Dermatoses account for up to 30% of occupational diseases. Of these, 90% correspond to contact dermatitis, a disease associated with a marked economic burden and considerably impaired quality of life. In 1989, Toby Mathias proposed 7 criteria to assess the relationship between contact dermatitis and occupation.
ObjectiveTo assess the Mathias criteria for establishing occupational causation of contact dermatitis in patients with dermatoses.
Materials and methodsThis was a descriptive study of 103 patients with dermatoses, attended consecutively between January and March of 2009 in the immunology and skin allergy department of the Parc de Salut Mar, Barcelona, Spain. The diagnosis of an occupational cause of the skin complaint by a specialist after interviewing the patient was correlated with diagnosis according to the Mathias criteria, applied by an independent specialist. Descriptive and inferential statistics were calculated.
ResultsAn occupational cause was identified in 13 patients according to the Matthias criteria and in 12 according to the judgment of the dermatologist. The sensitivity for the Mathias criteria was 100% and the specificity was 98.90%, with a positive predictive value of 92.31% and a negative predictive value of 100%. The prevalence of occupational contact dermatitis was 11.65%.
ConclusionsThe Mathias criteria show a high validity and diagnostic yield, making them useful for establishing occupational causation of contact dermatitis. We believe that application of these criteria would help improve diagnostic and prognostic accuracy in occupational contact dermatitis.
Las dermatosis representan un 30% de las enfermedades profesionales. De ellas, el 90% corresponden a eczema de contacto repercutiendo ostensiblemente en la economía y la calidad de vida del paciente. En 1989 Toby Mathias propuso 7 criterios para la evaluación del vínculo entre el eczema de contacto y una profesión dada.
ObjetivoEvaluar la utilidad de los criterios de imputabilidad de enfermedad profesional definidos por Mathias en pacientes afectos de dermatosis cutánea.
MétodosEstudio descriptivo de 103 pacientes afectos de dermatosis cutáneas consecutivamente visitados desde enero a marzo del año 2009 en la Unidad de Inmunología y Alergia cutánea del Servicio de Dermatología del Parc de Salut Mar de Barcelona, correlacionando los criterios de imputabilidad laboral de la patología cutánea mediante valoración del especialista y mediante entrevista personalizada, incluyendo los criterios de Mathias por facultativo independiente. Valoración estadística descriptiva e inferencial.
ResultadosTrece pacientes mostraban implicación laboral, según la aplicación de los criterios de Mathias, y 12 pacientes mostraban relevancia laboral según criterio del especialista en Dermatología. La sensibilidad de los criterios de Mathias fue de un 100%, la especificidad fue de un 98,90%, el valor predictivo positivo de un 92,31% y el valor predictivo negativo de un 100%, con una prevalencia del 11,65%.
ConclusionesLos criterios de Mathias muestran una elevada validez y rendimiento, siendo útiles para el diagnóstico de eczema de contacto de origen laboral. Pensamos que su aplicación contribuiría en la precisión diagnóstica y pronóstica de las dermatitis de contacto profesionales.
Occupational dermatitis is a skin disorder caused or aggravated by conditions at the workplace. An example is contact dermatitis, an inflammatory, eczematous skin reaction caused by direct contact with or environmental exposure to a substance, which may be a low-molecular weight compound or a protein.1 It is a pruritic condition that is often of multifactorial origin. Contact dermatitis initially manifests as intensely pruritic, erythematous lesions, immediately followed by vesicles, exudation, crusting, and lichenification caused by scratching. The condition is classified as acute or chronic depending on the predominant type of lesions. There are 2 types of contact dermatitis: irritant and allergic. Irritant contact dermatitis (ICD) is much more common than its allergic counterpart (80% vs 20%). Allergic contact dermatitis (ACD) is a delayed type IV hypersensitivity reaction, unlike ICD, which develops following exposure to sufficient concentrations of an irritant substance.1–3 It has been reported that 20% of the general population are at risk of developing contact dermatitis at some point in their lives.4
Occupational contact dermatitis, which is well characterized both clinically and pathologically, can be caused or aggravated by working conditions. According to data published in 2004, skin disorders account for up to 30% of all occupational diseases in industrialized countries5 and contact dermatitis accounts for 90% of these skin disorders.6
It is difficult to compare data between countries because of differences in practices in the reporting of occupational disease. Furthermore, the incidence of occupational contact dermatitis is underestimated and records tend to be incomplete.3
Occupational skin disorders have a considerable socioeconomic impact. Contact dermatitis occurring at the workplace, for example, is a frequent cause of work-related disability and can account for up to 30% of workers’ compensation costs in many countries.3 The impact of occupational skin disorders on the lives of patients and their families has not yet been studied in depth.5,7
It is difficult to establish a causal link between contact dermatitis and a specific occupation or activity at the workplace without the use of objective criteria. In 1989, Toby Mathias1 proposed 7 such criteria to assess the link between contact dermatitis and occupation. None of the criteria in isolation provides sufficient evidence of a causal link,6 but the fulfillment of 4 of the 7 criteria is considered indicative of probable causation.1
In Spain, no studies have validated the usefulness of the Mathias criteria. Our aim was to assess the value of these criteria for establishing probable occupational causation of contact dermatitis.
