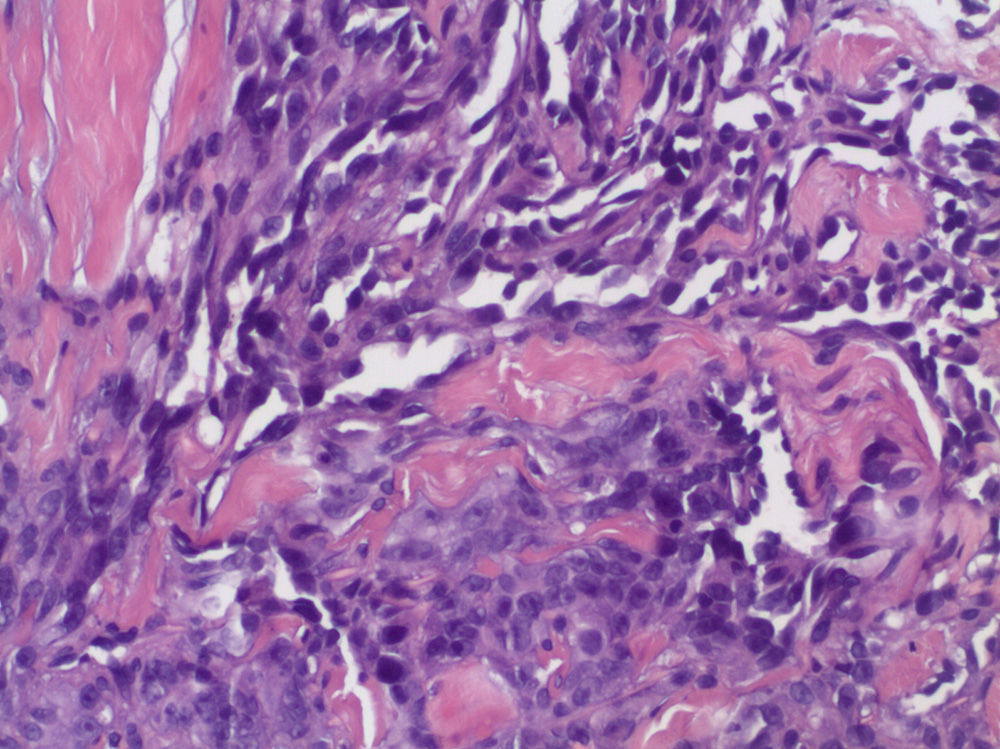
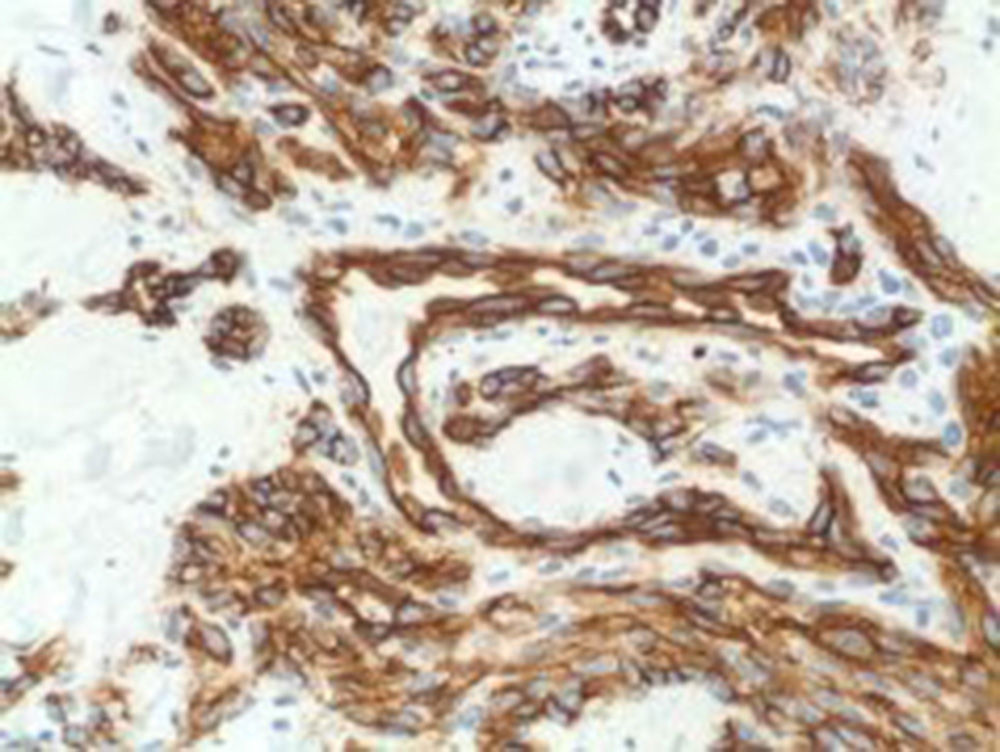
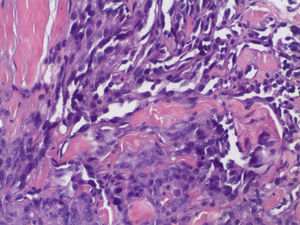
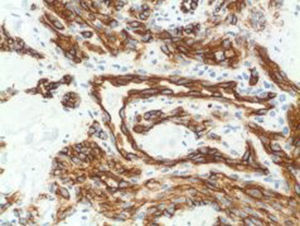
An 80-year-old woman with a history of hypertension and type 2 diabetes mellitus had been under treatment with ciclosporin (75mg/d) and mycophenolate (1500mg/d) since a 2004 kidney transplant for chronic renal failure. An infiltrating ductal carcinoma led to left mastectomy and axillary clearance in 2006 without adjuvant chemotherapy or radiotherapy. She was referred to the dermatologist for a lesion that had appeared on her abdomen 2 months earlier. The only symptom was a pulling sensation. The lesion formed a large reddish-purple bruise-like plaque covering almost the entire lower half of the abdomen. Nodular structures were also present (Fig. 1). No signs of adenopathy, ascites, or other cutaneous lesions were found. Histology revealed neoplastic endothelial cells forming channels that dissected collagen fibers. The cells exhibited atypia with loss of nuclear-cytoplasmic ratio, pleomorphism, and abundant mitoses (Fig. 2). Immunohistochemistry was positive for CD31 (Fig. 3) and CD34 markers in tumor cells and negative for human herpes virus 8. A diagnosis of angiosarcoma was established. A computed tomography scan of the abdomen revealed dermal tumors infiltrating the subcutaneous tissue as far as the abdominal wall below the umbilicus and mild ascites possibly related to peritoneal carcinomatosis. The patient was referred to the oncology department, where she declined the recommended chemotherapy. One month after diagnosis, she was admitted. Her general condition had declined, she had edema in the lower extremities and evident ascites. Paracentesis confirmed peritoneal infiltration of ascitic fluid secondary to the angiosarcoma. She died 2 weeks later from kidney failure.
Angiosarcoma, or malignant angioendothelioma, is an uncommon tumor of endothelial cells that accounts for only 2% of all sarcomas.1 It is an aggressive tumor with a 5-year survival rate of 50% to 60%.1 Mean survival after diagnosis ranges from 18 to 28 months.2 Three types of angiosarcoma are traditionally described. The first is idiopathic cutaneous angiosarcoma, which appears on the head and scalp of older patients.3 The second and third are angiosarcoma secondary to chronic lymphedema (Stewart-Treves syndrome) and a type that appears in skin exposed to radiotherapy. This