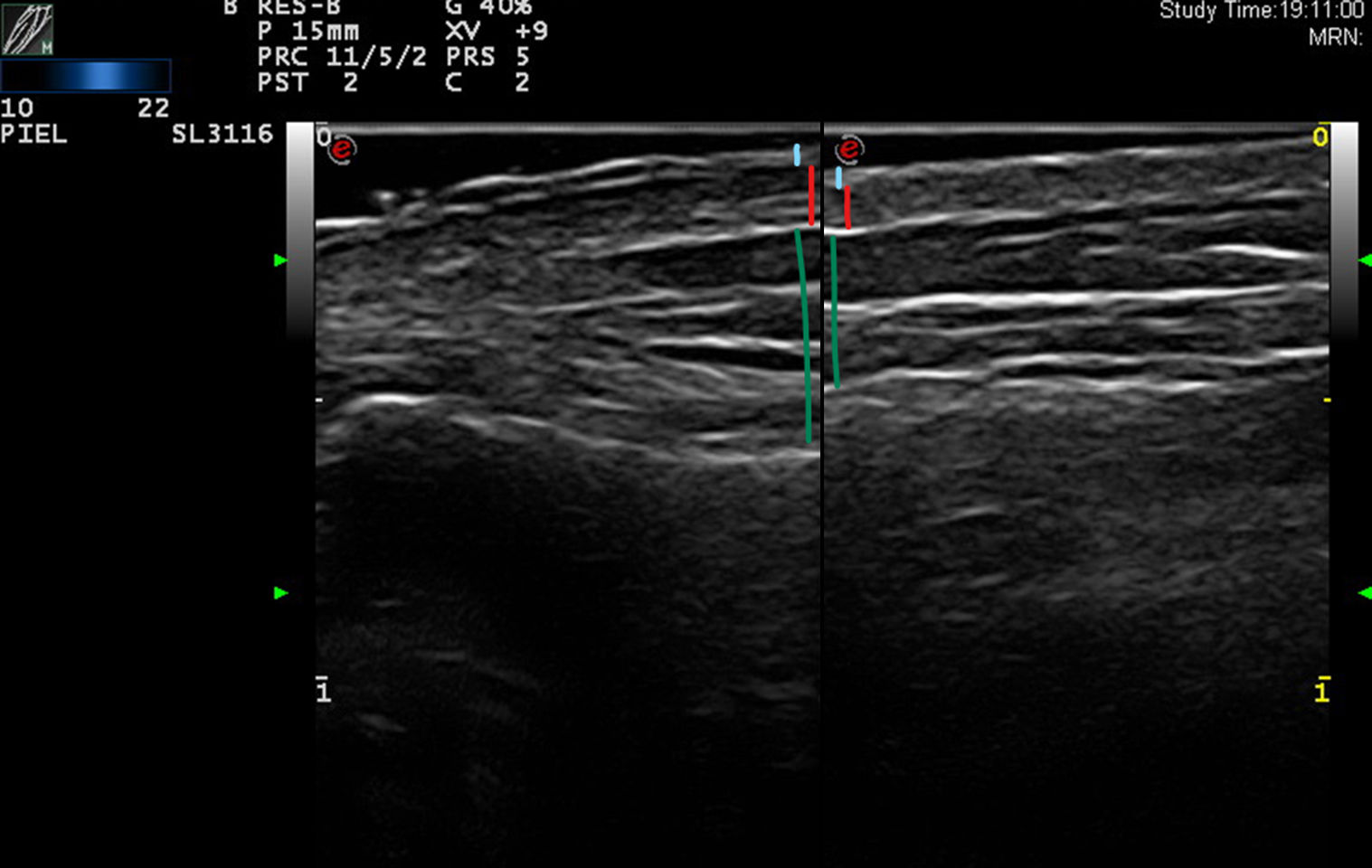
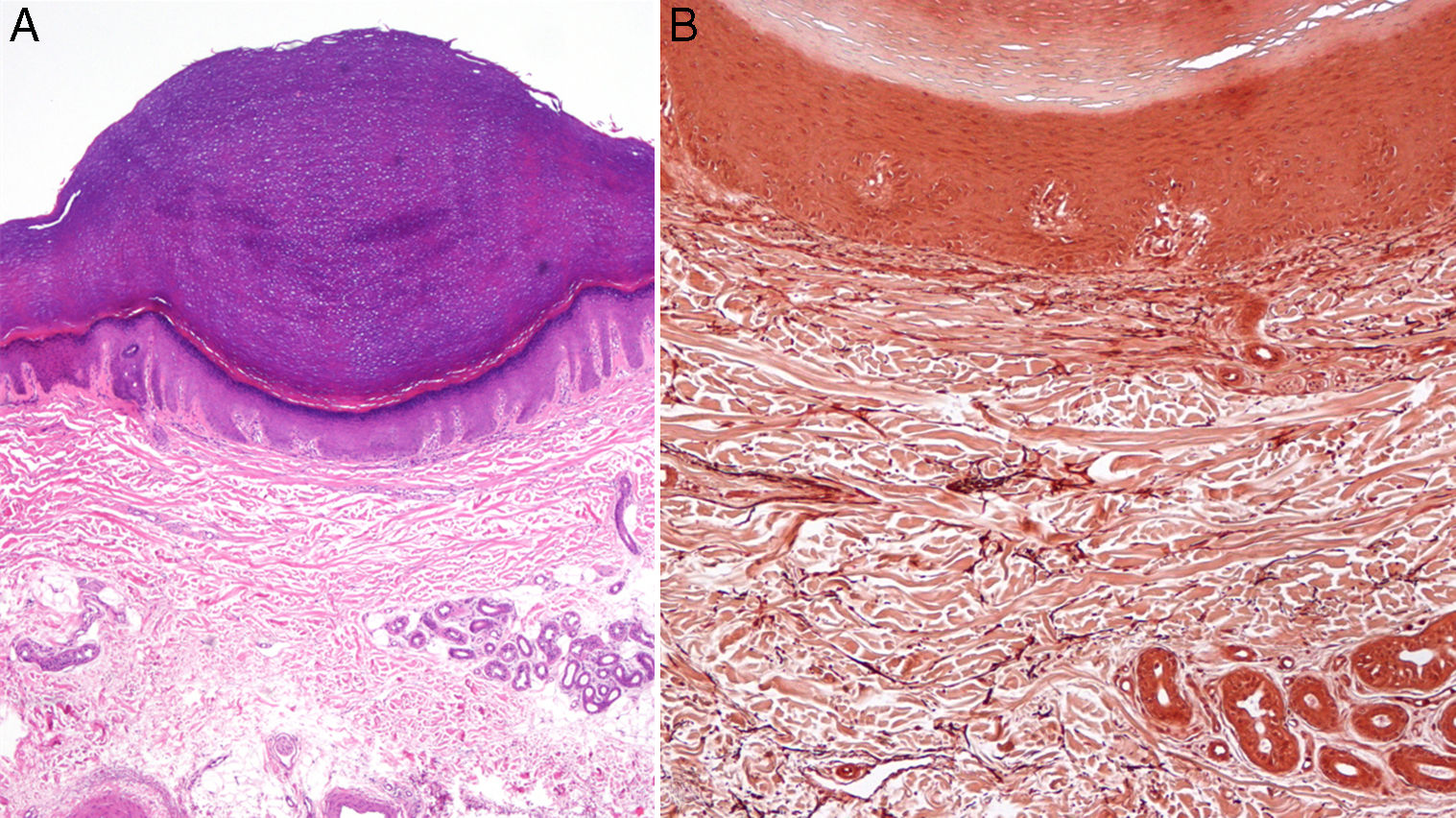
We report the case of a 38-year-old woman (skin type V) with a history of tricuspid and mitral regurgitation who had undergone pulmonary bilobectomy for atypical carcinoid tumor. She was taking oral contraceptives. She attended our center with a flare-up of pruriginous lesions on her hands and forearms that had first appeared 1 year previously. The lesions appeared every month and did not remit completely between flare-ups, although they did improve with medium-potency topical corticosteroids. She reported no lesions at other sites and denied having had concomitant symptoms. Physical examination revealed poorly defined, apparently residual erythematous-brownish macules on the anterior and lateral surfaces of the wrists. Multiple hyperpigmented papules with a shiny surface measuring between 1 mm and 3mm in diameter were observed on the radial surface of the first finger of both hands and on the palmar creases. These alternated with flesh-colored papules with a lichenoid appearance on the adjacent skin and were distributed symmetrically (Fig. 1). An ultrasound scan (Esaote, MyLabClass C with a 22-MHz transducer) of the affected area on the lateral surface of the wrist revealed epidermal thickening in the form of a cleft, which was observed as double hyperechoic band with a hypoechoic central area. The upper band was characterized by undulations that varied between more hyperechoic areas (convex) and more hypoechoic areas (concave) (Fig. 2). Ultrasound revealed a certain degree of hypoechogenicity in the dermis that was interpreted as an artifact resulting from epidermal thickening using the 22-MHz transducer. The suspicion of lichen nitidus compared with elastic fiber abnormality led us to perform a biopsy of the ultrasound lesion and to prescribe clobetasol cream. Histopathology revealed a compact area of orthokeratotic hyperkeratosis resting on a slight epidermal depression with mild hypergranulosis in the epidermis (Fig. 3). No inflammation or other significant histopathological abnormalities were observed. Orcein staining did not reveal elastorrhexis. Therefore, the findings were compatible with focal acral hyperkeratosis (FAH)–type marginal papular acrokeratoderma. At subsequent visits, the patient reported a lack of improvement with her daily high-potency corticosteroid and even mentioned the appearance of additional lesions; consequently, we recommended a switch to mometasone and calcipotriol cream.