ObjectiveThe aim of this study was to assess the usefulness of the Mathias criteria to establish occupational causation of skin disorders.
Material and MethodsStudy DesignWe performed a descriptive study to assess the usefulness of the Mathias criteria to establish occupational causation of skin disorders.
Study ParticipantsWe enrolled 103 adult patients who consecutively presented for skin patch testing at the dermatology department at Parc de Salut Mar in Barcelona, Spain between January 26 and March 30, 2009. No exclusion criteria were applied as we were interested in analyzing patients consulting for dermatitis, regardless of whether or not their condition was work-related.
Demographic, clinical, and diagnostic information was collected for each patient using the electronic unified medical record form within the Spanish version of the WinAlldat documentation system (European Surveillance System for Contact Allergy). The use of a structured medical record enabled the creation of a uniform database.
Consent was obtained from each patient and all the data were analyzed anonymously to ensure confidentiality.
Study VariablesPatients were analyzed by sex, age, occupation, preliminary diagnosis, site of lesions, allergy tests conducted, patch test results, final diagnosis, and occupational or nonoccupational relevance according to a dermatology specialist and based on the application of the Mathias criteria.
Patients were divided into those aged 35 years or less and those aged over 35 years. Occupations were coded using the Spanish National Classification of Occupations. The preliminary diagnosis was classified simply as an eczematous or a noneczematous skin condition. ACD was investigated by skin patch testing with the standard Spanish series and additional series where appropriate. In accordance with the recommendations of the International Contact Dermatitis Research Group and the European Society of Contact Dermatitis, only reactions that were positive (+, ++, or +++) at day 4 were considered to be positive. Lesion location was classified according to 6 sites: head, trunk, extremities, hands, flexural surfaces, and other sites. The definitive diagnoses were classified as ICD, ACD, atopic dermatitis, urticaria, or other conditions. The relevance of positive patch test results was assessed by a dermatology expert and classified as occupational (past or present), nonoccupational (past or present), or unknown. A separate analysis was performed to assess probable occupational causation using the Mathias criteria.
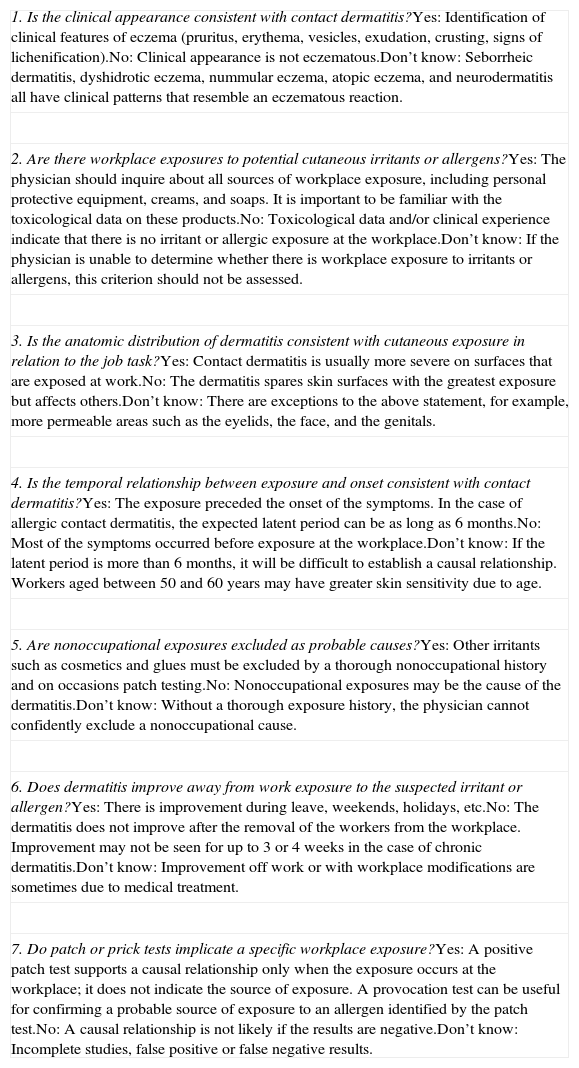
The Mathias CriteriaThe Mathias criteria are 7 objective criteria designed to establish probable occupational causation of contact dermatitis (Table 1).1 Four of the 7 criteria must be met to establish a probable causal link.1,5
The Mathias Criteria1.