tumor generally presents as a lesion that resembles bruising, with erythematous-violaceous nodules. The various types of angiosarcoma have similar histologic features. They are poorly defined tumors that trace irregular paths across large networks of dilated vascular channels, infiltrating dermal and subcutaneous layers. Tumor cells have large, hyperchromatic, pleomorphic nuclei and show a high degree of mitotic activity. CD31 positivity is the most sensitive immunohistochemical finding for establishing a diagnosis. Factor VIII and CD34 are secondary markers.4 The pathogenesis of these tumors is not clearly defined. Some have suggested that elevated serum concentrations of vascular endothelial growth factor or angiopoietin 2, or a decrease in cadherins in the vascular endothelium, may play a role.5 c-Myc amplification has also been detected in angiosarcomas secondary to radiotherapy or lymphedema.6,7 The role of drug-induced immunosuppression in the development of these tumors is unclear. Treatment requires surgical excision and radiotherapy. No evidence yet suggests that chemotherapy improves the prognosis, but chemotherapy with anthracyclines and taxanes would be the first line of treatment when the disease has metastasized. Twenty cases of angiosarcoma have been described to date in kidney transplant recipients on immunosuppressants. The tumor usually appears in an arteriovenous fistula. Only 5 other cutaneous angiosarcomas have been reported.3,8–10 The case we describe is highly unusual, similar only to one reported in 2011, in which an abdominal angiosarcoma appeared 8 years after a kidney transplant in an immunosuppressed patient.9 Our patient's tumor did not follow the traditional etiological pattern for this type of tumor. Although she had had a mastectomy, she had never undergone radiotherapy. Moreover, lymphedema was absent from the tumor site. The etiology of angiosarcomas in kidney transplanted patients on long-standing immunosuppressant therapy remains unclear, given the few known cases described. Impaired immune vigilance seems to be implicated, but further study is needed to establish the precise relationship between immunosuppression, kidney transplantation, and this rare tumor.
Please cite this article as: Martín P, Pulpillo A, Cabrera R, Conejo-Mir J. Angiosarcoma de pared abdominal en paciente con inmunosupresión farmacológica por trasplante renal. Actas Dermosifiliogr. 2016;107:162–163.