A 59-year-old man with type 2 diabetes mellitus who had experienced myocardial infarction 2 years earlier was seen for asymptomatic, generalized, somewhat photodistributed skin lesions that had appeared 1 year earlier and had not responded to topical corticosteroids. The patient was a nonsmoker and was taking daily fenofibrate, aspirin, acenocoumarol, metformin, pantoprazole, folic acid, and bisoprolol. He ruled out any connection between the dermatosis and his work, as the lesions persisted after he left his job as a plasterer.
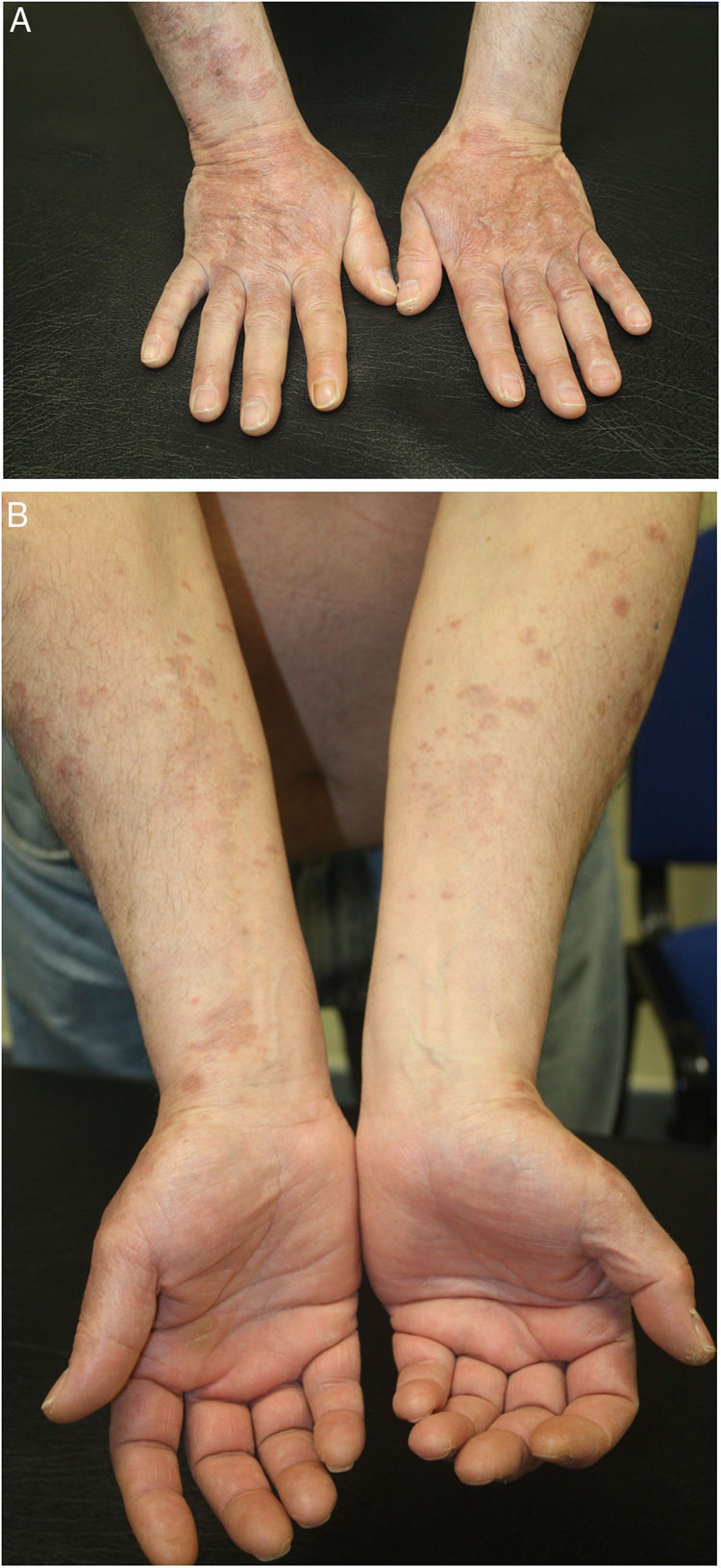
The dermatological examination revealed annular erythematous and violaceous papules with raised borders that clustered to form plaques on the back of the hands (Fig. 1A).