| 1. Is the clinical appearance consistent with contact dermatitis?Yes: Identification of clinical features of eczema (pruritus, erythema, vesicles, exudation, crusting, signs of lichenification).No: Clinical appearance is not eczematous.Don’t know: Seborrheic dermatitis, dyshidrotic eczema, nummular eczema, atopic eczema, and neurodermatitis all have clinical patterns that resemble an eczematous reaction. |
| 2. Are there workplace exposures to potential cutaneous irritants or allergens?Yes: The physician should inquire about all sources of workplace exposure, including personal protective equipment, creams, and soaps. It is important to be familiar with the toxicological data on these products.No: Toxicological data and/or clinical experience indicate that there is no irritant or allergic exposure at the workplace.Don’t know: If the physician is unable to determine whether there is workplace exposure to irritants or allergens, this criterion should not be assessed. |
| 3. Is the anatomic distribution of dermatitis consistent with cutaneous exposure in relation to the job task?Yes: Contact dermatitis is usually more severe on surfaces that are exposed at work.No: The dermatitis spares skin surfaces with the greatest exposure but affects others.Don’t know: There are exceptions to the above statement, for example, more permeable areas such as the eyelids, the face, and the genitals. |
| 4. Is the temporal relationship between exposure and onset consistent with contact dermatitis?Yes: The exposure preceded the onset of the symptoms. In the case of allergic contact dermatitis, the expected latent period can be as long as 6 months.No: Most of the symptoms occurred before exposure at the workplace.Don’t know: If the latent period is more than 6 months, it will be difficult to establish a causal relationship. Workers aged between 50 and 60 years may have greater skin sensitivity due to age. |
| 5. Are nonoccupational exposures excluded as probable causes?Yes: Other irritants such as cosmetics and glues must be excluded by a thorough nonoccupational history and on occasions patch testing.No: Nonoccupational exposures may be the cause of the dermatitis.Don’t know: Without a thorough exposure history, the physician cannot confidently exclude a nonoccupational cause. |
| 6. Does dermatitis improve away from work exposure to the suspected irritant or allergen?Yes: There is improvement during leave, weekends, holidays, etc.No: The dermatitis does not improve after the removal of the workers from the workplace. Improvement may not be seen for up to 3 or 4 weeks in the case of chronic dermatitis.Don’t know: Improvement off work or with workplace modifications are sometimes due to medical treatment. |
| 7. Do patch or prick tests implicate a specific workplace exposure?Yes: A positive patch test supports a causal relationship only when the exposure occurs at the workplace; it does not indicate the source of exposure. A provocation test can be useful for confirming a probable source of exposure to an allergen identified by the patch test.No: A causal relationship is not likely if the results are negative.Don’t know: Incomplete studies, false positive or false negative results. |
In our series, we established a diagnosis of contact dermatitis and determined probable occupational causation by analyzing the answers to the Mathias questionnaire, the patients’ clinical history, and the skin patch test results.
Two independent physicians assessed occupational relevance on a case-by-case basis. One of these, a dermatology specialist, assessed the work-relatedness of each patient's skin condition on the basis of clinical manifestations, patch test results, a visit to the patient's workplace, and clinical experience. The other physician, working independently, applied the Mathias criteria in a personal interview with each patient to investigate the probability of a causal relationship between the patient's condition and employment. Both the patients and the interviewing physician were blind to the conclusions reached by the dermatology expert, and all the studies were conducted in the same week.
Once this phase was complete, the results of the dermatology expert and the physician who applied the Mathias criteria were correlated.
Statistical AnalysisTo analyze the validity and usefulness of the Mathias criteria as a diagnostic tool in occupational contact dermatitis, we established contact dermatitis as the dependent variable and occupational causation according to the Mathias criteria as the independent variable. All analyses were performed using the statistical software programs SPSS and EPIDAT.
The diagnosis made by the dermatology expert was considered the gold standard diagnosis.
We calculated sensitivity, specificity, positive predictive value, negative predictive value for a confidence level of 95% and frequencies of each of the variables analyzed, also for a confidence level of 95%.
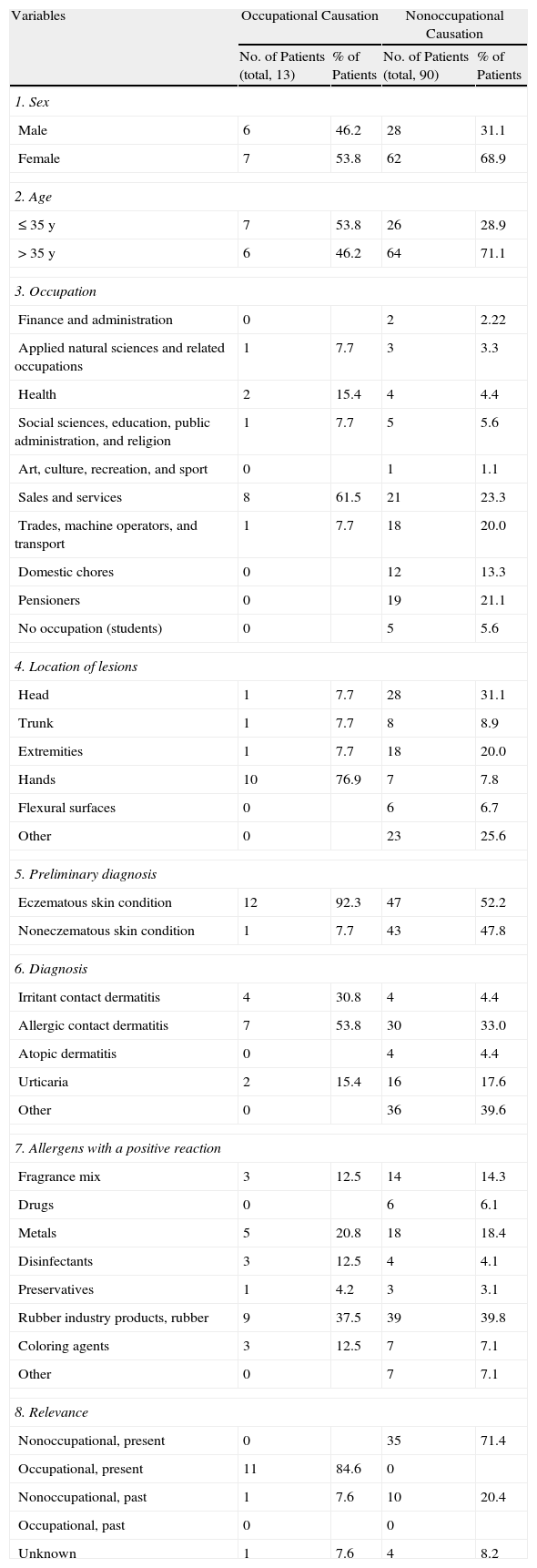
ResultsThe characteristics of the patients based on the information collected during the Mathias criteria interview are shown in Table 2.
