In Panama, weekly case conferences are held in which all dermatologists from throughout the country agree on a second opinion for the diagnosis of complicated cases. Unfortunately, patients from the interior of the country may have difficulty attending these case conferences. An alternative in such situations is the use of telemedicine. To date, however, no studies have been undertaken on the effectiveness of this approach in Panama. The aim of this study was to assess the degree of correlation between the diagnoses obtained in case conferences involving face-to-face examination and those involving telemedicine.
Material and methodA quasi-experimental nonblinded analysis of correlation was carried out in which dermatologists were randomly assigned to 2 groups: face-to-face examination and telemedicine. Both groups were asked to assess 30 cases and the degree of correlation (Cohen κ coefficient) between the diagnoses made by each group was assessed.
ResultsThe patient group included 19 women (63.3%) and 9 patients (30%) were aged between 50 and 59 years. There was a good correlation (κ=0.6512) between the results of teledermatology and face-to-face examination. Significant differences in the diagnostic skills of the 2 groups were ruled out.
ConclusionsTeledermatology can be used effectively to facilitate diagnosis in case conferences involving patients who cannot attend in person (gold standard).
El Ateneo de Dermatología de Panamá es una reunión científico-docente semanal que agrupa a todos los dermatólogos del país para dar una segunda opinión consensuada a aquellos dermatólogos que consultan por casos complicados. Desafortunadamente el Ateneo está menos disponible para los pacientes del interior del país debido a diversas barreras de accesibilidad. En el Teleateneo de Dermatología se utiliza la telemedicina para atender a aquellos pacientes que no tienen la posibilidad de asistir a esta reunión. No existen estudios en Panamá que determinen la utilidad de esta variante del Ateneo. El objetivo de este estudio es determinar si existe correlación entre la capacidad diagnóstica de los dermatólogos del Teleateneo y la de los que examinaban a los pacientes en el Ateneo presencial.
Material y métodoEstudio analítico, correlacional, cuasi-experimental, aleatorizado y abierto. Los dermatólogos fueron divididos en dos grupos al azar: Ateneo presencial y Teleateneo. Se les expuso a 30 casos clínicos y se determinó el grado de correlación (kappa de Cohen) entre la capacidad diagnóstica de los dermatólogos de cada grupo.
ResultadosEl 63,33% de los pacientes era del sexo femenino y el 30% tenía 50-59 años. El grado de correlación fue bueno (к = 0,6512) entre el grupo de Teleateneo y el de Ateneo presencial. Se descartaron diferencias significativas de capacitación entre ambos grupos.
ConclusionesEl Teleateneo puede ser utilizado con seguridad como una herramienta de apoyo al diagnóstico del dermatólogo cuyo paciente no puede asistir a la sesión de Ateneo presencial (patrón oro).
All dermatologists in Panama attend weekly case conferences at Hospital Santo Tomás in Panama City to discuss the diagnosis and treatment of complicated cases. The patients are examined in person at these conferences.
Skin diseases are very common in the general population.1 In 2008, 352 patients attended the case conferences at Hospital Santo Tomás; 65.44% were from the metropolitan area of Panama City and San Miguelito and 34.56% were from the interior of the country. This distribution of patients is the opposite of the geographic distribution of the population (35.7% and 64.3%, respectively),2 possibly indicating that patients from more remote areas face significant geographic, economic, cultural, and other barriers that reduce the likelihood of them attending the case conferences in the capital.
