The diagnosis of disorders of the hair and scalp can generally be made on clinical grounds, but clinical signs are not always diagnostic and in some cases more invasive techniques, such as a biopsy, may be necessary. This 2-part article is a detailed review of the histologic features of the main types of alopecia based on the traditional classification of these disorders into 2 major groups: scarring and nonscarring alopecias. Scarring alopecias are disorders in which the hair follicle is replaced by fibrous scar tissue, a process that leads to permanent hair loss. In nonscarring alopecias, the follicles are preserved and hair growth can resume when the cause of the problem is eliminated. In the first part of this review, we describe the histologic features of the main forms of nonscarring alopecia. Since a close clinical-pathological correlation is essential for making a correct histologic diagnosis of alopecia, we also include a brief description of the clinical features of the principal forms of this disorder.
El diagnóstico de las enfermedades del cabello y del cuero cabelludo se basa, en la mayoría de las ocasiones, en el reconocimiento de signos clínicos; sin embargo, dichos signos no siempre son característicos y, en ocasiones, tenemos que recurrir a técnicas más invasivas como la realización de una biopsia. En este artículo se revisa de forma detallada las principales formas de alopecia desde un punto de vista histopatológico, y para ello se utiliza la clasificación tradicional de las alopecias que las divide en 2 grandes grupos: las alopecias cicatriciales y las no cicatriciales. Las alopecias cicatriciales son aquellas en las cuales el folículo piloso es sustituido por tejido fibroso cicatricial, causando una pérdida permanente del cabello. En las alopecias no cicatriciales el folículo permanece intacto y puede retomar su actividad cuando cesa el estímulo desencadenante. La primera parte de este artículo revisa las principales formas de alopecia no cicatricial desde un punto de vista histopatológico. Dado que una buena correlación clínico-patológica es fundamental para realizar el correcto diagnóstico histopatológico de las alopecias, en este artículo se incluye también una breve descripción de las características clínicas de las principales formas de alopecia.
In our daily clinical practice, dermatologists often encounter patients consulting for alopecia. In many cases, these processes can be correctly and rapidly diagnosed from the presentation and course of hair loss. However, sometimes, biopsy is necessary to enable a definitive diagnosis to be established. The first part of this article reviews in detail the main forms of nonscarring alopecia from a histopathological standpoint. Our review will follow the traditional classification of alopecia into scarring alopecias and nonscarring alopecias.1 Scarring alopecias are those in which the hair follicle is replaced by fibrous scar tissue while in nonscarring alopecias, the hair follicles resume their normal activity once the inflammatory process affecting them has been resolved.2
Hair CycleTo describe the histopathology of alopecias, we must have a good understanding of the hair cycle and the morphological changes that the hair follicles undergo in each of the phases of the cycle. Alopecias will generally more frequently involve a given phase of the hair cycle, with anagen, that is, the active growth phase (with DNA synthesis and melanogenesis), being the most vulnerable.3–9 When a hair follicle in anagen undergoes a reversible aggression, the growth phase is shortened to give rise to early catagen and telogen. This conversion from a metabolically highly active phase to an almost inert one helps prevent irreversible damage to the hair follicle, thereby allowing the growth of new hair shafts once the aggression ceases.10–12 Of the 100 000 hair follicles in the normal human scalp, approximately 85% are in anagen, with a mean duration in this phase of 2 to 7 years. In late anagen, the inferior segment of the hair follicles lies in the deep dermis or the hypodermis and typically has a pincer-like appearance,3 with the papilla surrounded by germ cells that keratinize as they ascend. After anagen, the hair follicle enters into catagen, the shortest phase of the cycle, with a duration of approximately 2 to 3 weeks. Catagen is characterized by retraction of the inferior segment of the hair follicle, which is positioned nearer the surface, leading to corrugation of the outer root sheath giving it an undulating appearance, with disperse apoptotic cells, especially in the lower part.13 In a normal scalp, only 1% to 2% of these hair follicles are in catagen and it is common not to see any in this phase in a biopsy. However, the number of follicles in catagen can increase significantly in certain alopecias such as tricothylamany.1 Telogen is the last phase of the hair cycle, lasting for a mean of 3 months. In this phase, DNA synthesis has completely stopped and melanogenesis has been interrupted. At the end of telogen, the hair shaft detaches, and a new hair cycle begins. Follicles in telogen have a retracted and bulky lower segment (telogen club hair) in the middle and upper dermis, and appear composed mainly of the permanent part of the hair follicle (infundibulum and isthmus). They therefore have the form of a club and are surrounded by sheaths of retracted perifollicular connective tissue. In addition, an angiofibrotic streamer is often present in this phase, running from the isthmus to the subcutaneous cellular tissue, clearly revealing the site where the lower segment of the follicle is located.2 The stem cells of the hair follicle are found where the outer root sheath widens at site of insertion of the arrector pili muscle. This structure is known as the bulge. Recently, relatively specific immunohistochemical markers such as PHLDA1 have been identified for these follicular stem cells.14,15 In each hair cycle, activation of these cells will give rise to the reappearance of the transient portion of the hair follicle and thus to a new hair cycle. Permanent damage to these stem cells is the common feature of the pathophysiology of all scarring alopecias.16,17
Nonscarring AlopeciasIn the physical exploration of nonscarring alopecias, follicular orifices can sometimes still be seen. This is key to diagnosis to differentiate from scarring alopecias, where the follicular orifices appear obliterated. This observation correlates histopathologically with the presence of follicular units with capacity for synthesizing hair shafts, and is the reason why areas of alopecia become repopulated after removing the trigger for hair loss. In the study of nonscarring alopecias, it is very useful to assess the follicular density and dynamics of the hair cycle (phase of the cycle in which the hair follicles observed histopathologically are found). For this, it is preferable that the biopsies are transversal sections, as this makes it possible to observe many hair follicles in different phases at the same time. In addition, for the biopsy to be useful, the sample must be taken from an active region of the lesion. In alopecias with a patchy morphology, it is preferable to take the sample from the edge of the lesion, whereas with diffuse alopecias the sample should be taken from a region with a positive hair pull test. Whenever possible, it is also useful to obtain a biopsy from the occipital region, as this will lower the chance of encountering hair follicles with androgenic effects, which if present may mean that the sample is not representative. Finally, when we assess a sample from a patient with nonscarring alopecia, we should remember that the disease is a dynamic process, and so histopathologic findings may vary according to the point in the process at the time of biopsy.18 The key histopathological findings of use in the diagnosis of nonscarring alopecias are summarized in Table 1.
