Up to 30% of patients with psoriasis develop joint disease, the course of which can be improved by early diagnosis and treatment. The aim of this study was to describe our experience with a new multidisciplinary psoriasis and psoriatic arthritis unit over a period of 4 years (2009-2012).
Material and methodsImplementation of a PSOriasis Rheumatology and Dermatology unit (PSORD) to provide patient care and physician training. In the first phase of the project, referral criteria for the unit were defined and several meetings were organized to train and prepare the specialists involved in the program. In the second phase, a schedule was drawn up for monthly patient visits with the PSORD team. Starting in 2011, training was offered to dermatologists and rheumatologists from other hospitals interested in implementing a similar model.
ResultsA total of 259 visits (71% first visits, 8% no-shows) were scheduled during the period analyzed, with a median of 8 visits (range, 2-14 visits) per session. Sixty-three percent of the patients were referred from the rheumatology department. Diagnosis and treatment were modified in 32% and 47% of cases, respectively. Three training courses were held with 15 physicians from 6 hospitals, 3 of which created similar units.
ConclusionsThe PSORD model improved the management of difficult-to-diagnose and/or uncontrolled disease, the early diagnosis and treatment of psoriatic arthritis, and collaboration between dermatologists and rheumatologists. Finally, the model lends itself to being exported to other settings.
La afectación articular en los pacientes con psoriasis puede llegar hasta el 30%. El diagnóstico y tratamiento precoz de la artropatía puede influenciar su evolución. El objetivo de nuestro trabajo es describir la experiencia de la unidad multidisciplinar de psoriasis y artritis psoriásica de nuestro hospital en el periodo 2009-2012.
Material y métodosElaboración de un programa asistencial y docente. En una primera fase se consensuaron los criterios de derivación a la futura unidad y se realizaron varias reuniones conjuntas para formar y concienciar a los especialistas. En una segunda fase se estableció una agenda de visitas conjunta psoriasis-reumato-dermato (PSORD) con periodicidad mensual. A partir de 2011 se desarrolló un programa formativo abierto a dermatólogos y reumatólogos interesados en crear un modelo de colaboración similar.
ResultadosDurante el periodo revisado se han efectuado 259 visitas (71% primeras, 8% no presentados) con una media de 8 (2-14) visitas por sesión. El 63% de visitas eran derivaciones de reumatología. En un 32% de casos hubo algún cambio en el diagnóstico y en un 47% cambios en el tratamiento. También se han hecho 3 cursos con participación de 15 médicos de 6 hospitales, y en 3 de ellos se han creado unidades parecidas.
ConclusionesEste modelo ha comportado una mejora en el manejo de los pacientes que presentan problemas diagnósticos y/o de control de la enfermedad. También ha aumentado el diagnóstico precoz de la artritis y ha permitido indicar un tratamiento precoz. Además ha aumentado la colaboración entre ambas especialidades y el modelo creado se ha podido exportar a otros hospitales.
Psoriasis is considered a systemic disease that involves several organs, particularly the skin and the locomotor apparatus; it is often associated with various comorbid conditions.1–6 In most cases (70%-80%), skin lesions occur several years before joint involvement; consequently, the dermatologist plays a key role in early detection.7 Psoriatic arthritis (PsA) is a chronic, progressive disease that can become disabling and affects up to 30% of patients with psoriasis.8 Diagnosis of PsA is difficult in the early stages, even for the rheumatologist, and this difficulty is increased if the disease is not suspected or the physician is not aware of its characteristics. Early diagnosis and treatment are essential if joint damage and subsequent disability are to be prevented. In addition, early diagnosis obviates unnecessary examinations and risky treatment options, reduces costs, alleviates pain, and, therefore, improves the patient's quality of life.8,9 Approximately 10% to 29% of patients with psoriasis attended in the dermatology clinic are thought to have PsA. Since the disease is not suspected by the dermatologist, diagnosis may be delayed.10,11 Furthermore, skin involvement receives little or no attention in the rheumatology department, even though it may have a considerable impact on the patient's physical and psychological health, especially if suitable treatment is not intitiated.
Such a wider and more complex vision of the disease has gradually led to increased cooperation between the main specialists involved in the diagnosis and treatment of PsA. A multidisciplinary approach was recommended in the 2012 guidelines of the European League Against Rheumatism.12 Already in 2009, rheumatologists and dermatologists from Hospital Universitario Parc Taulí in Sabadell, Spain decided to create a cooperative model in the form of a multidisciplinary unit whose objective was to improve the management of patients with problematic psoriasis and PsA.
Materials and MethodsIn 2009, the multidisciplinary PSOriasis Rheumatology and Dermatology (PSORD) Unit was created at Hospital Universitario Parc Taulí for the general management of patients with problematic psoriasis.
