Upper-lip reconstruction after Mohs micrographic surgery is challenging for dermatologic surgeons. We describe a series of 15 patients (7 men and 8 women; mean age, 65.6 years) with skin cancer on the upper lip treated with Mohs surgery: 10 basal cell carcinomas, 2 melanomas, and 3 squamous cell carcinomas. The resulting defects measured between 3 and 7.6 cm. We used island flaps to reconstruct the defects in all cases, hiding the incisions in the nasolabial fold, at the line where the skin meets the vermillion border of the lip, and in the relaxed skin tension lines. We explain key aspects of the surgeries and design of the reconstructions, with emphasis on the importance of occasionally sacrificing small areas of healthy skin. Cosmetic and functional outcomes were satisfactory in all patients, and there were no postsurgical complications.
La reconstrucción del labio superior tras la cirugía de Mohs supone, en ocasiones, un reto para el cirujano dermatológico. Presentamos una serie de 15 pacientes (7 hombres y 8 mujeres; edad media 65,6 años) con cáncer cutáneo (10 carcinomas basocelulares, 2 melanomas y 3 carcinomas escamosos) localizados en el labio superior intervenidos mediante cirugía de Mohs con defectos resultantes de 3-7.6 cm. Para la reconstrucción se empleó un colgajo en isla del labio superior diseñado escondiendo las incisiones en el pliegue nasolabial, en la línea de unión del bermellón con la piel y en las líneas de tensión de la piel relajada. Se explican las claves del diseño y la cirugía, enfatizando en la importancia de sacrificar en ocasiones pequeñas zonas de tejido sano. Se alcanzaron resultados satisfactorios cosméticos y funcionales, sin complicaciones postquirúrgicas en todos los pacientes.
The upper lip is a common site for skin cancer. Reconstruction of the upper lip may be hampered by the limited availability of adjacent tissue and the by the functional and cosmetic importance of this anatomic unit. Options for reconstructive surgery depend on the size, location, and depth of the lesion.
Preservation of the function and appearance of the upper lip during reconstruction surgery must take into account the following: (1) Maintenance of symmetry in the nasolabial fold and the upper lip; (2) Sparing or reconstruction of the philtrum and Cupid’s bow without displacement; (3) Avoidance of creases at the line where the skin meets the vermillion border; (4) Avoidance of eclabium or upward traction on the vermillion border; and (5) Avoidance of horizontal scars by hiding incisions in natural folds or following relaxed tension lines or wrinkles.
In our experience, the subcutaneous island pedicle flap on the upper lip fulfills these norms and enables successful reconstruction of most defects at this site.
The objective of the present study was to review a series of patients who underwent reconstructive surgery in the upper lip based on an island flap and to describe and illustrate the surgical technique, taking into account basic practical considerations.
MethodsPatientsWe reviewed the clinical history and imaging data available for patients who underwent reconstruction surgery based on an island flap in the Dermatology Department of Clínica Universidad de Navarra, Pamplona, Spain between 2015 and 2019. Cosmetic and functional outcomes were evaluated independently by 2 dermatologists, and patients were asked about their satisfaction with the outcome. The study was approved by the Ethics Committee of Universidad de Navarra, and the patients provided their informed consent.