Telemedicine is the practice of health care using information and communication technology (ICT).3 It offers numerous advantages, including improved accessibility to health care services for patients located in remote geographic regions. In addition to wider access, telemedicine also reduces costs and workloads in referral hospitals with specialist services located in cities, speeds up the referral process, shortens waiting times, improves patient quality of life, and increases user satisfaction. It is also of value in the provision of specialist emergency care to victims of disasters as well as a useful tool for continuing medical education and multicenter research.3–9
Considerable advances have been made in telemedicine since it was first introduced in Panama in 1998. Particular progress has been made in the area of radiology but telemedicine is not currently used in dermatology practice in Panama. Among the Latin American countries that are making the greatest efforts to promote the use of telemedicine are Colombia, Mexico, Venezuela, Chile, Peru, and Paraguay.10–17
Teledermatology is a subspecialty of telemedicine in which dermatologists use ICT to examine skin lesions and analyze laboratory results to offer a diagnosis and recommend treatment from a distance.4,18–22 The use of various technologies as part of teledermatology facilitates the provision of remote health care services and education programs.23–28 The most common approach used in teledermatology is the store-and-forward, or asynchronous, approach. Several studies have shown this to be of value as a screening tool in patients with pigmented lesions and in the routine management of patients referred to skin cancer and pigmented lesion clinics.29,30
Teledermatology could be used to evaluate patients from the interior of Panama at the weekly case conferences held at Hospital Santo Tomás. These patients would not have to travel to the city as they could be evaluated by the team of dermatologists from a distance. No studies to date, however, have analyzed whether remote diagnoses are as reliable as those made in face-to-face consultations by dermatologists in Panama. The aim of the present study was to analyze the level of diagnostic agreement between face-to-face consultation and teleconsultation by a team of dermatologists from Panama who meet weekly to discuss complicated cases. Our results provide scientific evidence supporting the use of teledermatology at these case conferences. These findings provide a basis for the introduction of teledermatology to improve the accessibility of health care services among patients in the poorer, more remote parts of the country, who, as citizens of Panama, deserve the same level of care as their compatriots from the capital.
Material and MethodsWe performed a quasi-experimental analysis of diagnostic agreement between face-to-face consultation and teleconsultation using an open, randomized design. The target group comprised 352 patients, which is the number of patients evaluated at the weekly conferences held by dermatologists in Panama in 2008. Due to the complexity and cost associated with analyzing this number of patients, we analyzed a representative group of 30 patients (minimum sample size). This is the approximate number of patients who would be seen in a month. We chose April 2009 for our study. Thirty patients who had been seen by a dermatologist at Complejo Hospitalario Dr. Arnulfo Arias Madrid (CHDAAM) were randomly selected. They all had a diagnosis confirmed by biopsy and skin lesions that were present in April 2009. Patients were excluded if they did not wish to participate in the study, if they did not sign the informed consent form, if they had been previously evaluated at a case conference, if they did not have a diagnosis confirmed by biopsy, or if their dermatologists did not want them to participate. They were also excluded if they did not turn up for their appointment, if they left the case conference before they had been evaluated by both groups of dermatologists, or if they revealed their diagnosis during evaluation.
In addition to the patients’ sex, age, and occupation, we analyzed the following variables:
- 1.
Diagnosis: disease recorded by the majority of dermatologists for each patient examined at the case conferences.
- 2.
Diagnosis confirmed by biopsy: disease mentioned in the histopathology report.
- 3.
Type of consultation: approach used by the dermatologists to evaluate the patients in their weekly scientific/educational meetings: face-to-face consultation or teleconsultation.
The selected patients were scheduled for a visit at CHDAAM, where the attending dermatologist prepared a written report for the face-to-face consultation and a slide presentation for the teleconsultation. These reports included the following information: patient's name, age, sex, general medical history, relevant history, physical findings, and diagnosis confirmed by biopsy. The slide presentation also included photographs of the patient taken with a digital camera (Olympus μ 1010, 10.1megapixels. 7× optical zoom). The reports were e-mailed to the dermatology resident at Hospital Santo Tomás who was responsible for presenting the cases to the dermatologists. Three sessions were held, with 10 patients evaluated per session. The dermatologists who attended the 3 sessions were randomly assigned to a face-to-face consultation group and a teleconsultation group. In the face-to-face consultation, each dermatologist was given a form containing the numbers 1 to 10 to note down the diagnosis for each patient. For each case, the dermatology resident read out the report prepared by CHDAAM and then invited the patient to come in to be examined. The dermatologists discussed the case and then all noted down the diagnosis they believed to be correct next to the corresponding number on their diagnosis forms. The teleconsultation session was held in another room, which was acoustically isolated from the room in which the face-to-face consultation was taking place. The dermatologists in the teleconsultation group were given 2 diagnosis forms: one containing the letters A to H to note down their diagnoses following the remote evaluation and another containing the numbers 1 to 10 to note down their diagnoses after they had seen the patient in person. The resident presented each case using the slide presentations sent by the dermatologists at CHDAAM. After each presentation, the dermatologists were given time to discuss the case and note down the diagnosis they considered to be correct (on the form containing the letters A-J). When this session was complete, the dermatologists analyzed the same cases, but in the presence of the patients. The procedure was the same as that described for the first group. The resident read out the report sent by the dermatologists from CHDAAM and invited the patient to come in for examination. After discussing the case, the dermatologists noted down the diagnosis they considered to be correct next to the corresponding number on the form containing the numbers 1 to 10.