The specific objectives of the unit were to facilitate early diagnosis of PsA in patients with psoriasis, improve management of patients with psoriasis and PsA, and boost cooperation between the rheumatology department and the dermatology department at the hospital.
Before the unit could be implemented, both departments had to have sufficient specialists with experience and interest in psoriatic disease. It was also necessary to encourage interest in diagnostic suspicion and referral of patients to rheumatology by dermatologists.
A database was designed for collection of information on the patient, disease, and treatment, as well as the name of the physician who referred the patient and the reason for referral. The present work presents the results of a partial analysis of the database.
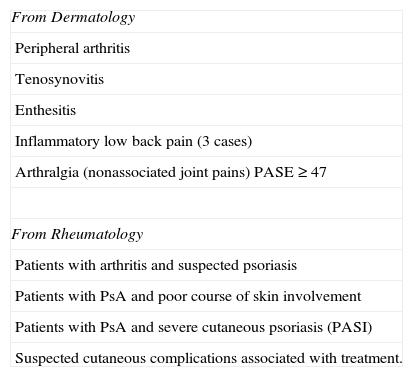
Care ProgramThe care program comprised 2 stages. In the first stage, training involved providing rheumatologists and dermatologists with a general vision of psoriasis, thus highlighting the need for cooperation between both specialties. Project leaders were appointed (1 rheumatologist and 1 dermatologist), and 2 joint training sessions were held during a 3-month period. All the members of both sections were present. At the training sessions, the nature of the disease was presented from the perspective of both groups, with emphasis on the signs and symptoms that raise suspicion of psoriasis and PsA. The sessions resulted in a consensus on the criteria for referral from the dermatology and rheumatology departments to the multidisciplinary unit (Table 1). The criteria were not applied for the management of all patients with psoriasis and/or PsA, only those with a diagnostic or treatment problem that was covered by the primary objective of this project. In the second stage, a joint monthly 3-hour visit schedule was prepared. All patients referred to the PSORD unit were visited jointly by a rheumatologist and a dermatologist, who made the appropriate decisions on diagnosis and treatment. PsA was diagnosed by the rheumatologist based on the classification criteria for psoriatic arthritis proposed by Taylor et al.13 Psoriasis was diagnosed based on characteristic signs and always according to the criteria of the dermatologist. Additional tests (eg, biopsy and culture) were ordered in cases of diagnostic uncertainty. Visits were made in the dermatology section in order to take advantage of infrastructure (clinics and specialized nursing staff). Once patients were seen in the PSORD unit and their problem resolved, they returned to the reference specialist for standard follow-up.
Criteria for Referral of Patients to the Psoriasis Rheumatology and Dermatology Unit According to the Source Unit.
| From Dermatology |
| Peripheral arthritis |
| Tenosynovitis |
| Enthesitis |
| Inflammatory low back pain (3 cases) |
| Arthralgia (nonassociated joint pains) PASE≥47 |
| From Rheumatology |
| Patients with arthritis and suspected psoriasis |
| Patients with PsA and poor course of skin involvement |
| Patients with PsA and severe cutaneous psoriasis (PASI) |
| Suspected cutaneous complications associated with treatment. |
Abbreviations: PASE, Psoriatic Arthritis Screening Evaluation; PASI, Psoriasis Area Severity Index; PsA, psoriatic arthritis.
In 2011, our experience led us to develop a certified training program, which was extended to colleagues interested in implementing a similar model at their institutions. The program comprised 2 parts: a 6-hour theory module in which the main aspects of psoriasis and PsA were reviewed from the perspective of the dermatologist and rheumatologist and the referral criteria and logistic structure necessary for implementation of a PSORD unit are taught; and a practical session held the following morning involving a routine visit to the PSORD unit.