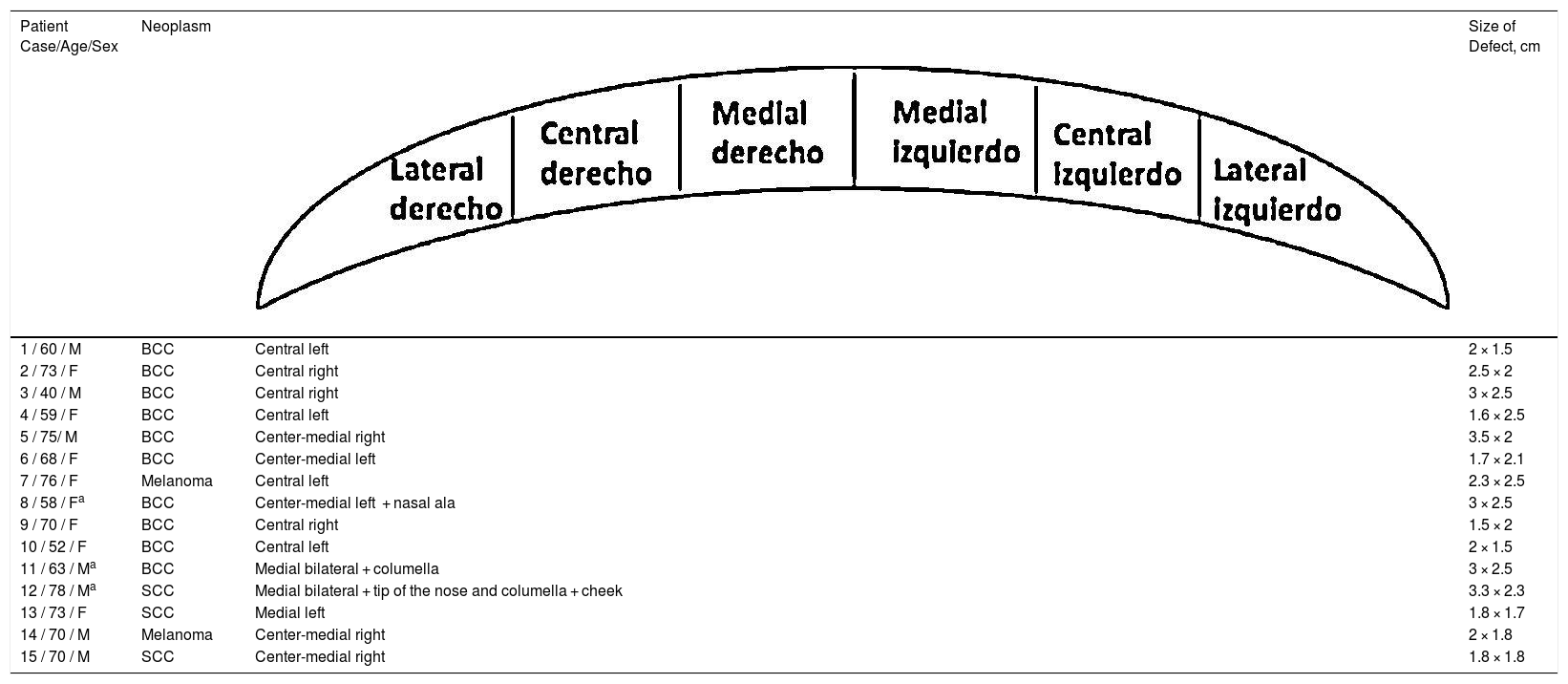
We selected 15 patients (7 men and 8 women, with a mean age of 65.6 years [range, 40-78 years]). The patients had had different types of skin cancer affecting the upper lip (basal cell carcinoma, 10 cases; melanoma, 2 cases; squamous cell carcinoma, 3 cases) that were treated with Mohs micrographic surgery (Table 1).
Characteristics of Patients, Neoplasms, and Defects in the Study Series.
| Patient Case/Age/Sex | Neoplasm | Size of Defect, cm | |
|---|---|---|---|
| 1 / 60 / M | BCC | Central left | 2 × 1.5 |
| 2 / 73 / F | BCC | Central right | 2.5 × 2 |
| 3 / 40 / M | BCC | Central right | 3 × 2.5 |
| 4 / 59 / F | BCC | Central left | 1.6 × 2.5 |
| 5 / 75/ M | BCC | Center-medial right | 3.5 × 2 |
| 6 / 68 / F | BCC | Center-medial left | 1.7 × 2.1 |
| 7 / 76 / F | Melanoma | Central left | 2.3 × 2.5 |
| 8 / 58 / Fa | BCC | Center-medial left + nasal ala | 3 × 2.5 |
| 9 / 70 / F | BCC | Central right | 1.5 × 2 |
| 10 / 52 / F | BCC | Central left | 2 × 1.5 |
| 11 / 63 / Ma | BCC | Medial bilateral + columella | 3 × 2.5 |
| 12 / 78 / Ma | SCC | Medial bilateral + tip of the nose and columella + cheek | 3.3 × 2.3 |
| 13 / 73 / F | SCC | Medial left | 1.8 × 1.7 |
| 14 / 70 / M | Melanoma | Center-medial right | 2 × 1.8 |
| 15 / 70 / M | SCC | Center-medial right | 1.8 × 1.8 |
All defects were reconstructed using a subcutaneous island pedicle flap on the upper lip.
