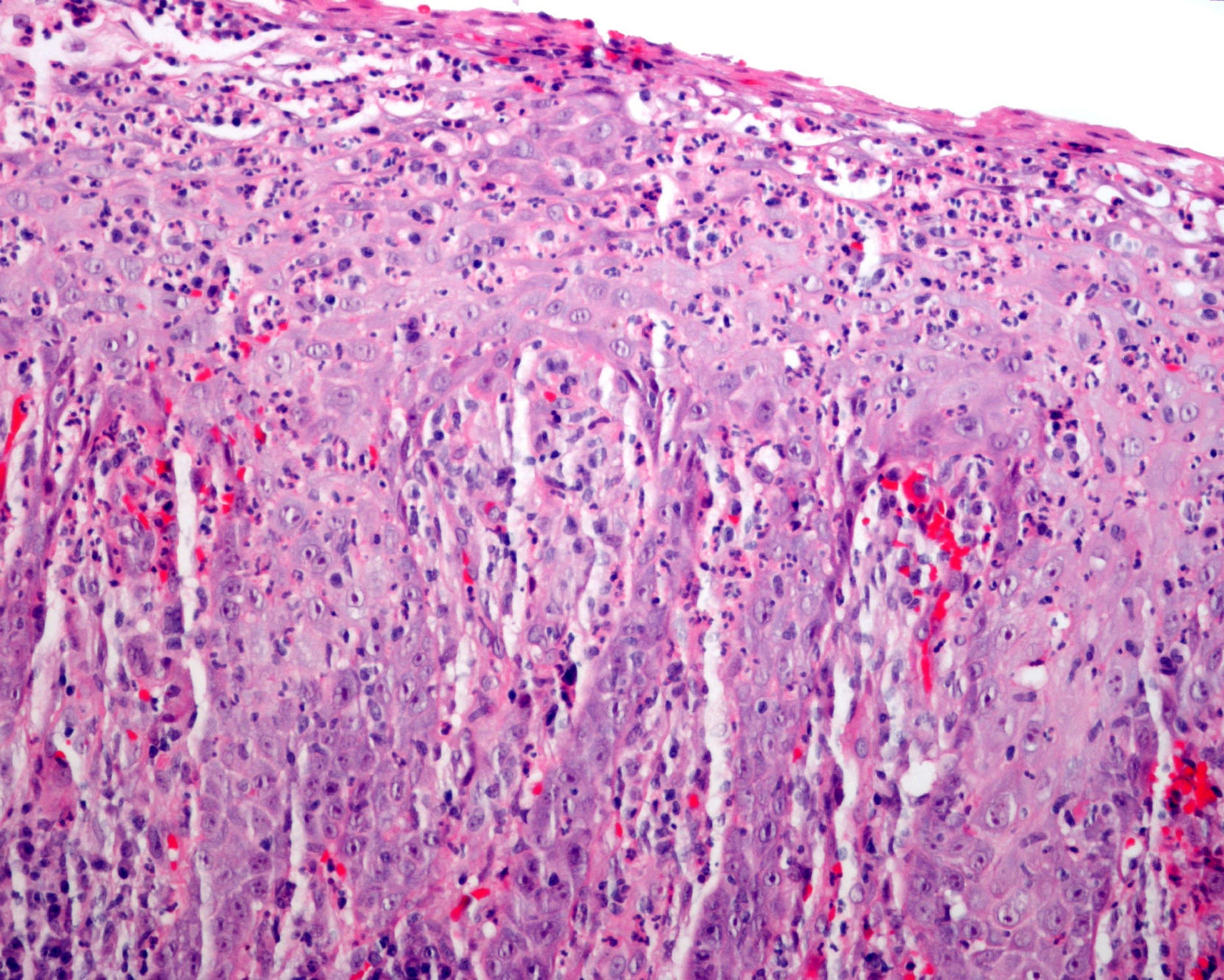
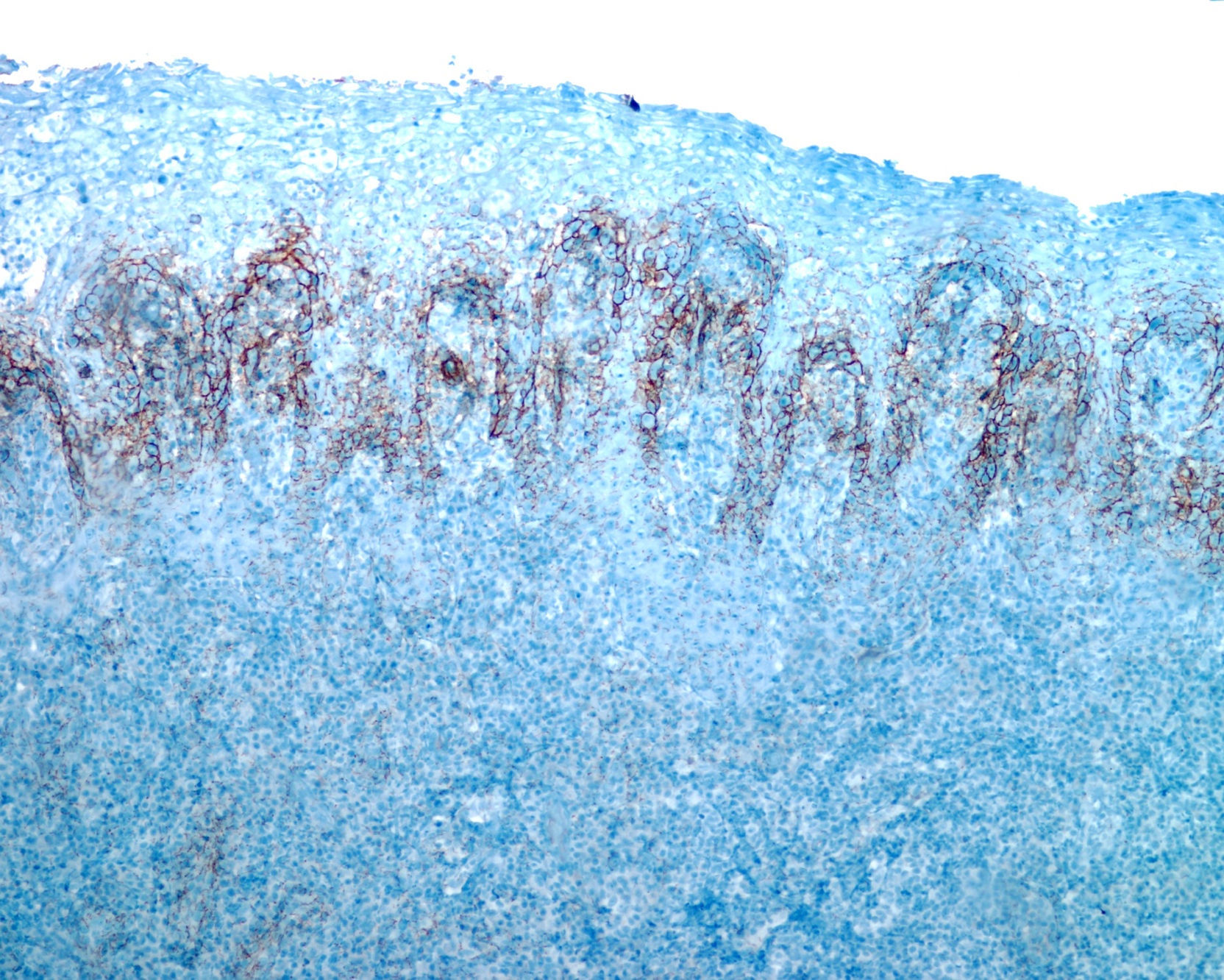
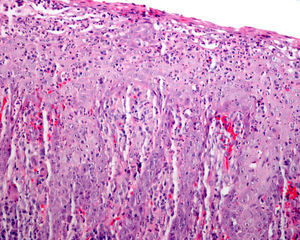
The patient was a 34-year-old man with human immunodeficiency virus (HIV) infection under treatment with antiretrovirals who presented with asymptomatic whitish plaques on the fauces. The lesions had grown slowly in size over 8 months and there was no bleeding. Of note, 2 years earlier, coinciding with the diagnosis of HIV infection, the patient was also diagnosed with latent syphilis (VDRL titer of 1:16) by the infectious diseases department. He was prescribed doxycycline 100mg for 14 days because of a possible allergy to penicillin. At the time, the physical examination revealed an irregular whitish plaque on the soft palate, the left tonsil, and the uvula that could not be removed by scraping (Fig. 1). There were no other lesions of interest. Considering the history of recurrent tonsillitis and the lack of response to antibiotics, a biopsy of the palatine tonsils was performed in the ear, nose, and throat department; the results suggested candidiasis and treatment was started with antifungals, but there was no improvement in the lesions. Two months later, a biopsy of the soft palate performed in the maxillofacial surgery department revealed a marked neutrophilic exudate with signs of epithelial regeneration and a slight inflammatory infiltrate (Fig. 2). Cultures of respiratory secretions were repeatedly negative for bacteria and fungi. Given the persistence of the lesions, the patient was referred to the dermatology department. Based on the patient's history and the clinical suspicion of secondary syphilis, the above