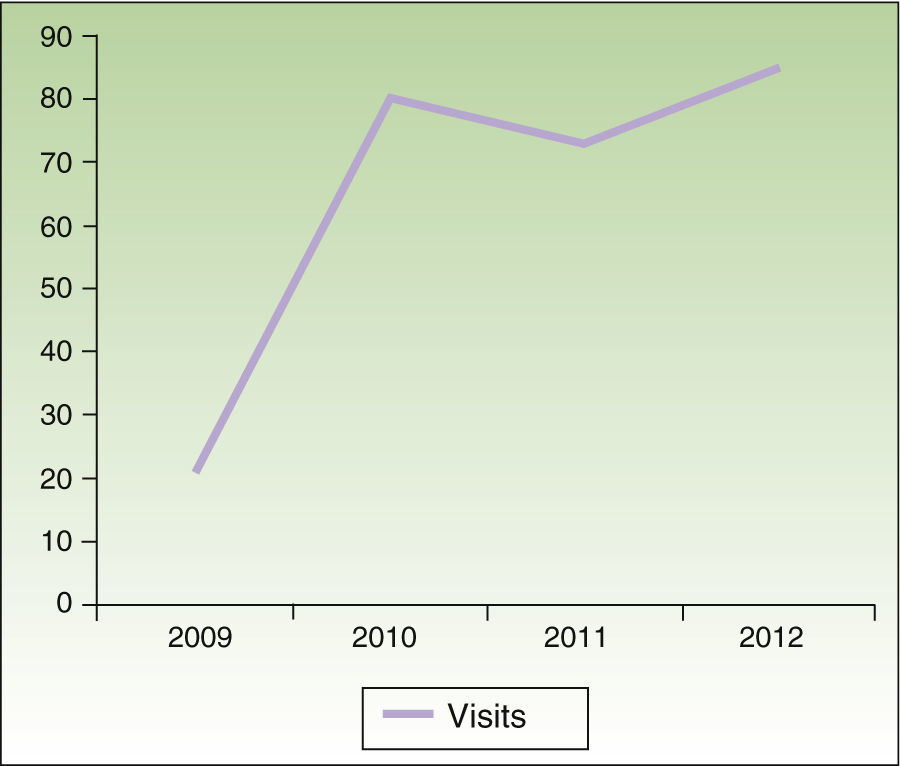
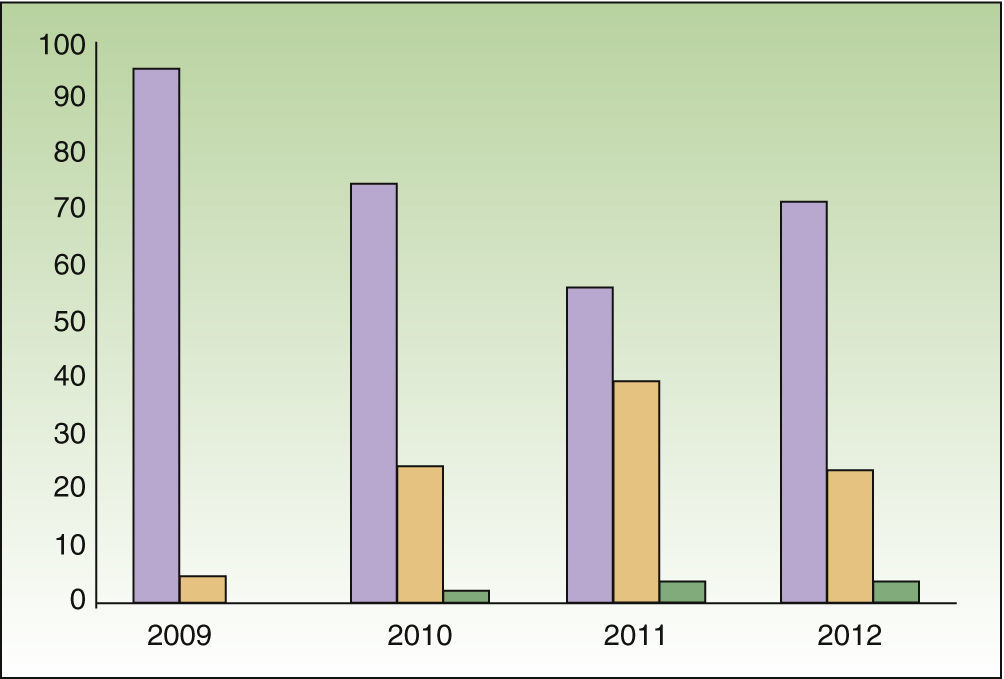
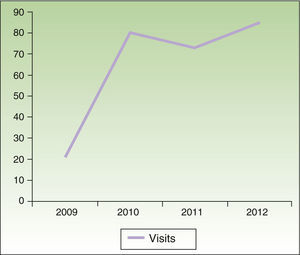
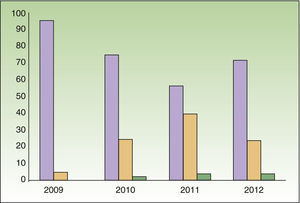
ResultsFrom 2009 to 2012, the unit received 184 patients (89 men and 95 women) who generated 259 visits. All the patients seen under the protocol were from the rheumatology and dermatology departments. A mean of 8 (2-14) visits per session was recorded. First visits accounted for 71% of the total; consecutive visits accounted for 21%, of which 5% were consecutive. Nonattendance at the scheduled visit was 8%. The number of visits increased significantly between 2009 and 2010 before leveling off at around 80 visits per year (Fig. 1). Although the number of consecutive visits increased over time, the ratio of first visits to consecutive visits settled at 7:3 (Fig. 2).
A total of 114 cases (63%) were referred from the rheumatology department, compared with 68 (37%) from the dermatology department; this proportion remained stable throughout the study period.