Abbreviations: BCC, basal cell carcinoma; F, female; M, male; SCC, squamous cell carcinoma.
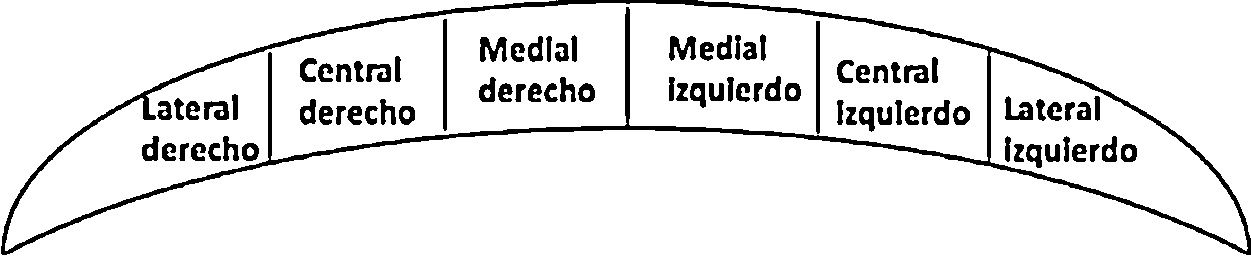
Each half of the upper lip (left and right) was divided into 3 parts (medial, central, and lateral) in order to describe the location of the defects (Table 1).
Surgical TechniqueAll of the patients had undergone Mohs micrographic surgery under local anesthetic (bupivacaine 0.5%), with resulting defects measuring from 3 to 7.6 cm2 (Table 1).
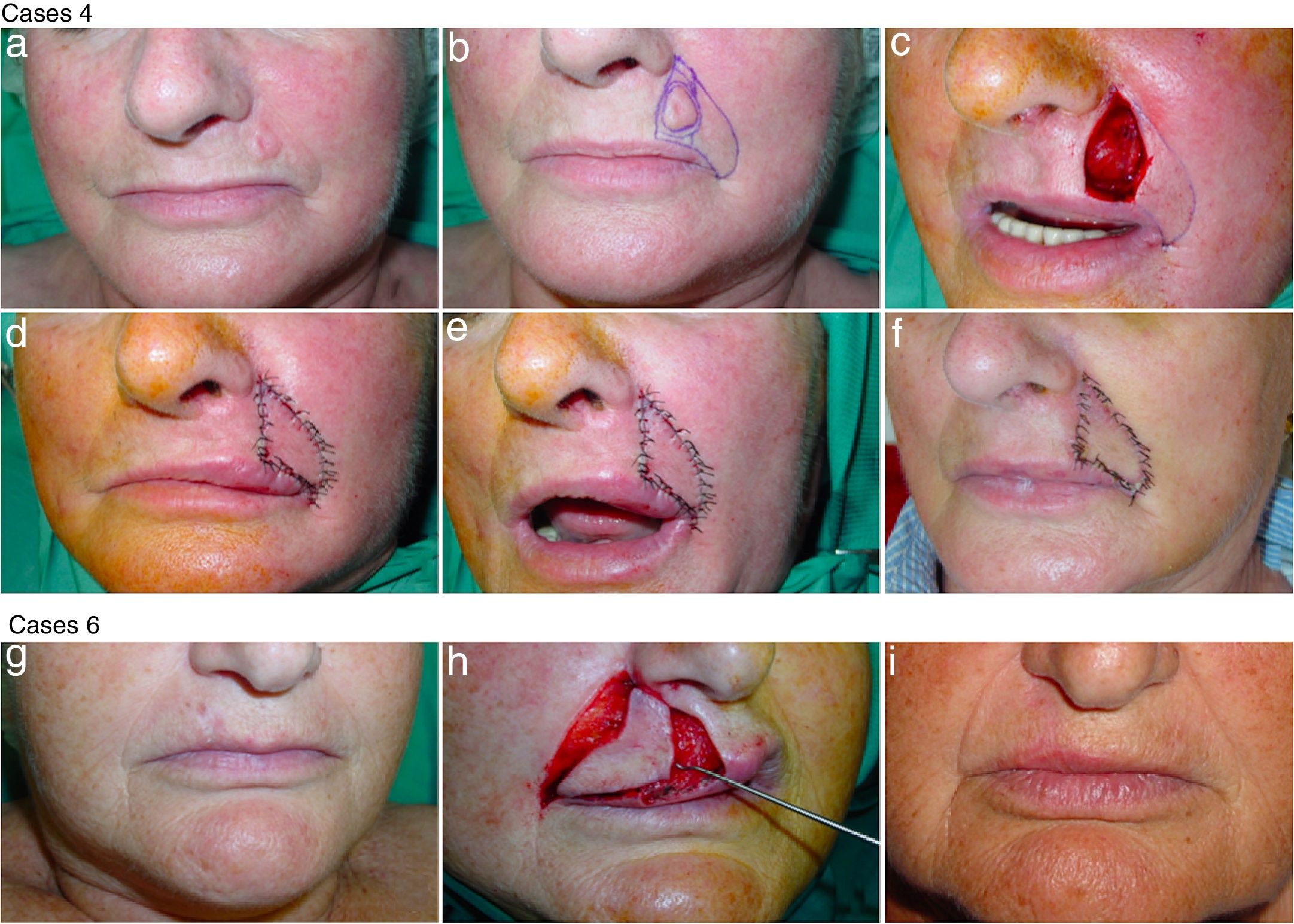
The steps for making the flap and reconstruction were as follows (Fig. 1):
- 1
Reconstruction started with adaptation of the final defect. It is essential for this to extend beyond the nasolabial fold and below the line where the skin meets the vermillion border. When this is not the case, a surgical skin marker can be used to draw the areas of healthy skin to be removed in order to adapt the defect and remove it. This first step makes it possible to achieve a more favorable cosmetic outcome, since it enables scars to be hidden in natural folds or lines, thus avoiding horizontal scars.
- 2
The island flap is designed. Using a surgical skin marker, a triangular flap is drawn; the medial part of the flap contains the defect. The upper part lies in the nasolabial fold and the lower part where the skin meets the vermillion border, in such a way that both lines converge on the natural wrinkles in the oral commissure. The size of the flap depends on the lines that delimit it. However, when the defect is larger, the upper side of the triangle can be extended with a line parallel to the nasolabial fold on the cheek.
- 3
The incisions are then made with a cold scalpel by marking out the design. The flap is cut and worked at the level of the subcutaneous tissue above the orbicular muscle. A subcutaneous pedicle must be maintained. This should be sufficiently thick to enable adequate vascularization of the flap and, at the same time, mobile in order to facilitate the advancement of the tissue.
- 4