Clinical presentation of the patient. A, Brownish, arciform, erythematous plaques with a tendency to coalesce on the backs of the hands and the dorsal aspect of the forearms. The lesions were mildly infiltrated and lacked an appreciable epidermal component. B, The lesions extended to the volar aspect of the forearms, where they were milder and coalesced less.
Smaller, isolated, light pink annular lesions (approximately 3–4 mm) were present on both arms (Fig. 1B).
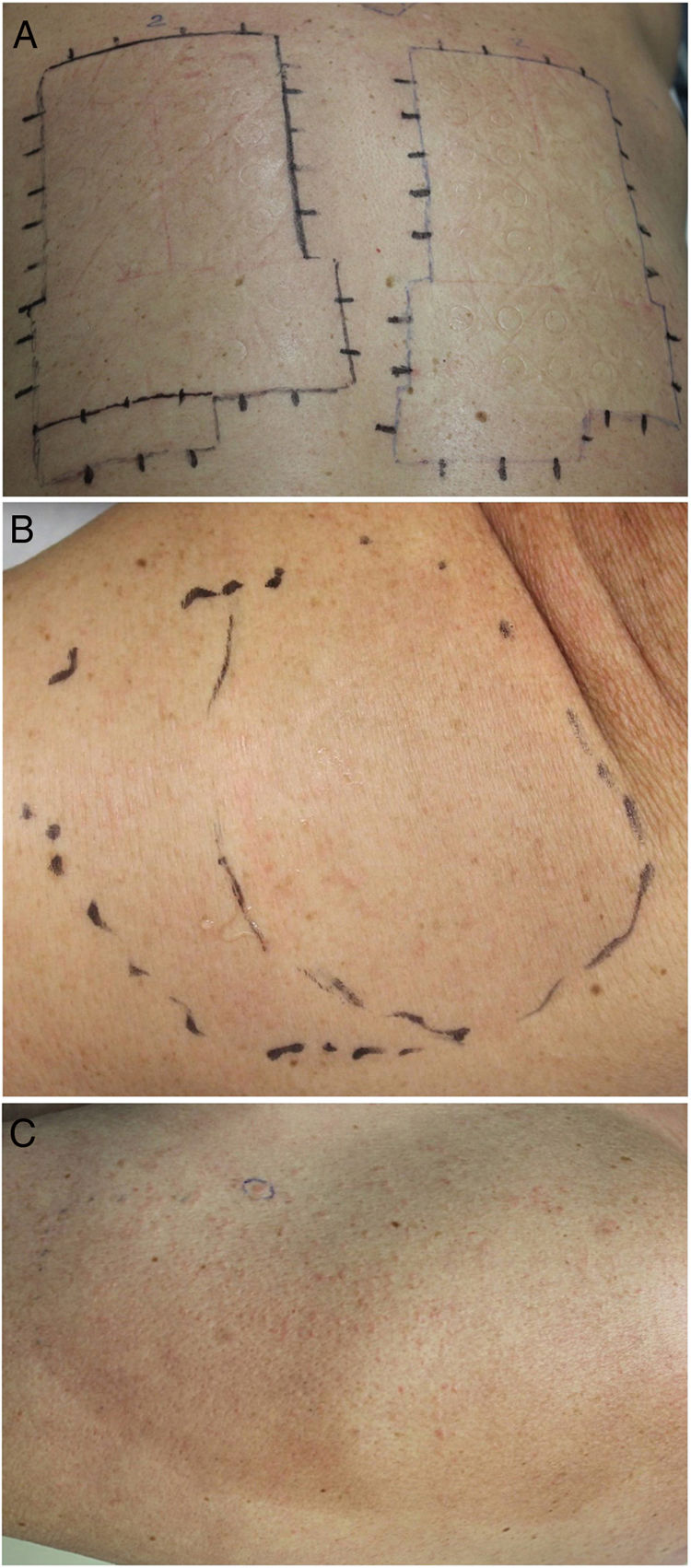
A phototest was performed using different light sources. A reading was taken immediately to determine the minimum urticarial dose and again after 24 hours to determine the minimum erythematic dose. Photoprovocation and photopatch tests were also performed. The immediate phototest reading revealed a normal response to both ultraviolet (UV) A and UVB light. After 24 hours the values obtained for the minimum erythematic dose were as expected for the patient’s phototype (31 mJ/cm2), and the response to UVA was normal. Double reading of photopatch tests (non-irradiated and UVA-irradiated [13.32 J/cm2] patches) after exposure to the standard battery, together with the drugs that the patient took habitually, revealed no reaction indicative of exogenous skin photosensitivity at either 24 or 48 hours after irradiation (Fig. 2A).