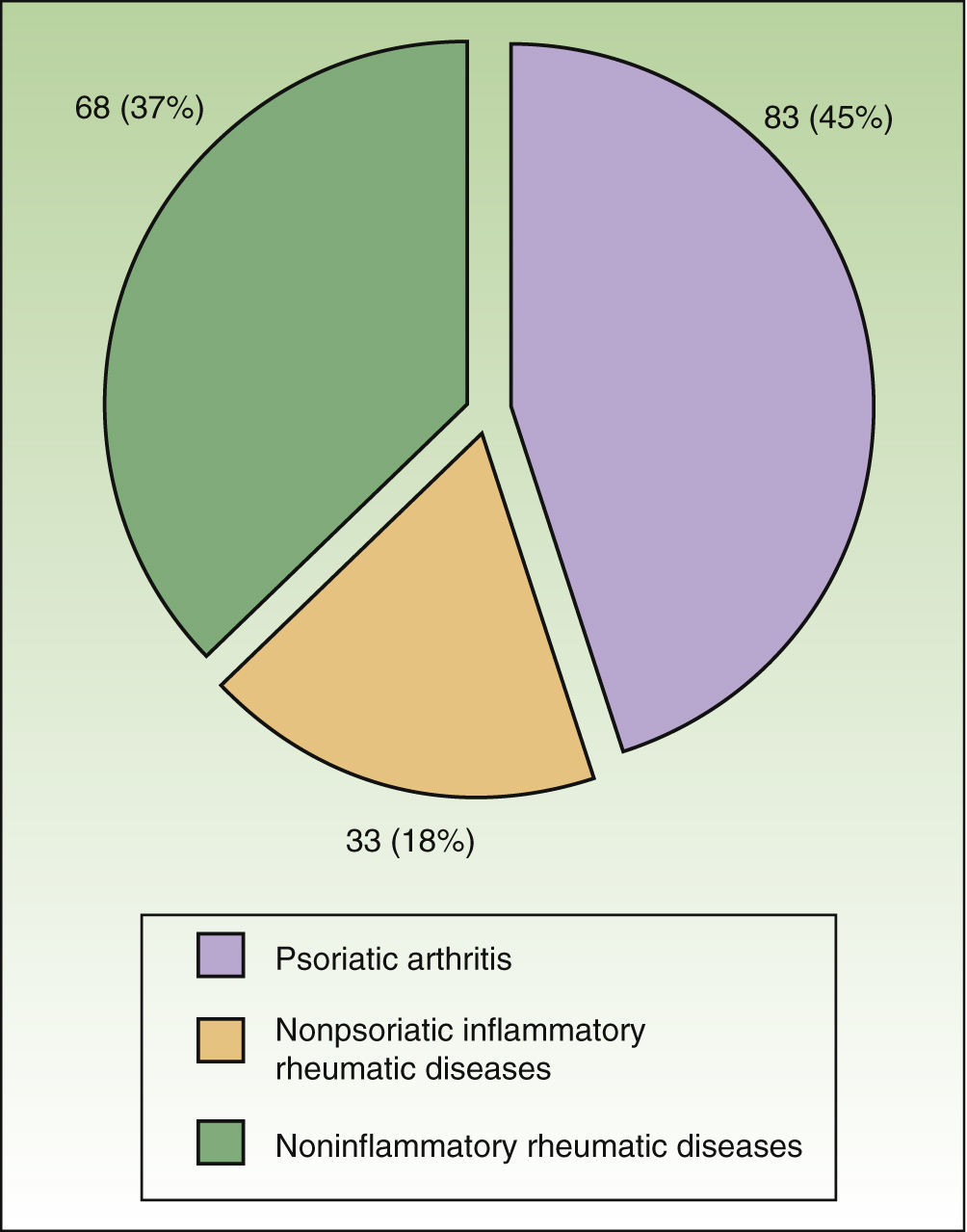
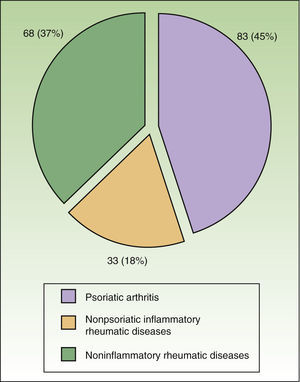
The presenting complaint was psoriasis of the skin and nails in 72% of cases (132/184). A definitive diagnosis of PsA was made in 45% of patients (83/184) and the disease was considered de novo in 44 cases (24%). In 18% of cases the diagnosis was nonpsoriatic inflammatory rheumatic disease (gout, connective tissue disease, and rheumatoid arthritis); in 37% the diagnosis was noninflammatory disease of the locomotor apparatus (arthrosis and nonspecific pain of the locomotor apparatus) (Fig. 3).