Key Histopathological Features of Nonscarring Alopecias.
| Type of Alopecia | Key Histopathological Features |
|---|---|
| Androgenic Alopecia | Miniaturization of hair follicles |
| Sebaceous pseudohyperplasia | |
| Telogen Effluvium | Predominance of hair follicles in telogen |
| Absence of significant histopathological changes | |
| Alopecia Areata | Peri- and intrabulbar lymphocytic infiltrate (honeycomb pattern) |
| Several follicles from the biopsy in the same phase of the cycle | |
| Inversion of the anagen to telogen ratio | |
| Syphilitic Alopecia | Abundant plasma cells in the inflammatory infiltrate |
| Presence of Treponema pallidum with immunohistochemical staining | |
| Trichotillomania | Absence of peribulbar inflammatory infiltrate |
| Trichomalacia | |
| Incontinentia pigmenti | |
| Intra and perifollicular hemorrhage | |
| Traction Alopecia | Similar to trichotillomania |
| Reduction of terminal hair follicles |
Androgenic alopecia, or common baldness, is considered as a normal and physiological progression of hair follicles in the scalp rather than a disease as such. The underlying cause of androgenic alopecia is an increased sensitivity of the hair follicles to androgens. This is determined genetically and varies according to the region of the scalp, with the follicles in the occipital zone being the least affected.19 It has been shown that both women and men with androgenic alopecia show higher levels of activity of the enzyme 5α-reductase in the follicles of the frontal region of the scalp, when compared with the activity of follicles of the occipital region of the same patient.20 This may explain the different sensitivity to androgens in certain areas of the scalp. The pattern of androgenic alopecia is different in men and women. Men tend to show a bitemporal receding hairline with subsequent involvement of the frontotemporal region and vertex whereas women start with diffuse hair loss, which mainly affects the central area of the scalp.21–23
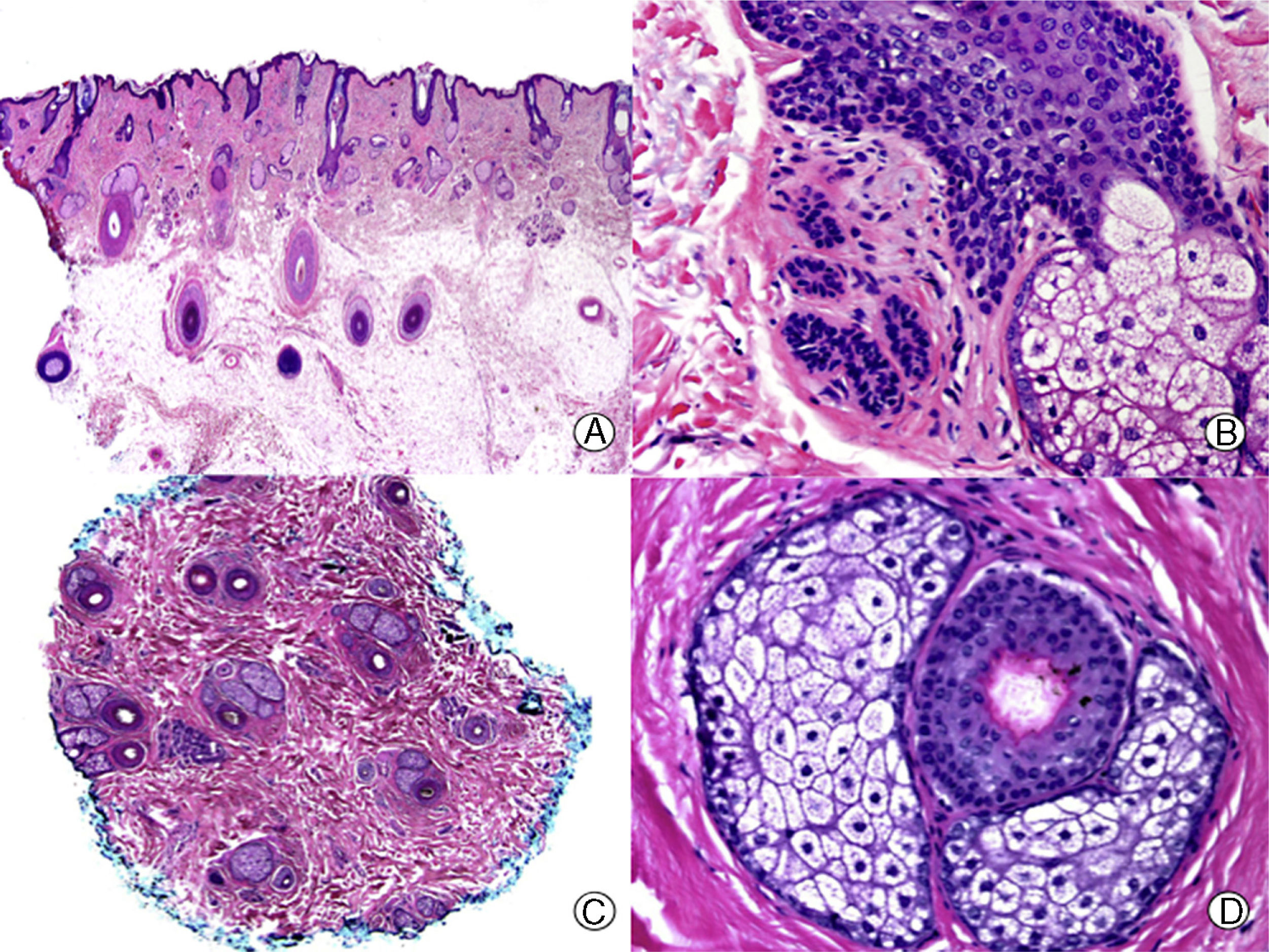
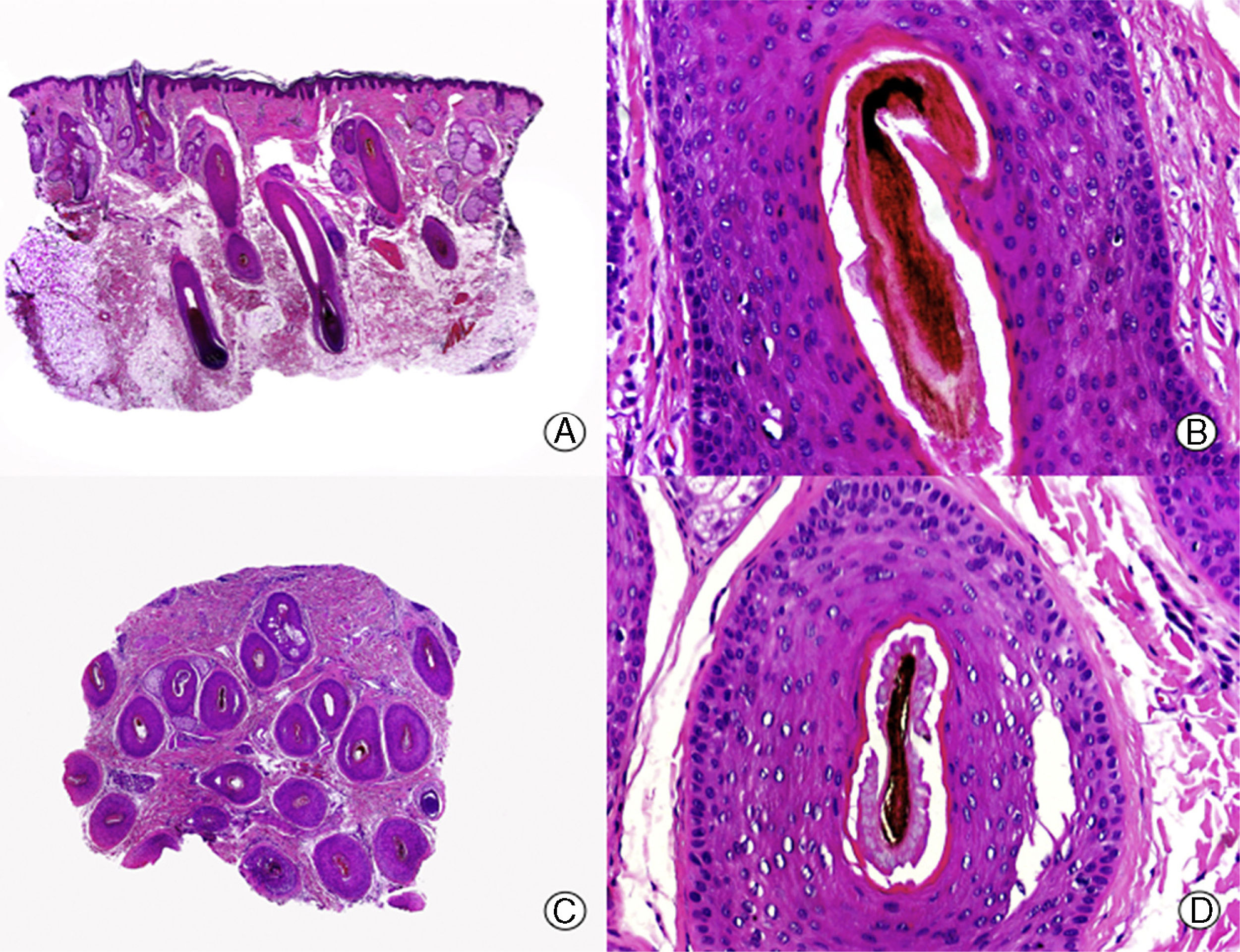
The key histopathological finding in androgenic alopecia is progressive miniaturization of terminal hair follicles,24–29 leading some of them to convert into vellus follicles (Figure 1). However, the total number of hair follicles remains stable, with a reduction in their size and depth and a smaller diameter of the hair shaft.30,31 The earliest change that can be observed in biopsies of androgenic alopecia is