Photobiological study of the patient. A, Photopatch reading at 48 hours. The photopatches on the left were irradiated with UVA for 6 minutes using a Philips® HB 404 high pressure lamp (13.32 J/cm2). The patches on the right were not irradiated. No contact or photo-contact reactions were observed for the standard battery or for the drugs that the patient had been prescribed. Results were also negative after 96 hours. B, Photoprovocation on day 1 of irradiation (7 min; 15.54 J/cm2). The photoprovoked region consisted of an area directly irradiated with UVA (left) and an area covered with a water-filled Petri dish (right) to eliminate the infrared (IR) component. C, Photoprovocation at 144 hours. Isolated minute micropapules are evident on the left side of the irradiated area. Some of the lesions near the edge are larger. Milder lesions are also evident in the area protected from IR radiation.
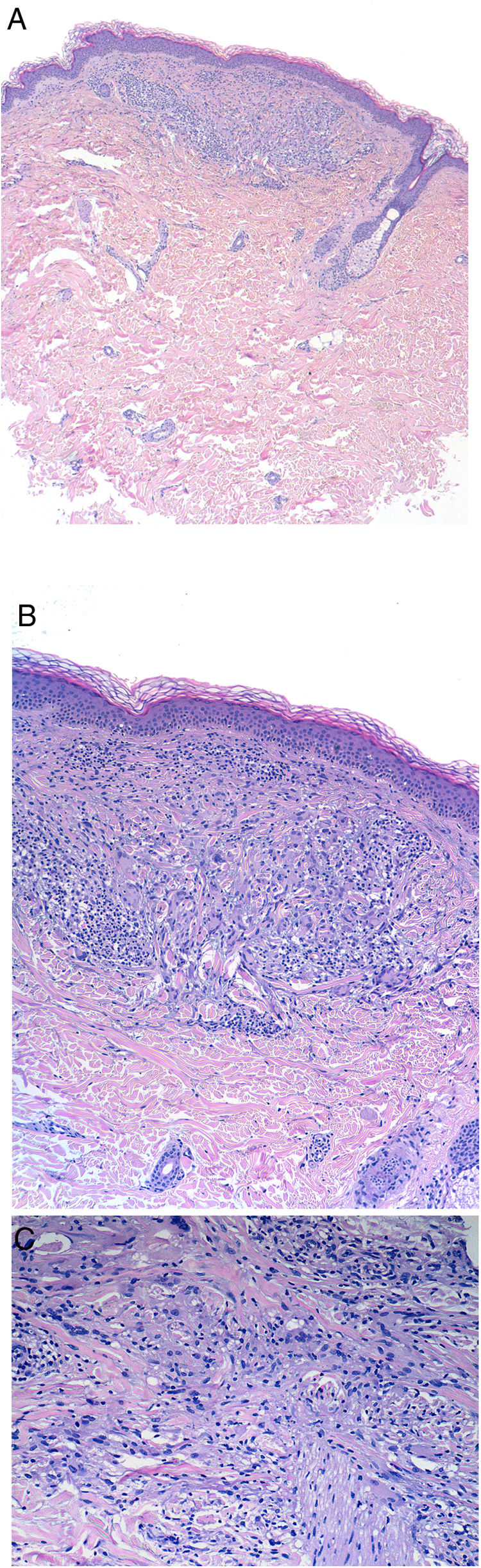
In a photoprovocation test, UVB irradiation of the back and shoulder had no effect, while UVA irradiation (24.42 J/cm2; Fig. 2B) resulted in the appearance of some micropapules and erythema after 48 hours. The lesions reappeared on the following days of the photoprovocation test, up until day 6 (cumulative dose, 97.71 J/cm2). Based on this finding, a skin biopsy of the newly formed lesions and the pre-existing papules was performed. Histology of the biopsies revealed numerous histiocytes and multinucleated giant cells distributed interstitially in the papillary and reticular dermis (Fig. 3A and B). No phagocytosis of elastic fibers was observed in interstitial macrophages (Fig. 3C). Based on the clinical and histopathologic findings, the patient was diagnosed with UVA-photoinduced granuloma annulare (GA).