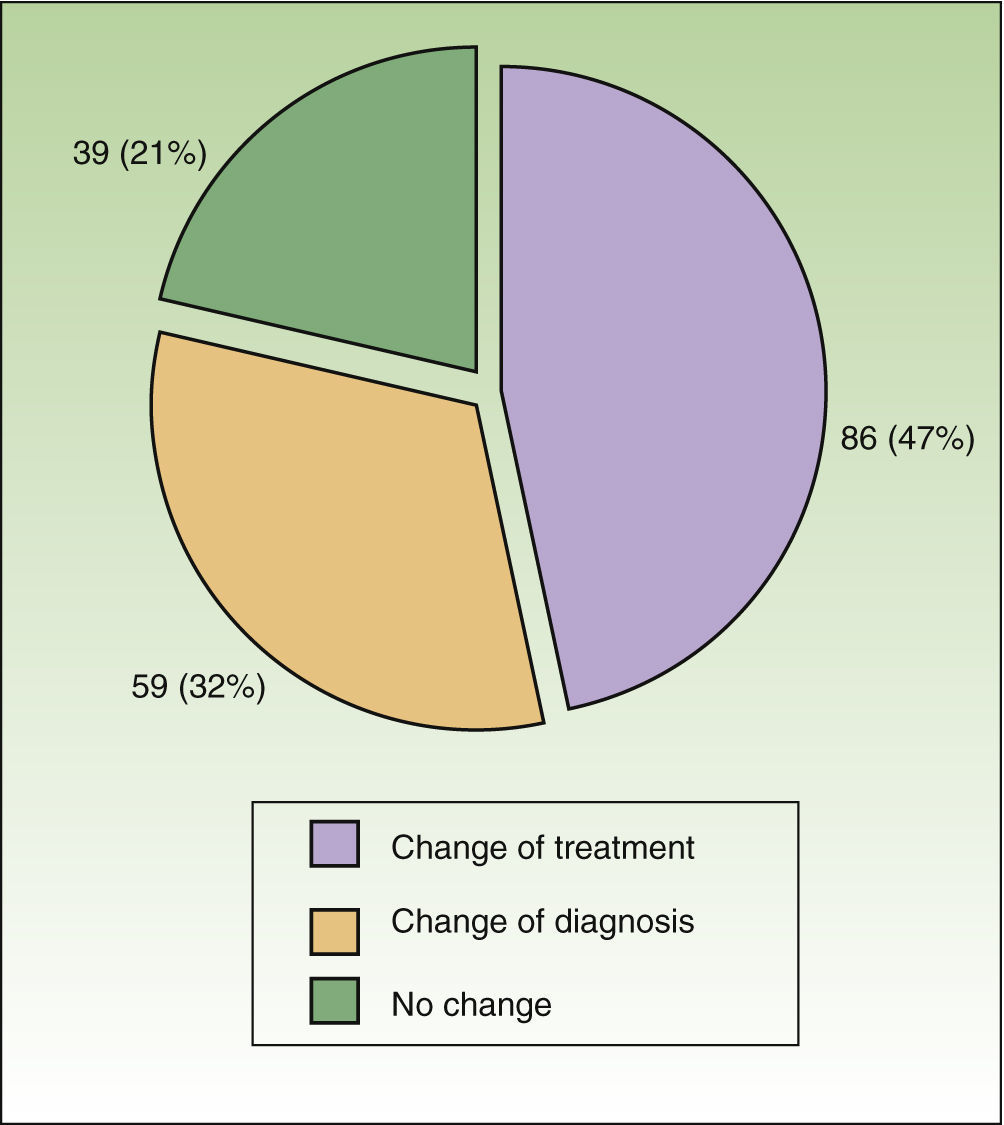
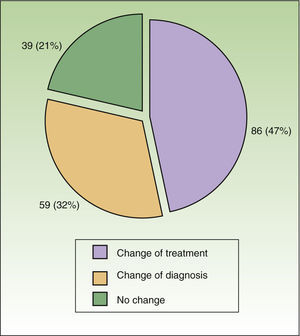
The reason for referral was suspected PsA in 106 cases (59%); the diagnosis was confirmed in 66% of these cases. The referral was for a problem with therapy in 41% of cases. The diagnosis was modified in 32% of cases; treatment was modified in 47% of cases, but not in 21% (39 cases) (Fig. 4). Diagnostic agreement was 40% both for suspicion of PsA by the dermatologist and for suspicion of psoriasis of the skin and/or nails by the rheumatologist. Of note, agreement was low for suspicion of psoriasis by the rheumatologist based on nail lesions (<20%) and for suspicion of PsA by the dermatologist based on arthralgia and osteomuscular pain (25%). In the latter, less than 5% of referrals were based on the result of the Psoriatic Arthritis Screening Evaluation (PASE).