Characteristics of Patients With and Without Probable Occupational Causation (n=103).
| Variables | Occupational Causation | Nonoccupational Causation | ||
| No. of Patients (total, 13) | % of Patients | No. of Patients (total, 90) | % of Patients | |
| 1. Sex | ||||
| Male | 6 | 46.2 | 28 | 31.1 |
| Female | 7 | 53.8 | 62 | 68.9 |
| 2. Age | ||||
| ≤35 y | 7 | 53.8 | 26 | 28.9 |
| >35 y | 6 | 46.2 | 64 | 71.1 |
| 3. Occupation | ||||
| Finance and administration | 0 | 2 | 2.22 | |
| Applied natural sciences and related occupations | 1 | 7.7 | 3 | 3.3 |
| Health | 2 | 15.4 | 4 | 4.4 |
| Social sciences, education, public administration, and religion | 1 | 7.7 | 5 | 5.6 |
| Art, culture, recreation, and sport | 0 | 1 | 1.1 | |
| Sales and services | 8 | 61.5 | 21 | 23.3 |
| Trades, machine operators, and transport | 1 | 7.7 | 18 | 20.0 |
| Domestic chores | 0 | 12 | 13.3 | |
| Pensioners | 0 | 19 | 21.1 | |
| No occupation (students) | 0 | 5 | 5.6 | |
| 4. Location of lesions | ||||
| Head | 1 | 7.7 | 28 | 31.1 |
| Trunk | 1 | 7.7 | 8 | 8.9 |
| Extremities | 1 | 7.7 | 18 | 20.0 |
| Hands | 10 | 76.9 | 7 | 7.8 |
| Flexural surfaces | 0 | 6 | 6.7 | |
| Other | 0 | 23 | 25.6 | |
| 5. Preliminary diagnosis | ||||
| Eczematous skin condition | 12 | 92.3 | 47 | 52.2 |
| Noneczematous skin condition | 1 | 7.7 | 43 | 47.8 |
| 6. Diagnosis | ||||
| Irritant contact dermatitis | 4 | 30.8 | 4 | 4.4 |
| Allergic contact dermatitis | 7 | 53.8 | 30 | 33.0 |
| Atopic dermatitis | 0 | 4 | 4.4 | |
| Urticaria | 2 | 15.4 | 16 | 17.6 |
| Other | 0 | 36 | 39.6 | |
| 7. Allergens with a positive reaction | ||||
| Fragrance mix | 3 | 12.5 | 14 | 14.3 |
| Drugs | 0 | 6 | 6.1 | |
| Metals | 5 | 20.8 | 18 | 18.4 |
| Disinfectants | 3 | 12.5 | 4 | 4.1 |
| Preservatives | 1 | 4.2 | 3 | 3.1 |
| Rubber industry products, rubber | 9 | 37.5 | 39 | 39.8 |
| Coloring agents | 3 | 12.5 | 7 | 7.1 |
| Other | 0 | 7 | 7.1 | |
| 8. Relevance | ||||
| Nonoccupational, present | 0 | 35 | 71.4 | |
| Occupational, present | 11 | 84.6 | 0 | |
| Nonoccupational, past | 1 | 7.6 | 10 | 20.4 |
| Occupational, past | 0 | 0 | ||
| Unknown | 1 | 7.6 | 4 | 8.2 |
After analyzing the results of the interview, we divided the 103 patients into 2 groups: those with a nonoccupational skin disorder (n=90) and those with an occupational skin disorder (n=13). A number of differences were observed between the groups depending on the variable analyzed: a) age: 53.8% of patients with an occupational skin disorder were 35 years old or younger, compared to 28.9% of those with a nonoccupational skin disorder; b) occupation: 61.5% of the patients with an occupational skin disorder worked in the sales and services sector, and 40% of those with a nonoccupational skin disorder did not have paid employment; c) location of skin lesions: 76.9% of patients with an occupational skin disorder had lesions, compared to only 9% of those with a nonoccupational skin disorder (this was one of main differences observed); d) diagnosis: the main diagnosis in the occupational skin disorder group was ACD (53.8%), while in the other group it was other skin disorders (39.6%).