focal basophil degeneration of the vitreous membrane of the follicles in anagen.32 In addition, with the miniaturization, there is an ascent of the inferior segment of the hair follicles towards the superficial dermis, accompanied by an increase in the number of fibrous tracts. Thus, there is an increase in the number of follicles in telogen and a decrease in the normal anagen to telogen ratio from 7:1 to 2:1.33 Another characteristic of androgenic alopecia is the presence of apparently larger sebaceous glands compared to the size of the miniaturized hair follicles. But this observation is really only an apparent sebaceous hyperplasia as the sebaceous glands are of normal size and morphology,34 but they appear larger compared to the miniaturized hair follicles.
Androgenic alopecia. A, The longitudinal sections show a miniaturization of the terminal follicles, which convert to vellus follicles (hematoxylin-eosin [HE] x 20). B, Miniaturized hair follicles and apparently hypertrophic sebaceous glands (HE x 200). C, Same case studied with transversal sections, with several hair units of smaller size than normal in the scalp (HE x 20). D, Detail of the previous image in which sebaceous glands can be seen with a proportionally greater volume compared to the size of the hair follicles (HE x 200).
The presence and significance of inflammatory infiltrate is a topic of debate in androgenic alopecia. Traditionally, the presence of an inflammatory infiltrate was a histopathological finding that pointed away from androgenic alopeica,35 but several authors have reported inflammatory infiltrate in up to 75% of patients with androgenic alopecia, without any clinical signs of inflammation in the physical exploration.30,31,36–38 This infiltrate, mainly composed of lymphocytes, is usually found around the infundibulum, but it has also been observed around the fibrous streamers.
On staining for elastic fibers, the biopsies from patients with androgenic alopecia show Arao-Perkins bodies, which consist of small aggregates of elastic fibers in the fibrous streamers.39 They appear because of the agglomeration of elastic tissue surrounding the neck of the follicular papilla during catagen, marking the initial site of the follicular papilla in the previous cycle. In advanced androgenic alopecia, multiple Arao-Perkins bodies can be observed in the fibrous streamers, located increasingly nearer the surface.40 According to Pinkus,8 these findings are diagnostic of androgenic alopecia.