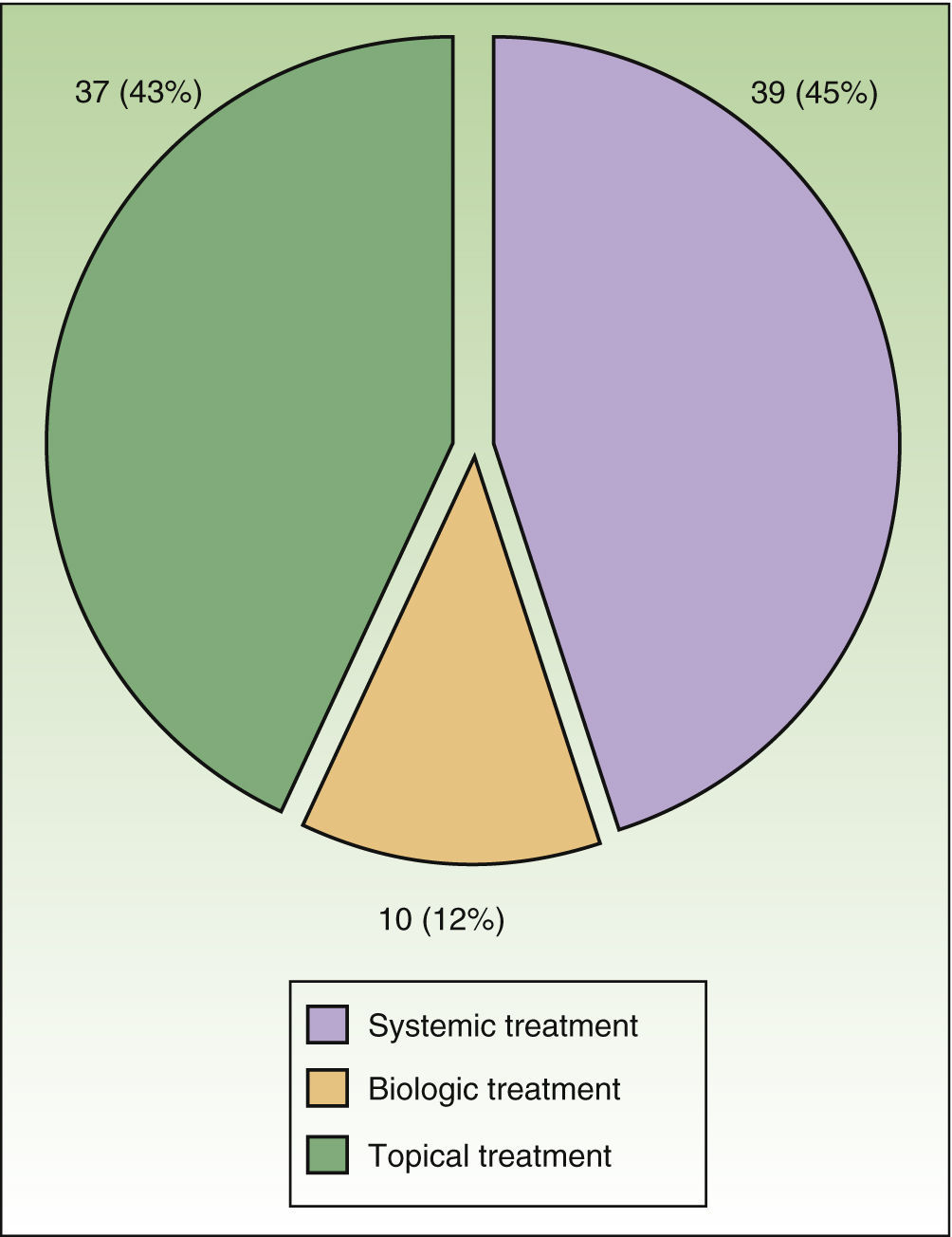
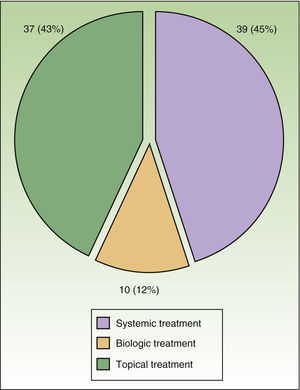
Of the 86 cases in which therapy was switched, 45% involved a modification to systemic therapy, ie, addition of a new disease-modifying antirheumatic drug in 30%. Methotrexate was the most commonly used. Finally, in 12% of cases the drug was switched or a new biologic was added (Fig. 5).
Results of the Training ProgramTwo training courses were held with 10 rheumatologists from 5 Spanish hospitals during 2011 and 2012. To date, PSORD units similar to ours have been implemented at 2 of these centers (Hospital Can Mises in Ibiza and Hospital de Basurto in Bilbao).
DiscussionWe present our experience with a multidisciplinary psoriasis unit at Hospital Universitario Parc Taulí during the period 2009-2012. In this care model, the patient is seen jointly by a rheumatologist and a dermatologist. The model has enabled a major improvement in the management of patients with psoriasis whose diagnosis and treatment are problematic and has facilitated early diagnosis and treatment of PsA, with all the advantages this entails for disease control. The model has also enabled the implementation of a training program, which in turn led to the implementation of 2 similar units at other centers. Finally, implementation of our PSORD unit has improved cooperation between dermatologists and rheumatologists, and it is hoped that similar joint research projects will be developed in the future.