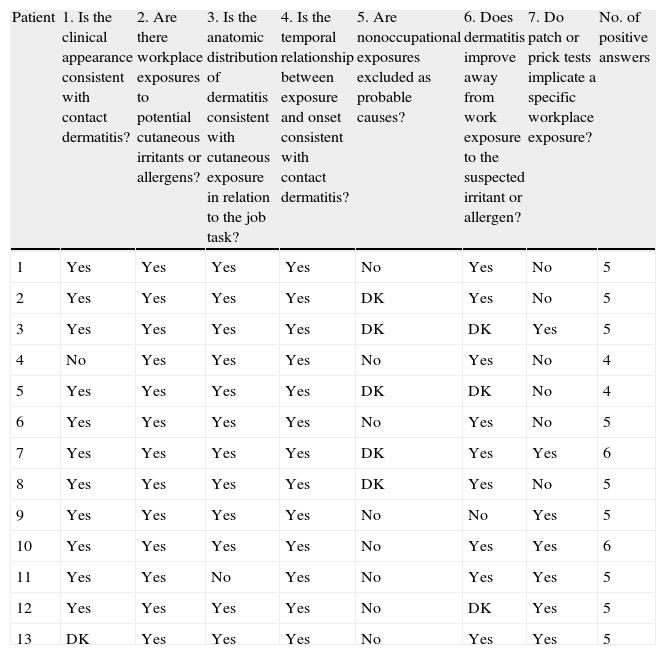
Of the 103 patients analyzed, 13 met 4 or more of the Mathias criteria (Table 3), indicating a probable occupational causation.
Results of Mathias Criteria Questionnaire.
| Patient | 1. Is the clinical appearance consistent with contact dermatitis? | 2. Are there workplace exposures to potential cutaneous irritants or allergens? | 3. Is the anatomic distribution of dermatitis consistent with cutaneous exposure in relation to the job task? | 4. Is the temporal relationship between exposure and onset consistent with contact dermatitis? | 5. Are nonoccupational exposures excluded as probable causes? | 6. Does dermatitis improve away from work exposure to the suspected irritant or allergen? | 7. Do patch or prick tests implicate a specific workplace exposure? | No. of positive answers |
| 1 | Yes | Yes | Yes | Yes | No | Yes | No | 5 |
| 2 | Yes | Yes | Yes | Yes | DK | Yes | No | 5 |
| 3 | Yes | Yes | Yes | Yes | DK | DK | Yes | 5 |
| 4 | No | Yes | Yes | Yes | No | Yes | No | 4 |
| 5 | Yes | Yes | Yes | Yes | DK | DK | No | 4 |
| 6 | Yes | Yes | Yes | Yes | No | Yes | No | 5 |
| 7 | Yes | Yes | Yes | Yes | DK | Yes | Yes | 6 |
| 8 | Yes | Yes | Yes | Yes | DK | Yes | No | 5 |
| 9 | Yes | Yes | Yes | Yes | No | No | Yes | 5 |
| 10 | Yes | Yes | Yes | Yes | No | Yes | Yes | 6 |
| 11 | Yes | Yes | No | Yes | No | Yes | Yes | 5 |
| 12 | Yes | Yes | Yes | Yes | No | DK | Yes | 5 |
| 13 | DK | Yes | Yes | Yes | No | Yes | Yes | 5 |
Abbreviation: DK, don’t know.
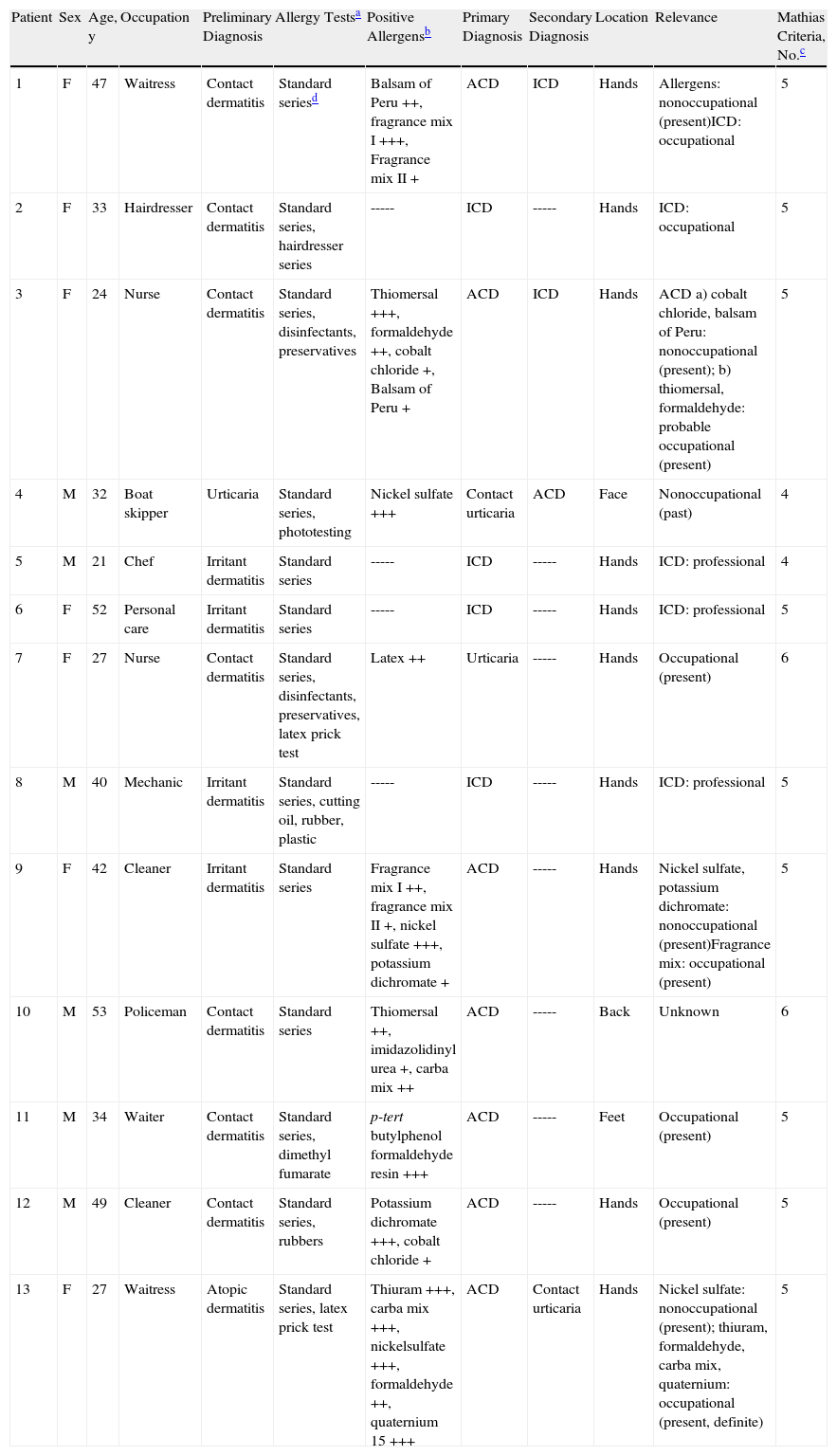