Telogen EffluviumTelogen effluvium is a disorder of the hair cycle in which one or more etiologic agents of different characteristics give rise to an early finalization of anagen. The underlying cause of this condition is an alteration of the biological clock of the follicular growth cycle, with a premature transition of the follicles from anagen to telogen.41–43 This early transition can be caused by a variety of situations, including surgery, infection, general anesthetic, surgical stress, and several intercurrent systemic diseases. These processes usually occur 2 to 3 months before the onset of effluvium (the time equivalent to the duration of telogen). Patients experience diffuse hair loss, and if we examine the detached hairs under the microscope, we see the typical club shape characteristic of telogen.9
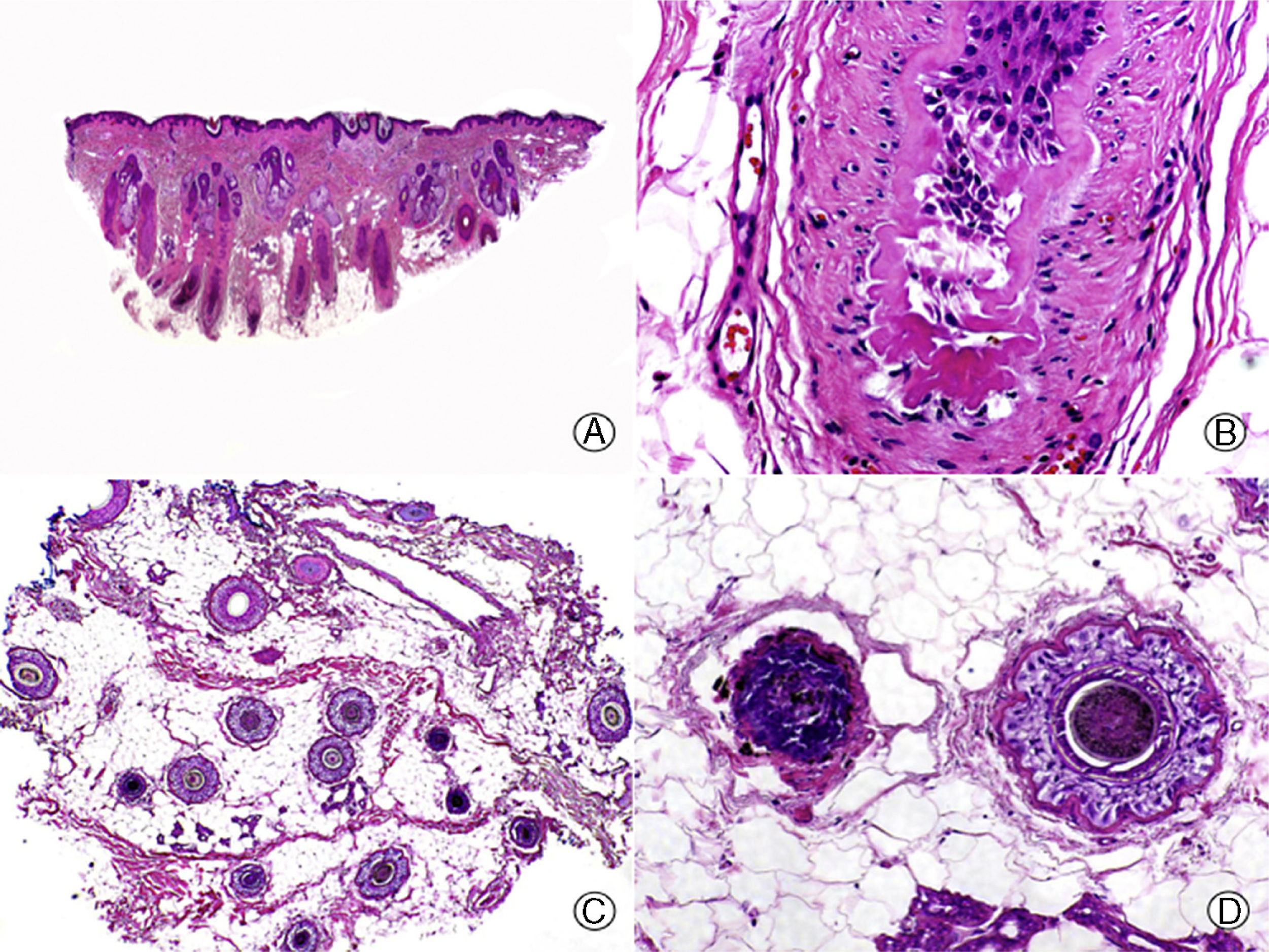
In all nonscarring alopecias, it is important to know where in the process the patient is, given that the histopathological characteristics vary according to disease progression. This is particularly important in telogen effluvium, where a trigger leads to a sudden transition of the follicles from anagen to telogen (Figure 2), but subsequently a new hair cycle begins. The biopsy in a patient with telogen effluvium is therefore usually normal. Thus, if we suspect telogen effluvium and we perform a biopsy with normal findings, we would be faced with a typical case of telogen effluvium, as the patients do not usually attend the dermatologist until they notice hair loss, which is usually when the disease is in an advanced phase.44,45 Only if we take a biopsy in an initial phase from a patient with telogen effluvium will we be able to detect a decrease in the ratio of anagen-to-telogen follicles, with a percentage of follicles in telogen of greater than 25%.46 In addition, in biopsies of telogen effluvium, we do not observe follicular abnormalities,47 inflammatory infiltrate, or an increase in fibrous streamers, while the number of follicles is normal.48 It is important to remember that some patients, especially men, can present with androgenic alopecia at the same time as telogen effluvium, and so it is important that the biopsy is performed in the occipital region of the scalp.
Chemotherapy-induced telogen effluvium. A, Longitudinal sections showing several hair follicles in telogen, surrounded by thick perifollicular connective sheaths (hematoxylin -eosin [HE] x 10). B, Detail of the previous image showing a thick, corrugated vitreous membrane around the telogen club hair (HE x 200). C, Same case studied with transversal sections, with several hair units (HE x 20). D, Detail of the previous image showing a corrugated outer root sheath surrounded by a thick vitreous membrane (HE x 200).