Once adequate hemostasis has been achieved, the flap is advanced, and the wound is closed. The medial sutures are placed (normally first with an anchor at a reference point in the center of the medial side), followed by the remaining sutures. Subcutaneous stitches are placed first (Novosyn 4/0), followed by tension-free stitches (silk 6/0).
- 5
The secondary defect is closed directly using a V-Y technique.
- 6
A slightly compressive dressing is placed.
Design, surgical technique, and outcome based on 2 representative cases. Case 4. A, Basal cell carcinoma on the upper lip. B, Definition of the tumor with a margin to be excised using Mohs surgery and adaptation of the defect so that it reaches the nasolabial fold and the line where the skin of the upper lip meets the vermillion border. C, Final defect after removal with free borders and excision of the upper and lower healthy skin. Design of the flap following the nasolabial fold and the line where the skin of the upper lip meets the vermillion border, with both lines finishing at the angle of the natural wrinkles in the oral commissure. D and E, Sutured flap with simple stitches (silk 6/0). The upper and lower scars are hidden in natural lines and the medial scar is vertical, parallel to the wrinkles. F, Appearance at removal of the stitches 7 days after surgery. Case 6. G, Basal cell carcinoma on the right upper lip. H, Image of the flap, which, after being worked in the subcutaneous plane by maintaining a central subcutaneous pedicle that guarantees the blood supply, advances toward the defect. The lesion had previously been removed using Mohs surgery. I, Outcome 6 months after the procedure.
In 3 cases, the reconstruction involved variations owing to the larger size and/or location of the lesion. A bilateral island pedicle flap was placed in 2 cases (one by combining an advancement flap from the cheek and the other by combining the unilateral flap with a paramedian forehead flap to reconstruct the nasal ala).
ResultsAll of the flaps progressed satisfactorily without acute complications such as bleeding, infection, or necrosis and without the need for correction of scars. Postoperative follow-up was from 6 to 34 months.