biopsy samples were submitted for immunohistochemical analysis with polyclonal Treponema pallidum antibody (Biocare Medical). The results showed abundant spirochetes located predominantly in the epithelium and to a lesser extent in the underlying chorion (Fig. 3) The treponemal tests were positive, with a VDRL titer of 1:4. The lesions resolved completely after a dose of 2.4 million units of penicillin benzathine. The patient received an additional 2 doses of intramuscular penicillin at weekly intervals, and 4 months later, was completely free of lesions.
HIV infection and immunodepression can alter the typical course of syphilis. Asymptomatic primary syphilis, for instance, is more common in patients with HIV infection, meaning that secondary manifestations are detected more frequently.2
The differential diagnosis should include stomatitis, erythema multiforme, pemphigus, lichen, squamous cell carcinoma, candidiasis, oral gonococcal infection, and oral hairy leukoplakia.3 Oral secondary syphilis frequently presents a diagnostic challenge. The presence of oral saprophytic spirochetes limits the diagnostic utility of dark field microscopy. Histopathology frequently shows a nonspecific, predominantly plasmocytic infiltrate with epidermal hyperplasia. Warthin-Starry staining reveals spirochetes in up to a third of cases. Immunohistochemical staining of biopsy samples is currently considered to be a rather useful test for patients with false positive or negative serology results. The technique has a specificity of almost 100% and a sensitivity of 90%, rates that are higher even than those described for polymerase chain reaction analysis of tissue