Chronic telogen effluvium is described as diffuse hair loss lasting more than 6 months. It differs from acute telogen effluvium in that it is more common among women (especially during menopause) and its etiology is not so clear. Onset is usually sudden and progression fluctuates but is self-limiting; in addition it often presents as a bitemporal regression of the hairline.49,50 It has been suggested that the process is due to a decreased duration of the anagen phase, thereby impeding the growth of long hairs.45,51 Biopsy reveals a scalp that hardly differs, if at all, from a normal scalp, with a slight increase in the percentage of follicles in telogen if the biopsy is performed during the most active phases. According to Whitting,52 hair loss in the absence of histopathological changes is characteristic of this condition. To differentiate from female-pattern androgenic alopecia, whose clinical characteristics are very similar, it is useful to determine the telogen to anagen ratio in the biopsy. In the case of female-pattern androgenic alopecia, this ratio is usually increased but does not exceed 4:1, whereas if the ratio is greater than 8:1, this is indicative of chronic telogen effluvium.53
Alopecia AreataAlopecia areata is a relatively common cause of alopecia. The most likely pathogenesis is a genetically determined autoimmune disorder mediated by T lymphocytes against aberrant HLA-RR expressed by keratinocytes of the hair follicles.54,55 It tends to affect children and young adults more frequently but can present at any age. It is manifest clinically as one or several oval or round patches of alopecia, without loss of follicular orifices. The process can affect any hair-bearing region of the body. In alopecia areata, characteristically, hairs in the form of exclamation marks can be seen, particularly at the margins of the lesion. These correspond to small broken hairs, with a conical attenuated bulb and thicker distal end.56,57
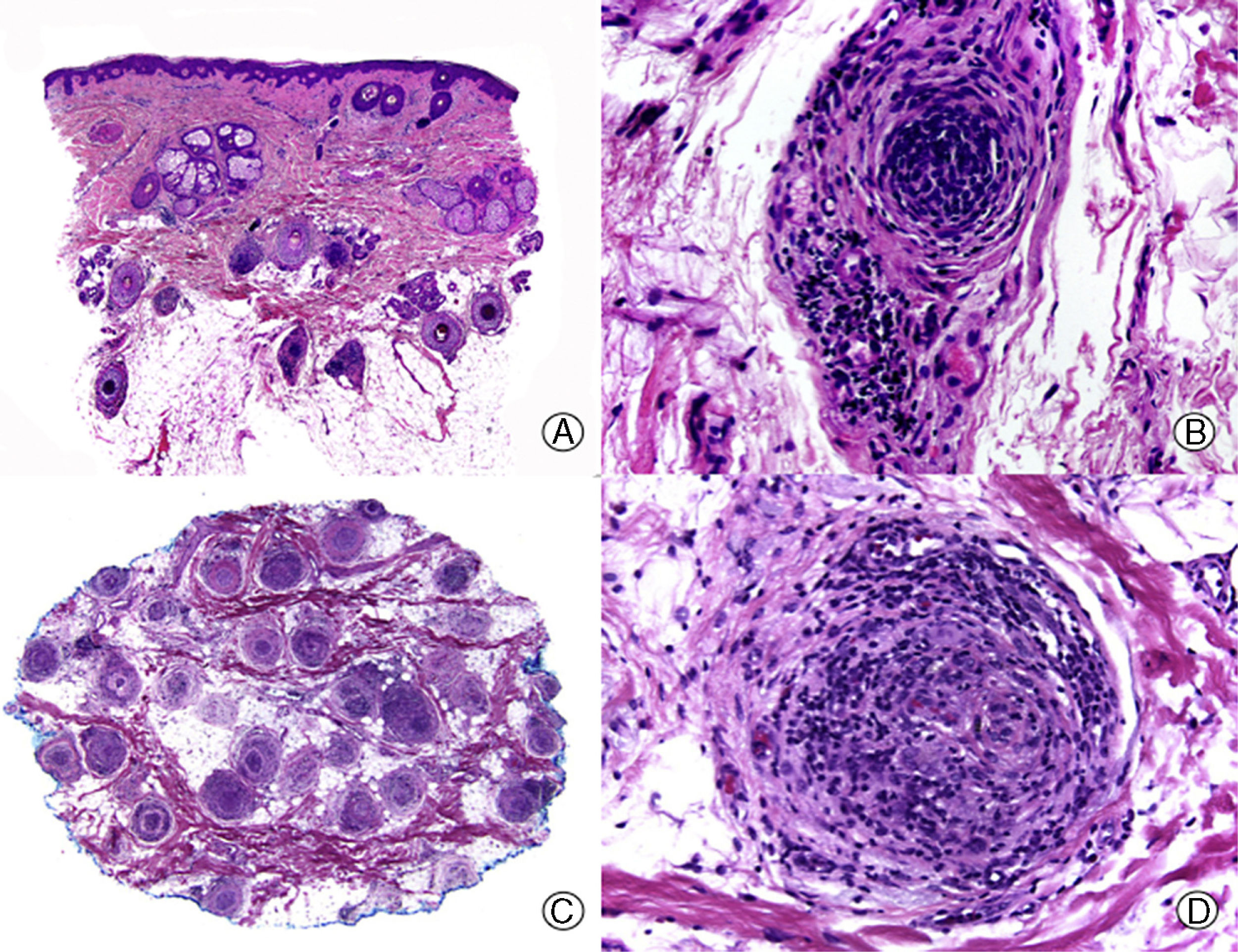
From the histopathological point of view, alopecia areata is characterized by the presence of an inflammatory infiltrate of small lymphocytes that surround the bulb of the follicles in anagen (Figure 3), thereby inducing early conversion to catagen and telogen. The infiltrate adopts a peri- and intrabulbar distribution, creating a honeycomb effect, and is composed mainly of CD4+ T lymphocytes and Langerhans cells. Histiocytes, plasma cells, mast cells, and eosinophils can also be observed.58–63 T lymphocytes induce apoptosis of matrix cells of the bulb, starting with the peripheral ones, which are the ones responsible for the formation of the inner root sheath and the cortex of the hair shaft.62 This gives rise to a narrowing of the hair shaft, which is responsible for the appearance of exclamation mark hairs. This also induces an early transition from catagen to telogen, in turn leading to a reversal of the anagen to telogen ratio, typical in alopecia areata. Therefore, in biopsies of this process, there is an increased number of follicles in catagen and telogen, all with an accompanying fibrous streamer. This abundance of hair follicles all in the same phase of the cycle is a key to the diagnosis of alopecia areata.64 However, the characteristic inflammatory infiltrate that is normally observed in alopecia areata may be absent at times, particularly in cases of long-standing disease. In such cases, it may be useful to search for other histopathological characteristics suggestive of alopecia areata, such as the presence of eosinophils, lymphocytes, and melanin in the fibrous streamers. Other characteristics, less specific to alopecia areata but nevertheless of assistance in diagnosis include an increased number of follicles in catagen and telogen, incontinentia pigmenti (both peribulbar and in the fibrous streamer), and tricholamalacia. In alopecia areata, but also in other forms of alopecia, a proliferation of ducts similar to syringoma can be observed, although these lack the sclerotic stroma characteristic of this tumor. This is therefore thought to correspond to a reactive ductal hyperplasia.65 Moreover, in longstanding alopecia areata, there is a miniaturization of the hair follicles with an almost complete absence of terminal follicles.