The first of its kind in Spain, our model follows the current guidelines of the European League Against Rheumatism.14 The only previous report of joint visits by rheumatologists and dermatologists was from the Center for Skin and Related Musculoskeletal Diseases (SARM) at Brigham and Women's Hospital in Boston, Massachusetts, USA.15 In their 2007 pilot study, the authors reported results for 94 patients seen at their unit over a 1-year period16; however, the first retrospective review (6-year results for 510 patients) was not performed until 2012.17 Other formally structured initiatives similar to ours have also been implemented. These include the project by Drs. Diamant Thaçi and Frank Behrens from the Goethe University of Frankfurt, Germany (Thaçi D, Behrens F. Psoriatic arthritis: Multidisciplinary units experience. Shedding light on psoriatic arthritis and psoriasis. Rheumatologists and dermatologists: two perspectives. Madrid, February 1-2 2013), although the results of their experience have not been published. The existence of structured models of joint visits by dermatologists and rheumatologists, such as that of the SARM and ours, mean that unofficial contact between both specialties can make it possible to systematize consultations, collect and analyze activity data, and, in particular, strengthen cooperation through design of criteria and patient management protocols. Consequently, both the PSORD and the SARM are examples of structured cooperation. However, our model differs considerably from that of the SARM: whereas SARM provides an integral service with its own management unit, the PSORD is a joint visit model that uses existing resources. We decided to implement this model because it was not feasible to create an independent service in our National Health System.
Unlike the SARM, in which patients could be referred from areas other than rheumatology and dermatology (eg, orthopedics and primary care), patients in our model were only referred from dermatology and rheumatology, since the PSORD unit was not an independent department. Although this might initially appear to be a weakness of our model, it does favor implementation of joint training and awareness programs on early diagnosis of complications, including the suspected diagnosis of PsA by dermatologists. This skill in particular is of special interest, since cutaneous psoriasis precedes onset of arthritis in 75% of cases. Furthermore, given that no correlation has been established between the severity of psoriasis and the presence of arthritis and no specific diagnostic test has been developed for PsA, it is difficult for dermatologists to suspect this disease.18,19 Therefore, we believe that it is very important for experienced dermatologists with particular interest in psoriasis to participate in joint training programs aimed at encouraging recognition of the principal symptoms and signs so that they can suspect a diagnosis of PsA. Nevertheless, the percentage of patients in our series referred from the dermatology department (37%) was lower than expected and reported elsewhere15; unfortunately, this percentage has not increased during the time the unit has been in operation. Although we can offer no clear explanation for this observation, it is somewhat easier to refer a patient with arthritis (rheumatology) and skin lesions than to suspect PsA in a patient with cutaneous psoriasis. This observation could go some way to explaining our findings. Consequently, it is necessary to periodically repeat joint training sessions in order to ensure that dermatologists are aware of PsA and that they regularly suspect and attempt to identify the disease in patients with psoriasis.
The joint training sessions should also serve to set consensus criteria for referral both from the dermatology department and from the rheumatology department to the appropriate unit. Although this was the approach we adopted, diagnostic agreement in our model was only moderate (40%), with excessive referral from dermatology because of nonspecific osteomuscular pain for which diagnostic agreement was low (25%). Several validated screening tests (PASE, Psoriasis Epidemiology Screening Tool, Toronto Psoriatic Arthritis Screen) can be applied to improve the outcome of referral in these situations,20,21 although their use in clinical practice has recently been shown to be less effective than previously thought.22 In our model, the PASE was recommended in one of the referral criteria (polyarthralgia), although it was not obligatory, which meant that it was used in fewer than 5% of cases, depending on the interest of the clinician in question. Given the results obtained, mandatory implementation could prove interesting in certain circumstances (suspicion of PsA based on polyarthralgia). As for referrals from rheumatology, a key problem is the suspected diagnosis of PsA based on lesions of the nails; in this area in particular, only one-quarter of our diagnoses were correct. This finding is not surprising, since nail disease is a key diagnostic challenge, even for the dermatologist. Although lesions of the nail are accurately described, thus facilitating the diagnosis of psoriatic nail disorders, the lack of specificity with respect to these lesions creates a veritable diagnostic challenge and an extremely interesting field for future study in both specialties.23,24
The number of first visits in our model, which remained stable throughout the study period, is much higher than that published by the SARM. Furthermore, and in contrast with the SARM, all the patients referred to our unit returned to their specialist for continued regular follow-up once the reason for referral was established. The joint care model we propose acts as a support unit to improve management of problematic patients. It is not intended as a parallel service for routine follow-up, nor does it aim to monopolize treatment, since this would lead to duplicate visits and conflicts of interest between specialists. The model could also lead to fewer referrals, thus diminishing the quality of care provided to the patient.