The functional and cosmetic outcomes were satisfactory, both for the dermatologist and for the patient in all cases. Slight eversion of the upper lip was recorded in 1 case. In functional terms, mouth opening and upper lip mobility remained intact, and paresthesia was reported in the area in 4 cases during the days after the procedure, although this resolved after a few weeks. In cosmetic terms, the scars were hidden in natural lines, as follows: upper scar, in the nasolabial fold; lower scar, at the line where the skin meets the vermillion border; closure of the V-Y advancement flap, wrinkles of the oral commissure; and medial border, in a vertical scar hidden among the vertical wrinkles on the upper lip.
DiscussionLarge defects following Mohs surgery on the upper lip make reconstruction challenging because of the cosmetic and functional importance of this area. Local flaps are the main option for defects where direct closure is not possible. In most cases, we believe that the subcutaneous island pedicle flap of the upper lip is the reconstructive option of choice, taking into account a few basic considerations.
As commented on above, a key consideration is that of adapting the defect. It is not uncommon to find designs in which this flap has horizontal scars in the middle of the upper lip. This occurs when the area of healthy tissue between the defect and the nasolabial fold (above) and/or between the defect and the vermillion border (below) is not sacrificed. Whenever possible, horizontal scars on the upper lip should be avoided, since they run contrary to the wrinkles and relaxed tension lines, resulting in a very poor cosmetic appearance. The simple maneuver of removing a small amount of neighboring healthy tissue makes it possible to hide curved scars in the nasolabial fold and the vermillion border and enables the scar to run into the natural wrinkles of the oral commissure. The medial scar, on the other hand, is vertical and runs parallel to the philtrum and wrinkles. In addition, this flap enables reconstruction with skin of the same characteristics as that removed; this is essential in men, as it ensures that hairy skin and, therefore, the appearance of the moustache, are maintained.
The flap used here is an advancement-rotation flap, which is easily designed and performed and enables the expression and appearance of the upper lip to be maintained and large defects to be closed.1 Similarly, the versatility of island flaps means that dermatological surgeons are generally comfortable performing them, since the design is useful in other areas of the face. Li et al.2 used the traditional island flap or variants thereof (e.g., the transposition island flap) in 80 patients with relatively large and deep defects on the nose, lip, and cheek, achieving favorable results in more than 90% of cases. Kimyai-Asadi and Goldberg3 review key aspects of the anatomy and vascularization of this flap and propose additional variants, also at other sites, such as tunneling, which we do not feel is a suitable option for the upper lip, since it can result in a marked trapdoor effect. However, various authors3–5 present images showing that in the case of the upper lip, not extending the defect towards the natural lines mentioned above can lead to horizontal scars in the middle of this anatomical subunit. The subtle difference observed by sacrificing adjacent healthy tissue in order to reach the borders of the upper lip, which is particularly easy in large defects,6 is fundamental.
Other options for reconstruction include the melolabial transposition flap, the cheek advancement flap, the subcutaneous tunneled pedicle flap, or transposition-advancement flaps from another area of the upper lip.7–9 These options are second choice owing to the distortion or loss of symmetry in the nasolabial fold, the fact that they do not spare aesthetic units, alteration of the moustache (men), or resulting trapdoor effect. However, they may be considered in large defects including the upper lip adjacent to the commissure when a subcutaneous island pedicle flap is impossible. Grafts should generally not be used at this site, since in addition to the unsatisfactory cosmetic effect, they carry a high risk of retraction that may hamper functionality in the area. Finally, in defects that, besides the upper lip, involve neighboring anatomical areas, the subcutaneous island pedicle flap can be combined with other flaps. Furthermore, the advancement-rotation flap can be designed from both sides (bilateral) in the case of large centrally located defects including the philtrum and the nasal vestibule.
ConclusionThe subcutaneous island pedicle flap enables simple reconstruction of many surgical defects affecting the upper lip where direct closure is not possible. Its functional and cosmetic outcomes are satisfactory, with preservation of the orbicular muscle. In addition, scars can be hidden in natural folds, with maintenance of symmetry in the nasolabial fold, philtrum, and lip.
Conflicts ofinterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Tomás-Velázquez A, Redondo P. Colgajo en isla del labio superior: claves fundamentales y serie de casos. Actas Dermosifiliogr. 2021;112:171–175.