Alopecia areata. A, Longitudinal sections showing an inflammatory infiltrate surrounding the bulbs of the terminal hair follicles (hematoxylin-eosin [HE] x 10). B, Detail of the previous image showing that the inflammatory infiltrate is made up mainly of lymphocytes (HE x 200). C, Transversal sections of the same case showing an inflammatory infiltrate around the inferior segment of several of the hair follicles (HE x 10). D, Detail of the previous image showing an intense lymphocyte infiltrate (HE x 200).
Unlike scarring alopecias, the inflammatory infiltrate in alopecia areata does not involve stem cells, so the hair follicle maintains its capacity to regenerate after an aggression. If the inflammation has resolved when the follicle enters a new growth cycle, the affected region will progressively repopulate. If, on the other hand, the follicle in anagen is still affected by the inflammatory infiltrate, the hair cycle will be interrupted once again in early anagen phase, leading to premature catagen and telogen66 and persistence of the disease. Although alopecia areata is a nonscarring condition, in chronic forms of alopecia areata resistant to treatment, biopsies show a lack of hair follicles and these appear to be replaced by nodules of fibroplasia and collagen tissue arranged in concentric rings. Such findings are indicative of alopecia areata in which repopulation will not occur.67
Syphilitic AlopeciaSyphilitic alopecia is a secondary manifestation of infection and is the result of inflammation caused by local aggression of Treponema pallidum on the hair follicles. Syphilitic alopecia rarely presents in isolation, but when it does so, whether in its patchy clinical presentation (moth-eaten alopecia) or its diffuse form, the clinician may be faced with diagnostic uncertainty as a high degree of clinical suspicion is required and in most cases it will be necessary to request syphilis testing to establish diagnosis.
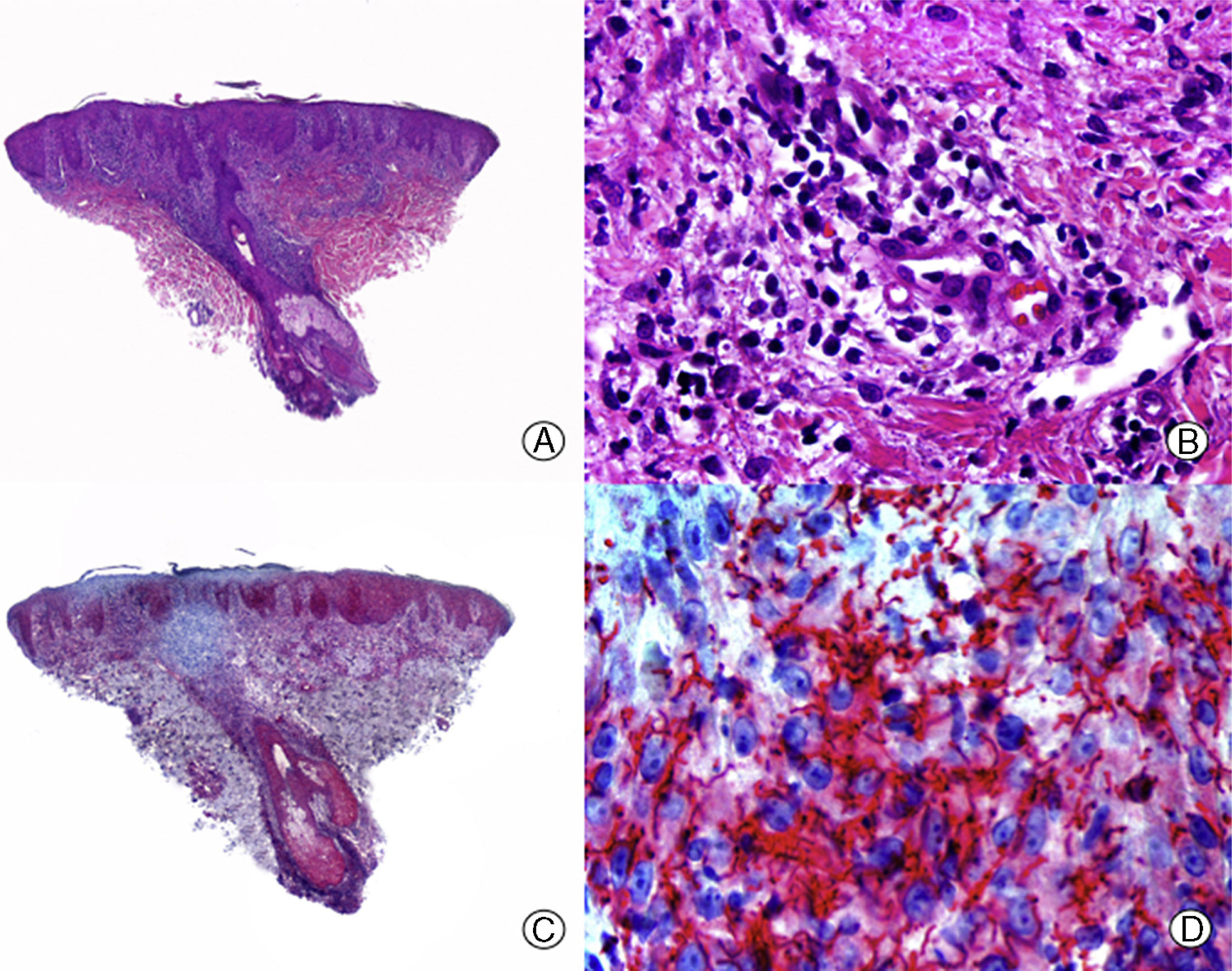
From the histopathological point of view, it is important to try to detect the spirochetes in the inflammatory infiltrate through histochemical study, as this is the most sensitive technique at present (Figure 4).68 Syphilitic alopecia presents as a lymphohistiocytic inflammatory infiltrate with a striking plasma cell component, which surrounds the fibrous streamers and the bulb. Moreover, in biopsies of syphilitic alopecia, we see an increase in the number of follicles in telogen and catagen. This latter observation is important in the differential diagnosis with alopecia areata as both show clinical and histopathological similarities. Different authors have searched for other histopathological findings that would help in the differential diagnosis of syphilitic alopecia and alopecia areata. One of the proposals has been the presence of eosinophils. Some studies, such as the one by Jordaan and Louw,69 describe the presence of eosinophils in syphilitic alopecia, whereas other authors, such as Lee and Hsu70 report their absence and consider this criterion useful for differential diagnosis with alopecia areata.