Seven of the 12 patients with an occupational skin disorder according to the Mathias criteria had a primary diagnosis of ACD, and in 5 of these the positive allergy test results were considered to be of present occupational relevance (Table 4). Patient #11, a waiter with a primary diagnosis of ACD with foot involvement, wore shoes at work that caused contact dermatitis on his feet. Patient #10 had a presumed diagnosis of ACD with involvement of the back, but the positive patch test results were classified as being of unknown relevance. The patient was a policeman, who attributed his condition to a new heat-resistant shirt he wore at work. This could not be demonstrated, however, as a patch test performed with material from the shirt was negative; nonetheless, the shirt produced an irritant dermatitis on the patient's back. It cannot, therefore, be ruled out that the initial symptoms assumedly caused by the heat-resistant shirt were responsible for the patient's dermatitis. Five patients were diagnosed with ICD. One of these (patient #1) had a primary diagnosis of ACD and a secondary diagnosis of ICD, but only ICD was classified as having occupational relevance (negative patch tests). In patient #7, who had a primary diagnosis of urticaria, occupational relevance was established on the basis of the patient's clinical and occupational history, a history of contact dermatitis of the hands, and allergy test results.
Patients With Occupational Causation: Demographic Characteristics, Occupation, and Occupational Relevance Based on the Application of the Mathias Criteria and the Judgment of a Dermatology Specialist.