Histology of newly formed papules after photoprovocation. A, Well-circumscribed interstitial dermal infiltrate. At low magnification, neither granulomas nor epidermal involvement are observed (hematoxylin-eosin [HE] ×2, original magnification ×20). A higher magnification image reveals lymphohistiocytic infiltrate containing an important component of large cytoplasmic cells surrounding collagen bundles to create an interstitial granulomatous dermatitis pattern (HE ×10, original magnification ×100). C, High magnification image in which elastophagocytosis is not observed, ruling out a diagnosis of actinic granuloma (HE ×20, original magnification ×200).
GA is a benign and self-limiting inflammatory dermatosis of uncertain origin.1,2 It is characterized by the presence of dermal papules with no appreciable epidermal component and a tendency to coalesce to form mainly asymptomatic arcuate or annular plaques.1,3 The specific etiology of GA is unknown, although it has been linked to a multitude of comorbidities, including malignant neoplasms,3 viral infections, and drug treatment.2 Although most resolve spontaneously, even after biopsy, some lesions can leave permanent scars.4
Disseminated GA has been more specifically related to systemic conditions such as diabetes mellitus1,5 and, in rare cases, sun exposure.6 Actinic granuloma, described by O’Brien, is characterized by the presence in photo-exposed areas of lesions that are suggestive of GA7 but exhibit degeneration of elastic fibers, which are phagocytosed by histiocytes present in the infiltrate (elastophagocytosis).8
There are few published cases of GA induced by light radiation.4,9,10 According to some studies, solar radiation is considered one of the potential causes of GA. Attempts have been made to reproduce GA lesions using ultraviolet light, without success.1 We believe that this is the first reported case of photoinduced granuloma annulare in experimental conditions in the context of a photobiological study. There are some published descriptions of photoinduced GA in patients taking medication, such as paroxetine.10 However, in our patient the results of photopatch tests ruled out a pharmacological etiology. Despite the absence of medication, we believe that in our case a preformed antigen may have undergone a conformational change upon exposure to UVA, triggering GA-like granulomatous dermatitis.
Treatment of this entity is often unsatisfactory. Various treatment options have been used, including oral retinoids, antimalarials, and phototherapy.5,9 Our patient was recommended exhaustive topical photoprotection with a high sun protection index, including UVA and infrared photoprotection, as well as oral photoprotection. After 9 months of follow-up, the patient has not presented any new lesions and all existing lesions have stabilized.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fonda-Pascual P, de Gálvez MV, Aguilera J, Herrera-Ceballos E. Granuloma anular fotoinducido demostrado experimentalmente mediante fotoprovocación UVA. Actas Dermosifiliogr. 2021;112:190–192.



![Histology of newly formed papules after photoprovocation. A, Well-circumscribed interstitial dermal infiltrate. At low magnification, neither granulomas nor epidermal involvement are observed (hematoxylin-eosin [HE] ×2, original magnification ×20). A higher magnification image reveals lymphohistiocytic infiltrate containing an important component of large cytoplasmic cells surrounding collagen bundles to create an interstitial granulomatous dermatitis pattern (HE ×10, original magnification ×100). C, High magnification image in which elastophagocytosis is not observed, ruling out a diagnosis of actinic granuloma (HE ×20, original magnification ×200). Histology of newly formed papules after photoprovocation. A, Well-circumscribed interstitial dermal infiltrate. At low magnification, neither granulomas nor epidermal involvement are observed (hematoxylin-eosin [HE] ×2, original magnification ×20). A higher magnification image reveals lymphohistiocytic infiltrate containing an important component of large cytoplasmic cells surrounding collagen bundles to create an interstitial granulomatous dermatitis pattern (HE ×10, original magnification ×100). C, High magnification image in which elastophagocytosis is not observed, ruling out a diagnosis of actinic granuloma (HE ×20, original magnification ×200).](https://static.elsevier.es/multimedia/15782190/0000011200000002/v1_202102100758/S157821902030398X/v1_202102100758/en/main.assets/thumbnail/gr3.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)