samples.4 Apart from its high sensitivity and specificity, immunohistochemical staining can also be used to distinguish primary syphilis from secondary syphilis based on the location of the treponemes. While primary syphilis shows a mixed epitheliotropic and vasculotropic pattern, secondary syphilis shows an exclusively epitheliotropic pattern.5,6
We have presented the case of an immunodepressed patient who was referred to our department after several months of study with a whitish oral plaque that had been present for months. The plaque cleared within a week of administration of penicillin following confirmation of the suspected clinical diagnosis of secondary syphilis by immunohistochemistry. While syphilis reinfection cannot be ruled out, it is possible that doxycycline was ineffective because it is not a first-line drug or perhaps because the patient adhered poorly to the treatment. In patients allergic to penicillin, we recommend penicillin as the treatment of choice after prior desensitization. Dermatologists have an important role in the diagnosis of secondary syphilis, as many patients develop atypical lesions as an early manifestation.7
To conclude, diagnosis of secondary syphilis, the great imposter, continues to present challenges due to its multiple clinical manifestations. Immunohistochemical analysis of biopsy specimens may be a useful diagnostic tool in oral secondary syphilis with clinically and histologically atypical lesions and with negative serology for syphilis.
Please cite this article as: Solano-López G, de Argila D, Fraga J, García-Diez A. Placa blanquecina en el paladar blando. Actas Dermosifiliogr. 2013;104:834–835.