| Patient | Sex | Age, y | Occupation | Preliminary Diagnosis | Allergy Testsa | Positive Allergensb | Primary Diagnosis | Secondary Diagnosis | Location | Relevance | Mathias Criteria, No.c |
| 1 | F | 47 | Waitress | Contact dermatitis | Standard seriesd | Balsam of Peru ++, fragrance mix I +++, Fragrance mix II + | ACD | ICD | Hands | Allergens: nonoccupational (present)ICD: occupational | 5 |
| 2 | F | 33 | Hairdresser | Contact dermatitis | Standard series, hairdresser series | ----- | ICD | ----- | Hands | ICD: occupational | 5 |
| 3 | F | 24 | Nurse | Contact dermatitis | Standard series, disinfectants, preservatives | Thiomersal +++, formaldehyde ++, cobalt chloride +, Balsam of Peru + | ACD | ICD | Hands | ACD a) cobalt chloride, balsam of Peru: nonoccupational (present); b) thiomersal, formaldehyde: probable occupational (present) | 5 |
| 4 | M | 32 | Boat skipper | Urticaria | Standard series, phototesting | Nickel sulfate +++ | Contact urticaria | ACD | Face | Nonoccupational (past) | 4 |
| 5 | M | 21 | Chef | Irritant dermatitis | Standard series | ----- | ICD | ----- | Hands | ICD: professional | 4 |
| 6 | F | 52 | Personal care | Irritant dermatitis | Standard series | ----- | ICD | ----- | Hands | ICD: professional | 5 |
| 7 | F | 27 | Nurse | Contact dermatitis | Standard series, disinfectants, preservatives, latex prick test | Latex ++ | Urticaria | ----- | Hands | Occupational (present) | 6 |
| 8 | M | 40 | Mechanic | Irritant dermatitis | Standard series, cutting oil, rubber, plastic | ----- | ICD | ----- | Hands | ICD: professional | 5 |
| 9 | F | 42 | Cleaner | Irritant dermatitis | Standard series | Fragrance mix I ++, fragrance mix II +, nickel sulfate +++, potassium dichromate + | ACD | ----- | Hands | Nickel sulfate, potassium dichromate: nonoccupational (present)Fragrance mix: occupational (present) | 5 |
| 10 | M | 53 | Policeman | Contact dermatitis | Standard series | Thiomersal ++, imidazolidinyl urea +, carba mix ++ | ACD | ----- | Back | Unknown | 6 |
| 11 | M | 34 | Waiter | Contact dermatitis | Standard series, dimethyl fumarate | p-tert butylphenol formaldehyde resin +++ | ACD | ----- | Feet | Occupational (present) | 5 |
| 12 | M | 49 | Cleaner | Contact dermatitis | Standard series, rubbers | Potassium dichromate +++, cobalt chloride + | ACD | ----- | Hands | Occupational (present) | 5 |
| 13 | F | 27 | Waitress | Atopic dermatitis | Standard series, latex prick test | Thiuram +++, carba mix +++, nickelsulfate +++, formaldehyde ++, quaternium 15 +++ | ACD | Contact urticaria | Hands | Nickel sulfate: nonoccupational (present); thiuram, formaldehyde, carba mix, quaternium: occupational (present, definite) | 5 |
Abbreviations: ACD, allergic contact dermatitis; ICD, irritant contact dermatitis.
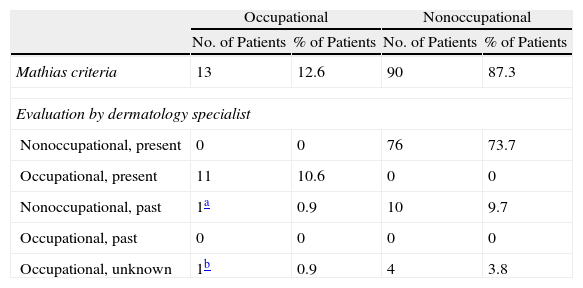
Twelve of the 13 patients who had a work-related skin disorder according to the Mathias criteria were also considered to have a skin disorder of present or past occupational relevance according to the dermatology specialist (Table 5). The present relevance was not the same for all the patients. For example, in 1 patient, the ICD but not the ACD was considered to be work-related and in another patient, there were 2 positive patch test results but only 1 of them was occupationally relevant. All the patients were analyzed on a case-by-case basis.
Correlation of Results Based on Application of Mathias Criteria and on the Judgment of a Dermatology Specialist.
| Occupational | Nonoccupational | |||
| No. of Patients | % of Patients | No. of Patients | % of Patients | |
| Mathias criteria | 13 | 12.6 | 90 | 87.3 |
| Evaluation by dermatology specialist | ||||
| Nonoccupational, present | 0 | 0 | 76 | 73.7 |
| Occupational, present | 11 | 10.6 | 0 | 0 |
| Nonoccupational, past | 1a | 0.9 | 10 | 9.7 |
| Occupational, past | 0 | 0 | 0 | 0 |
| Occupational, unknown | 1b | 0.9 | 4 | 3.8 |
Patient #4 (see Table 4) had urticaria, and the positive skin patch test was of past nonoccupational relevance.
In brief, probable occupational causation was established in 13 patients according to the Mathias criteria and in 12 according to the dermatology expert (Table 5).
One of the 13 patients (patient #4) had a false positive result as the positive patch test reaction was of past nonoccupational relevance. Nonetheless, the answers to the Mathias questionnaire indicated probable occupational causation. The patient was diagnosed with contact urticaria.
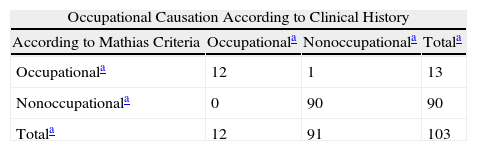
The Mathias criteria had a sensitivity of 100%, a specificity of 98.90%, a positive predictive power of 92.31%, and a negative predictive power of 100%; the prevalence of occupational contact dermatitis was 11.65% (Table 6). These results show that the Mathias criteria have a high validity and diagnostic yield in occupational contact dermatitis.
Validity of Mathias Criteria for Establishing Occupational Causation.
| Occupational Causation According to Clinical History | |||
| According to Mathias Criteria | Occupationala | Nonoccupationala | Totala |
| Occupationala | 12 | 1 | 13 |
| Nonoccupationala | 0 | 90 | 90 |
| Totala | 12 | 91 | 103 |
| Value | 95% CI | |
| Sensitivity, % | 100.00 | 95.83-100.00 |
| Specificity, % | 98.90 | 96.21-100.00 |
| Validity, % | 99.03 | 96.65-100.00 |
| Positive predictive value, % | 92.31 | 73.98-100.00 |
| Negative predictive value, % | 100.00 | 99.44-100.00 |
| Prevalence of contact dermatitis, % | 11.65 | 4.97-18.33 |
The validity of the Mathias criteria according to the different measures and variables analyzed was reduced by the false positive result for patient #4 (Table 6).