Syphilitic alopecia. A, A lichenoid infiltrate at the dermal-epidermal junction along with a dense perifollicular infiltrate (hematoxylin-eosin [HE] x 10). B. At higher magnification, we see that the infiltrate is made up mainly of lymphocytes and plasma cells (HE x 400). C. Immunohistochemistry of the same case for Treponema pallidum (HE x 10). D. Numerous treponemas between the epithelium of the outer root sheath of the follicle (HE x 400).
Trichotillomania is a self-inflicted pathological process, either consciously or unconsciously, in which patients experience the compulsion to twist or pull their hair and so achieve pleasure or relief.71 Such patients usually show an aberrant clinical pattern of alopecia, which generally involves the scalp but which can also affect any hair-bearing region of the body.72 The areas of alopecia appear patchy and with irregular borders. Characteristically, hair of different lengths can be seen, and in extreme cases, broken or frayed ends may be present due to pulling and breakage of the hairs over time. Unlike alopecia areata, the patches do not usually show complete hair loss, as the hair cycle progresses normally despite the constant aggressions.72
The consequences of hair follicle lesion due to repeated trauma are reflected histopathologically. Often, in the same biopsy, it is possible to observe alternating damaged and intact follicles, even very close to one another,73–75 and this finding correlates with the clinical observation of incomplete hair loss in the patches of alopecia. There is also a lack of perifollicular inflammatory infiltrate,76 although at times perivascular inflammation is observed in the superficial dermis. As evidence of trauma, the individual damaged follicles show tricholamalacia, incontinentia pigmenti, and intra- and perifollicular hemorrhage.76 Trichomalacia is the most characteristic histopathological finding of this disease, and refers to distortion of the hair shaft (Figure 5), although it may not always be present.75–77 The damage to bulbar melanocytes gives rise to incontinentia pigmenti, which is observed in the form of irregular pigmented masses in the permanent part of the follicle, both in the infundibulum and in the isthmus, occupying the now corrugated outer root sheath.75 In fair- and red-haired individuals, it is uncommon to find these accumulations of pigment.18 Follicular hemorrhages appear in the early phases of the process and are not a constant finding, but when they are observed, they constitute a finding that almost confirms diagnosis of trichotillomania.44 It is sometimes possible to observe a granulomatous reaction around the follicles of the hairs that have been pulled out, probably in response to broken hair shafts in direct contact with the dermis and without the protection afforded by the follicular root sheaths.3,10 The presence of empty follicular channels76 is also a common finding in this process, but unfortunately it does not help diagnosis as this is a frequent finding in many of the scalp biopsies due to the microtome actions. If it is possible to obtain a biopsy with the hair shafts conserved, the characteristic hamburger sign can be seen, resulting from longitudinal breakage of the hair shaft with accumulation of protein material and erythrocytes in the resulting intermediate space.78
Trichotillomania. A, Longitudinal sections showing normal hair follicles in alternation with abnormal ones (hematoxylin-eosin [HE] x 10). B, Trichomalacia showing pigmented and corrugated shafts in the follicular channel (HE x 200). C, Same case studied with transversal sections (HE x20). D, Detail of the previous image in which a broken hair shaft is observed with abundant pigment (HE x 200).
Transversal sections show an increase in the number of follicles in catagen in the earliest stages.36,75–77 As with alopecia areata, lesion of follicles in anagen hastens the transition to catagen and telogen. According to Whitting,12 trichotillomania is the alopecia in which most follicles are in catagen, although the total number of follicles or the ratio of terminal to vellus follicles does not vary. The main histopathological criterion for establishing differential diagnosis with alopecia areata is the absence of peribulbar inflammatory infiltrate in trichotillomania.