Our PSORD unit has had a significant impact on patient management, since diagnosis and/or therapy remained unchanged in only 21% of cases after referral to our unit. The most frequent diagnosis during follow-up was cutaneous psoriasis (71% of cases). A concomitant diagnosis of PsA was established in 45% of cases and, most importantly, the PsA was de novo in more than half of the cases. This finding is especially relevant, since it shows that a diagnosis of de novo PsA was established in 44 referred patients thanks to the diagnostic suspicion of the dermatologist. Given that early diagnosis7,18 and the possible effect of treatment on disease progression during these phases25 are key challenges in PsA, we believe that the data on new diagnoses of PsA alone would justify the existence of our unit. Furthermore, it is noteworthy that in 47% of cases, referral to our unit led to a change in therapy. In more than half of the cases, this change led to modifications in systemic therapy; specifically, in 30% of cases it meant addition of a new disease-modifying antirheumatic drug, the most commonly used being methotrexate. The most frequent reason for changing the dose and/or adding a new systemic drug was concomitant detection of PsA. These findings are consistent with those published by the SARM group17 and support the usefulness of these units for improved management of problem patients with psoriatic disease.
In 12% of cases, referral to our unit led to modification of biologic therapy (addition or discontinuation). The most common reason for the change was to improve management of skin and nail lesions in psoriasis, although in 2 cases therapy was modified owing to poorly controlled PsA. While this number may not seem very relevant, it is very significant if we remember that ours is not a unit where biologic therapy is prescribed, yet a change in biologic therapy was made.
Eight percent of patients did not attend their visits. In our experience, this figure is very low, perhaps because the average time to the visit was less than 1 month. This finding should be borne in mind when evaluating the quality of our model, especially in the case of problematic patients.
We present the experience of a single center; however, the fact that almost half of the rheumatologist from the other centers that participated in the training program were able to implement similar units in their hospitals shows that the model could be applied in various real-life clinical situations. Previous editions of the courses were attended only by rheumatologists. Our experience seems to indicate that future editions would benefit from the joint participation of rheumatologists and dermatologists from centers interested in implementing a similar model. This would no doubt facilitate development and increase the number of centers able to implement the model.
Although the PSORD unit was designed as a consultation-investigation-diagnosis unit to provide support to specialist colleagues in the management of problematic patients with psoriasis and PsA, the model has greatly improved cooperation between both specialties and has enabled several joint projects to be developed. The present work is the first report on this cooperation.
One of the limitations of this study is that it is based on the experience of a single center. Our experience should be confirmed and compared with that of other centers of this type, although the lack of publications on similar projects has made such a comparison impossible.
The low rate of referral from the dermatology department could mean that the rate of early diagnosis of PsA is lower than desired. Given that one of the main benefits stemming from the implementation of the unit was that it facilitated early diagnosis of PsA, we believe that the model should be revised and that we should concentrate more on dermatologists and on improving training in this group.
Our study is also limited by the fact that the monitoring of activity at our unit does not include clinical variables, comorbid conditions, follow-up, treatment, or patient progress. Nevertheless, our primary objective was to be a consultation-investigation-diagnosis unit providing support in the management of problematic patients for specialist colleagues from hospitals with a high caseload, not a parallel unit or service for attending and following patients with PsA. The project benefited considerably from the cooperation between both specialties and has made it possible to implement a training program and encourage cooperation in various ongoing scientific projects. Ours is not a closed model. On the contrary, taking into account the specific aspects of each center, it could serve as a basis for cooperative models that involve, to a greater or lesser extent, follow-up of patients with PsA.
In conclusion, implementation of a multidisciplinary unit comprising rheumatologists and dermatologists who are experts in the management of PsA is consistent with the main guidelines on management of psoriasis. Our unit served as a support for specialists attending patients with psoriasis for whom diagnosis and treatment were problematic. Finally, the project has led to improved cooperation between the dermatologist and the rheumatologist, thus enabling the implementation of a training program and the development of several joint projects, of which the present work is the first example.
Ethical DisclosuresProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe participating authors declare that they have received support and fees for research, consultancy, and training from the following companies: Abbvie, Janssen, MSD, Novartis, and Pfizer.
The training courses stemming from this project were supported by Pfizer.
Please cite this article as: Luelmo J, Gratacos J, Moreno Martínez-Losa M, Ribera M, Romaní J, Calvet J, et al. Experiencia de 4 años de funcionamiento de una unidad multidisciplinar de psoriasis y artritis psoriásica. Actas Dermosifiliogr. 2014;105:371–377.
De acuerdo con los autores y los editores este artículo se publica simultáneamente y de forma íntegra en la revista Reumatología Clínica http://dx.doi.org/10.1016/j.reuma.2014.01.004.