Upper trace, epidermis; middle trace, dermis; lower trace, subcutaneous cellular tissue. Lesional skin (left): cleft in the epidermis seen as a double hyperechoic band with a hypoechoic central area on a somewhat hypoechoic dermis (possible artifact secondary to variability in epidermal thickening). Upper band: undulation that alternates between more hyperechoic areas (convex) and more hypoechoic areas (concave). Healthy skin (right): epidermis with no abnormalities in the form of a fine homogeneous hyperechoic band.
FAH is an uncommon variant of a heterogeneous group of conditions grouped together under the term palmoplantar keratoderma, which are characterized by chronic pathologic thickening of the hairless skin of the palms and soles secondary to hyperkeratosis. Until 1983, there had been multiple reports of hyperkeratotic papular lesions on the lateral sides of the hands and feet. Their clinical presentation was similar to that of a condition previously known as acrokeratoelastoidosis,1 and the histology findings were similar, except for the absence of elastorrhexis. This is when Dowd et al.2 coined the term focal acral hyperkeratosis to define a new entity whose differentiation with acrokeratoelastoidosis continues to be controversial. Those authors who see the conditions as separate entities believe that the first is a focal keratinization disorder, whereas the second is based on abnormalities of the elastic fibers. Their claims are supported by the histologic nuance of elastorrhexis.3 In 1994, Rongioletti et al.4 proposed grouping these 2entities and other clinically indistinguishable conditions under the term marginal papular acrokeratoderma. In 2009, Martínez-Casimiro et al.5 reported a new FAH-type case, similar to the one we report here. The patient was a black woman in the third decade of life with asymptomatic lesions on the palms and lateral surfaces of the hands that had first appeared several years previously. The authors studied the article by Dowd et al., who reported on familial cases (autosomal dominant inheritance pattern6). The typical histology pattern is invariably characterized by orthokeratotic hyperkeratosis on an epidermal depression, with no abnormalities of collagen or elastic fibers. Lee and Kim7 examined biopsy specimens of lesional and healthy skin and performed immunohistochemical staining of proliferation and differentiation markers (Ki-67/proliferating cell nuclear antigen and involucrin, respectively). In addition to a 3.4-fold increase in the thickness of the orthokeratotic layer and a 2-fold increase in the thickness of the epidermis, the authors reported increased levels for both markers, thus supporting the possibility that FAH is a focal disorder of keratinization in which the process is accelerated.
In addition to the histology findings, we reported the ultrasound characteristics of the condition, which involved a specific epidermal cleft with marked changes in echogenicity and no abnormalities in the dermis. No abnormalities of the healthy skin were observed (the marked difference in the thickness of the epidermis can be seen in Fig. 3). To date, diagnosis of FAH has been based on characteristic symptoms with consistent demographic data and a potentially compatible family history, as well as on the absence of dermal abnormalities in histology. The finding of the ultrasound characteristics used in the differential diagnosis8 of FAH (acrokeratoelastoidosis itself, plane warts, acrokeratosis verruciformis, punctate porokeratosis, punctate palmoplantar keratoderma, palmoplantar lichen planus, and juvenile elastoma) could be essential for determining the role of ultrasound in the differential diagnosis of these conditions. The main limitation is the low number of cases and, therefore, the difficulty in matching with similar clinical presentations in the various conditions that manifest as palmoplantar keratoderma. There is no evidence to support treating FAH, which often proves to be ineffective: given the absence of symptoms, not treating is a reasonable option.9
We report the first ultrasound description of FAH as an additional diagnostic tool in the study of palmoplantar keratoderma.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Company-Quiroga J, Echeverría B, Tardío JC, Martínez-Morán C. Hiperqueratosis acral focal: correlación clínica, histopatológica y ecográfica. Actas Dermosifiliogr. 2018;109:936–939.