Traction AlopeciaTraction alopecia is included along with trichotillomania in the group of mechanically induced alopecias. The chronic form can be seen fairly often in clinical practice. In general, it is caused by inappropriate hair styling, such as pulled-back hair or the use of elastic bands for the hair.79 In this form, hair loss occurs in the regions where there is greatest traction, leading in time to a recession of the hairline or a widening of the separation between hair parting and progressive centrifugal hair loss.80
Traction alopecia is very well characterized from a clinical point of view, but its histopathological characteristics are not so well known. By and large, the histological findings of traction alopecia are very similar to those observed in trichotillomania, although over time it can give rise to a scarring alopecia, which is known as follicular degeneration syndrome.81 In the early phases, when the alopecia is still reversible, changes similar to those described for trichotillomania can be observed, such as the presence of trichomalacia and incontinentia pigmenti, although less severe and with fewer involved hair follicles.48 In advanced phases, when the alopecia is irreversible, regions of fibrosis can be observed in places where the terminal hair follicles were previously found.48 A characteristic finding of traction alopecia is a decrease in the number of terminal hair follicles, with a normal number of vellus follicles. Characteristically, inflammatory infiltrate is not observed at any time during the course of traction alopecia.1
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Bernárdez C, Molina-Ruiz AM, Requena L. Histopatología de las alopecias. Parte I: alopecias no cicatriciales. Actas Dermosifiliogr. 2015;106:158–167.


![Androgenic alopecia. A, The longitudinal sections show a miniaturization of the terminal follicles, which convert to vellus follicles (hematoxylin-eosin [HE] x 20). B, Miniaturized hair follicles and apparently hypertrophic sebaceous glands (HE x 200). C, Same case studied with transversal sections, with several hair units of smaller size than normal in the scalp (HE x 20). D, Detail of the previous image in which sebaceous glands can be seen with a proportionally greater volume compared to the size of the hair follicles (HE x 200). Androgenic alopecia. A, The longitudinal sections show a miniaturization of the terminal follicles, which convert to vellus follicles (hematoxylin-eosin [HE] x 20). B, Miniaturized hair follicles and apparently hypertrophic sebaceous glands (HE x 200). C, Same case studied with transversal sections, with several hair units of smaller size than normal in the scalp (HE x 20). D, Detail of the previous image in which sebaceous glands can be seen with a proportionally greater volume compared to the size of the hair follicles (HE x 200).](https://static.elsevier.es/multimedia/15782190/0000010600000003/v3_202209240641/S1578219015000141/v3_202209240641/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)
![Chemotherapy-induced telogen effluvium. A, Longitudinal sections showing several hair follicles in telogen, surrounded by thick perifollicular connective sheaths (hematoxylin -eosin [HE] x 10). B, Detail of the previous image showing a thick, corrugated vitreous membrane around the telogen club hair (HE x 200). C, Same case studied with transversal sections, with several hair units (HE x 20). D, Detail of the previous image showing a corrugated outer root sheath surrounded by a thick vitreous membrane (HE x 200). Chemotherapy-induced telogen effluvium. A, Longitudinal sections showing several hair follicles in telogen, surrounded by thick perifollicular connective sheaths (hematoxylin -eosin [HE] x 10). B, Detail of the previous image showing a thick, corrugated vitreous membrane around the telogen club hair (HE x 200). C, Same case studied with transversal sections, with several hair units (HE x 20). D, Detail of the previous image showing a corrugated outer root sheath surrounded by a thick vitreous membrane (HE x 200).](https://static.elsevier.es/multimedia/15782190/0000010600000003/v3_202209240641/S1578219015000141/v3_202209240641/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)
![Alopecia areata. A, Longitudinal sections showing an inflammatory infiltrate surrounding the bulbs of the terminal hair follicles (hematoxylin-eosin [HE] x 10). B, Detail of the previous image showing that the inflammatory infiltrate is made up mainly of lymphocytes (HE x 200). C, Transversal sections of the same case showing an inflammatory infiltrate around the inferior segment of several of the hair follicles (HE x 10). D, Detail of the previous image showing an intense lymphocyte infiltrate (HE x 200). Alopecia areata. A, Longitudinal sections showing an inflammatory infiltrate surrounding the bulbs of the terminal hair follicles (hematoxylin-eosin [HE] x 10). B, Detail of the previous image showing that the inflammatory infiltrate is made up mainly of lymphocytes (HE x 200). C, Transversal sections of the same case showing an inflammatory infiltrate around the inferior segment of several of the hair follicles (HE x 10). D, Detail of the previous image showing an intense lymphocyte infiltrate (HE x 200).](https://static.elsevier.es/multimedia/15782190/0000010600000003/v3_202209240641/S1578219015000141/v3_202209240641/en/main.assets/thumbnail/gr3.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)
![Syphilitic alopecia. A, A lichenoid infiltrate at the dermal-epidermal junction along with a dense perifollicular infiltrate (hematoxylin-eosin [HE] x 10). B. At higher magnification, we see that the infiltrate is made up mainly of lymphocytes and plasma cells (HE x 400). C. Immunohistochemistry of the same case for Treponema pallidum (HE x 10). D. Numerous treponemas between the epithelium of the outer root sheath of the follicle (HE x 400). Syphilitic alopecia. A, A lichenoid infiltrate at the dermal-epidermal junction along with a dense perifollicular infiltrate (hematoxylin-eosin [HE] x 10). B. At higher magnification, we see that the infiltrate is made up mainly of lymphocytes and plasma cells (HE x 400). C. Immunohistochemistry of the same case for Treponema pallidum (HE x 10). D. Numerous treponemas between the epithelium of the outer root sheath of the follicle (HE x 400).](https://static.elsevier.es/multimedia/15782190/0000010600000003/v3_202209240641/S1578219015000141/v3_202209240641/en/main.assets/thumbnail/gr4.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)
![Trichotillomania. A, Longitudinal sections showing normal hair follicles in alternation with abnormal ones (hematoxylin-eosin [HE] x 10). B, Trichomalacia showing pigmented and corrugated shafts in the follicular channel (HE x 200). C, Same case studied with transversal sections (HE x20). D, Detail of the previous image in which a broken hair shaft is observed with abundant pigment (HE x 200). Trichotillomania. A, Longitudinal sections showing normal hair follicles in alternation with abnormal ones (hematoxylin-eosin [HE] x 10). B, Trichomalacia showing pigmented and corrugated shafts in the follicular channel (HE x 200). C, Same case studied with transversal sections (HE x20). D, Detail of the previous image in which a broken hair shaft is observed with abundant pigment (HE x 200).](https://static.elsevier.es/multimedia/15782190/0000010600000003/v3_202209240641/S1578219015000141/v3_202209240641/en/main.assets/thumbnail/gr5.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)