The forms filled in by the dermatologists were used to record the diagnosis made by the majority of dermatologists for each patient. Data from the case and biopsy reports were also recorded. The information was entered into an electronic form containing the study variables and their respective categories created using the Epi Info software program (version 3.4.3). Data tables were created and used to calculate the percentage of diagnoses that coincided with the diagnosis confirmed by biopsy and to compare the number of correct diagnoses in the face-to-face consultation and the teleconsultation groups. The influence of interobserver variability was analyzed to confirm that any differences detected could be attributed to differences between the consultation methods and not between the observers. This was why the teleconsultation group also examined the patients in person in a second session. In theory, the percentage of correct diagnoses made by both groups of dermatologists in the face-to-face consultations should have been similar. The percent agreement between the 2 groups was calculated by adding the number of correct and incorrect diagnoses in each group, dividing the result by the number of cases studied, and multiplying this by 100. The level of diagnostic agreement between the 2 groups was also measured using the κ statistic, which was calculated using EpiData (version 3.1) and interpreted using the Landis and Koch scale.31
The study complied with the ethics guidelines of the Declaration of Helsinki and was approved by the bioethics committee and the scientific committee at CHDAAM, which is operated by the country's social security office (Caja de Seguro Social). It was also approved by the Vice Rector's Office for Research and Postgraduate Studies at the University of Panama. All of the patients agreed to participate in the study and appropriate measures were taken to guarantee their confidentiality. They were informed about the purpose of the study and the procedure and told that refusal to participate would not affect their treatment. All of the participants were asked to sign an informed consent form.
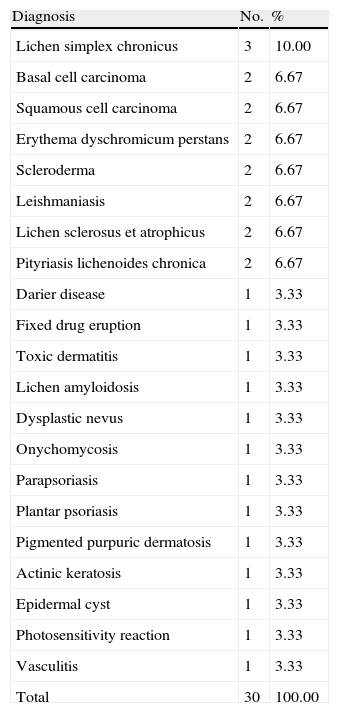
ResultsAlmost two-thirds (63.33%) of the patients were female and 30% were aged between 50 and 59 years. The diagnoses confirmed by biopsy sent by CHDAAM for each patient are shown in Table 1. This information was used to calculate the percentage of correct diagnoses made by the dermatologists after the face-to-face consultation, after the teleconsultation, and after the dermatologists from the teleconsultation group had seen the patients (Table 2).