DiscussionOur findings show that the likelihood of establishing occupational causation in a patient with occupational contact dermatitis using the Mathias criteria was 100% (sensitivity, 100%), with a specificity of 98.9%, a positive predictive power of 92.31%, and a negative predictive power of 100%. These results confirm that the Mathias criteria have a highly validity and diagnostic yield in occupational contact dermatitis.
Of the 103 patients analyzed, a link between disease and employment was found in 13 patients according to the Mathias criteria and in 12 according to the judgment of the dermatology specialist. In other words, the application of the Mathias criteria yielded just 1 false positive result.
In a similar study to ours, Ingber and Merims6 concluded that the Mathias criteria were useful for assessing occupational causation and aggravation of contact dermatitis, but they had reservations about the first criterion. According to Mathias, all the criteria in the questionnaire should be analyzed, even if the answer to the first question is no. While Ingber and Merims agreed that a patient might have a work-related skin disease other than contact dermatitis (e.g., atopic dermatitis), they considered that it would be better to have a questionnaire where a negative answer to the first question meant that the rest of the questions did not have to be answered.
Similarly to Ingber and Merims,6 we found that the Mathias criteria were useful for establishing a causal link between occupation and skin disease.
Several aspects should be taken into consideration with regard to our findings: 1) the first question in the Mathias questionnaire (“Is the clinical appearance consistent with contact dermatitis?”) was answered using the information available during the patient interview, where not all patients had visible symptoms; 2) for the second question (“Are there workplace exposures to potential cutaneous irritants or allergens?”), it was considered that workplace exposure did not occur in students, homemakers, or pensioners; 3), question 5 (“Are nonoccupational exposures excluded as likely causes?”) was difficult to assess because it is impossible to exclude nonoccupational exposure as workers are in contact with suspect allergens both at and outside the workplace5; and finally 4) question 7 (“Do patch tests or provocation tests implicate a probable causal agent?”) had to be answered after the interview as it was necessary to review the patients’ clinical history to assess the allergy test results.
Patient #4 had a false positive result that influenced the overall sensitivity, specificity, and predictive values for the Mathias criteria. Based on the application of the criteria, there was a probable link between the patient's condition and his occupation, but the primary diagnosis according to the dermatology specialist was contact urticaria without occupational relevance. None of the Mathias criteria in isolation provides sufficient evidence to establish occupational causation of contact dermatitis.6 The questionnaire contains 7 criteria and likely causation is established on the basis of a positive answer to any 4 items. As Ingber and Merims reasoned,6 if the answer to the first question is no (as was the case with patient #4 in our series), there would be no reason to continue with the other 6 questions considering that a causal relationship between contact dermatitis and employment has been ruled out.5 In our study, we applied the Mathias criteria exactly as proposed by Mathias.1 Accordingly, all 7 criteria were tested, despite the negative answer to question 1 (the patient had urticaria and not dermatitis). The answers to the remaining 6 questions established the probability of a causal relationship between the patient's skin condition and employment (4 positive answers).
This study has several limitations: the time allocated to the study was short; a specialist was needed to answer question 7; and not all patients had symptoms during the interview, meaning that question 1 had to be answered on the basis of information gathered during the questioning of the patient. Not all patients have symptoms when seen in routine clinical practice, as many only see the specialist months after they have first consulted for their symptoms, and these patients will often have received several treatments. Nevertheless, a substantial number of patients with severe disease are seen and diagnosed when they have visible symptoms. A final limitation of our study is the possible presence of selection bias as our data are based on a hospital sample.
The study has numerous strengths: we studied a large number of patients, the dermatology department where the study was conducted has experience in occupational disease, and the Mathias criteria were applied without knowledge of the patient's clinical history.
Very few studies have investigated the causal link between contact dermatitis and employment, despite the obvious interests for patients, workers’ compensation agencies, and society as a whole. While the Mathias criteria were designed to establish the likelihood of occupational causation of contact dermatitis, they may also be useful for guiding referrals to specalists in occupational dermatology. Although more studies are necessary, our findings suggest that the Mathias criteria are useful for assessing occupational causation, although this does not obviate the need for additional, necessary measures such as a visit to the patient's workplace and an analysis of what his or her job entails.
ConclusionIn summary, we can conclude that the Mathias criteria are useful for establishing probable occupational causation of contact dermatitis. Finally, we believe that it is important to disseminate these criteria, because, as has been suggested by other authors, greater knowledge and application of these criteria may improve the diagnosis of occupational contact dermatitis.
Conflict of InterestsThe authors declare that they have no conflicts of interest.
Please cite this article as: Gómez de Carvallo M, et al. Evaluación de los criterios de imputabilidad de dermatosis profesinal definidos por Mathias. Actas Dermosifiliogr.2012;103:411-21.