Diagnoses Confirmed by Biopsy for the Patients (n=30) Evaluated at the Weekly Case Conferences at Hospital Santo Tomás in Panama in April 2009.
| Diagnosis | No. | % |
| Lichen simplex chronicus | 3 | 10.00 |
| Basal cell carcinoma | 2 | 6.67 |
| Squamous cell carcinoma | 2 | 6.67 |
| Erythema dyschromicum perstans | 2 | 6.67 |
| Scleroderma | 2 | 6.67 |
| Leishmaniasis | 2 | 6.67 |
| Lichen sclerosus et atrophicus | 2 | 6.67 |
| Pityriasis lichenoides chronica | 2 | 6.67 |
| Darier disease | 1 | 3.33 |
| Fixed drug eruption | 1 | 3.33 |
| Toxic dermatitis | 1 | 3.33 |
| Lichen amyloidosis | 1 | 3.33 |
| Dysplastic nevus | 1 | 3.33 |
| Onychomycosis | 1 | 3.33 |
| Parapsoriasis | 1 | 3.33 |
| Plantar psoriasis | 1 | 3.33 |
| Pigmented purpuric dermatosis | 1 | 3.33 |
| Actinic keratosis | 1 | 3.33 |
| Epidermal cyst | 1 | 3.33 |
| Photosensitivity reaction | 1 | 3.33 |
| Vasculitis | 1 | 3.33 |
| Total | 30 | 100.00 |
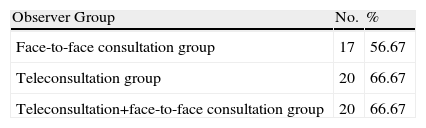
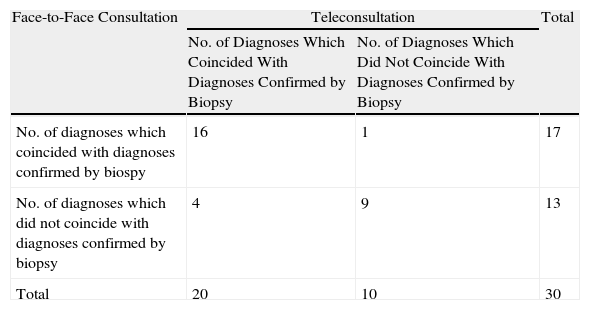
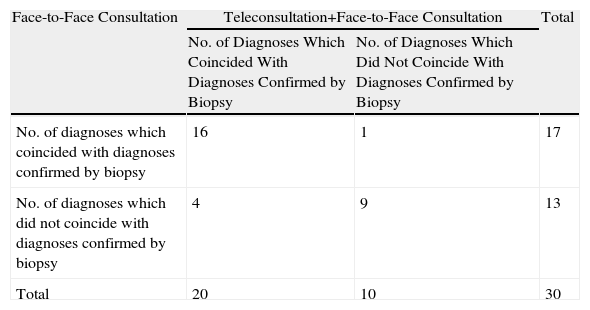
To calculate the level of diagnostic agreement between the face-to-face consultation group (observer group 1) and the teleconsultation group (observer group 2), we determined (1) how many diagnoses in each group coincided with the diagnosis confirmed by biopsy, (2) how many diagnoses in each group did not coincide with this diagnosis, and (3) how many diagnoses were correct in one group but incorrect in the other (Table 3). We also calculated the level of diagnostic agreement between the face-to-face consultation group (observer group 1) and the teleconsultation group after they had examined the patients in person (observer group 3) (Table 4).
Diagnostic Agreement Between Face-to-Face Consultation Group and Teleconsultation Group.
| Face-to-Face Consultation | Teleconsultation | Total | |
| No. of Diagnoses Which Coincided With Diagnoses Confirmed by Biopsy | No. of Diagnoses Which Did Not Coincide With Diagnoses Confirmed by Biopsy | ||
| No. of diagnoses which coincided with diagnoses confirmed by biospy | 16 | 1 | 17 |
| No. of diagnoses which did not coincide with diagnoses confirmed by biopsy | 4 | 9 | 13 |
| Total | 20 | 10 | 30 |
Diagnostic Agreement Between Face-to-Face Consultation Group and Teleconsultation+Face-to-Face Consultation Group.
| Face-to-Face Consultation | Teleconsultation+Face-to-Face Consultation | Total | |
| No. of Diagnoses Which Coincided With Diagnoses Confirmed by Biopsy | No. of Diagnoses Which Did Not Coincide With Diagnoses Confirmed by Biopsy | ||
| No. of diagnoses which coincided with diagnoses confirmed by biopsy | 16 | 1 | 17 |
| No. of diagnoses which did not coincide with diagnoses confirmed by biopsy | 4 | 9 | 13 |
| Total | 20 | 10 | 30 |
The percent agreement between groups 1 and 2 and between groups 1 and 3 was 83.33%.
The level of diagnostic agreement between the dermatologists in the face-to-face consultation group and the teleconsultation group was good (κ=0.6512). Differences due to interobserver variability were ruled out because a κ value of 0.6512 was also observed between the face-to-face consultation group and the teleconsultation group after they had examined the patients in person. This confirmed that both groups had similar diagnostic skills.
DiscussionThe percent agreement between the face-to-face consultation group and the teleconsultation group was 83.33% (0.83). This percentage is similar to rates reported in a review of 9 studies that compared the diagnostic reliability of store-and-forward teledermatology and face-to-face consultation.23 The total aggregate agreement for the 9 studies was 0.80, which is very similar to our rate of 0.83.
The diagnostic agreement between face-to-face consultation and teleconsultation followed by face-to-face consultation was good (κ=0.6512), showing that the dermatologists produced similar diagnoses when working under the same conditions. This allowed us to conclude that any differences detected between the groups would be attributable to the type of consultation rather than to the level of training of the dermatologists. The diagnostic agreement between face-to-face consultation and teleconsultation only was also good (κ=0.6512). Similar results were reported in a study comparing the reliability of store-and-forward teledermatology and face-to-face consultation for diagnosing and planning the surgical treatment of skin cancer.32 The authors of that study reported a κ value of 0.86 for the diagnostic agreement between the 2 types of consultation and a κ value of 0.75 for the agreement between the technique chosen using teledermatology and that finally used in surgery. These levels are even higher than ours and demonstrate a high level of diagnostic agreement between face-to-face and remote evaluation in dermatology patients.32
Most studies comparing teleconsultation and face-to-face consultation in dermatology have focused on reproducibility (intraobserver reliability) or on the level of agreement between different observers (interobserver reliability). In our review of the literature, however, we found no studies that analyzed diagnostic agreement between teams of observers. This makes our findings even more interesting.
Our findings also have important implications for dermatology patients in more remote parts of Panama who find it very difficult to travel to the capital to be evaluated at the case conferences held at Hospital Santo Tomás. We have shown that, in such cases, the dermatologist could send the patient's clinical history and images to the on-site dermatologists for evaluation. It should be noted that face-to-face consultation is the preferred method for diagnosing skin conditions but store-and-forward teledermatology proved to be reliable in this respect and can therefore be used with confidence when a face-to-face examination is not possible. A limitation of our study is that we only analyzed dermatologists; this means that our results cannot be extrapolated to teleconsultation between general practitioners and dermatologists. This needs to be analyzed in further studies.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We thank Drs Medrano, de Luque, Escala, Montilla, Samudio, Ávila, Saavedra, Duarte, Donderis, McKeever, Sánchez, Archbold, Ríos Castro, Yuil de Ríos, Escartín, Quesada, Suárez, Trujillo, Peralta, Ramírez, Villanueva, España, Arosemena, Llauradó, Marchena, Correa, Muñoz, Grajales, Martínez, Coutté, Fernández, Mora, González, Schlager, Rodríguez, Gaudiano, Valdés, Martín, Leyton, and Martíz for their contributions to this paper. We would also like to thank Ms Meneses, Ms Cedeño, and Ms Reyna for their assistance in managing the patients who participated in this study.
This study was awarded first prize in the Dr. Miguel Ahumada Padilla competition organized by the Colegio Ibero-Latino-Americano de Dermatología and the Sociedad Mexicana de Cirugía Dermatológica y Oncológica A.C at the XVII Ibero Latin American Dermatology Congress held in Cancun, Mexico on November 14, 2010.
Please cite this article as: Ríos-Yuil JM. Correlación del Teleateneo con el Ateneo prsencial de Dermatología en el diangóstico de las patologías. Actas Dermosifiliogr. 2012;103:138–43.