Marginal zone B-cell lymphoma (MZL) is subclassified into extranodal MZL of mucosa-associated lymphoid tissue (including cutaneous lymphomas), splenic MZL, and nodal MZL. We report the case of a 68-year-old man with erythematous-violaceous plaques and nodules. Skin biopsy showed an epidermotropic lymphocytic infiltration and cytology and immunohistochemistry were consistent with MZL. The workup revealed disease in the peripheral blood and bone marrow and massive splenomegaly. Splenectomy confirmed the diagnosis of splenic MZL and led to resolution of the skin lesions. Cutaneous recurrence was treated successfully with chemotherapy and rituximab but caused fatal hepatitis due to hepatitis B virus reactivation. Skin involvement by splenic MZL is uncommon; this form of the disease can present epidermotropism, a very rare finding in primary cutaneous MZL. Treatment consists of splenectomy, which may be associated with chemotherapy and/or rituximab; this treatment may lead to reactivation of latent hepatitis B infection and screening for hepatitis should therefore be performed prior to starting therapy.
El linfoma B de la zona marginal (LZM) se subdivide en LZM extraganglionar tipo MALT (incluye los cutáneos), esplénico y ganglionar. Presentamos el caso de un varón de 68 años con placas y nódulos eritematovioláceos. La biopsia cutánea mostró una infiltración linfocitaria epidermotropa con citología e inmunohistoquímica compatibles con LZM. El estudio de extensión mostró afectación de sangre periférica, médula ósea y esplenomegalia masiva. La esplenectomía confirmó el diagnóstico de LZM esplénico con desaparición de las lesiones cutáneas. Tras la recidiva cutánea se instauró quimioterapia/rituximab con desaparición de la misma, pero produciéndose una hepatitis letal por reactivación de virus de hepatitis B. La afectación cutánea por un LZM esplénico es un hallazgo infrecuente. Dicha afectación puede presentar epidermotropismo, hallazgo excepcional en los LZM cutáneos primarios. El tratamiento consiste en esplenectomía y/o quimioterapia y/o rituximab que pueden reactivar una hepatitis B inactiva, por lo que es preciso el screening de hepatitis antes de iniciarlos.
Marginal-zone B-cell lymphoma (MZL) is a neoplasm that originates in lymphocytes of the marginal zone, which is a compartment of lymphoid follicles that is highly developed in lymphoid organs with a high influx of antigens. The World Health Organization classification subdivides MZL into mucosa-associated lymphoid tissue (MALT) lymphoma and splenic or nodal lymphoma.1 The etiopathogenic process has been linked to chronic antigenic stimulus by self-antigens or bacteria such as Borrelia burgdorferi (cutaneous MZL) and Helicobacter pylori (gastric MZL) and viruses such as hepatitis C (splenic MZL). Although the clinical behavior of these different types of lymphoma may differ, they share similar morphologic features and have a similar immunophenotype: CD19+, CD20+, CD79a+, CD5-, CD10-, CD23-, bcl6-, and bcl2+. More than 70% of MZL, including the primary cutaneous forms, are of the MALT type, whereas splenic and nodal forms occur less frequently and account for only 1% of non-Hodgkin lymphomas. With MALT lymphoma and nodal MZL, there have been reports of cutaneous involvement,2 but this is rare in the case of splenic MZL. We present a case of splenic MZL with epidermotropic skin involvement.
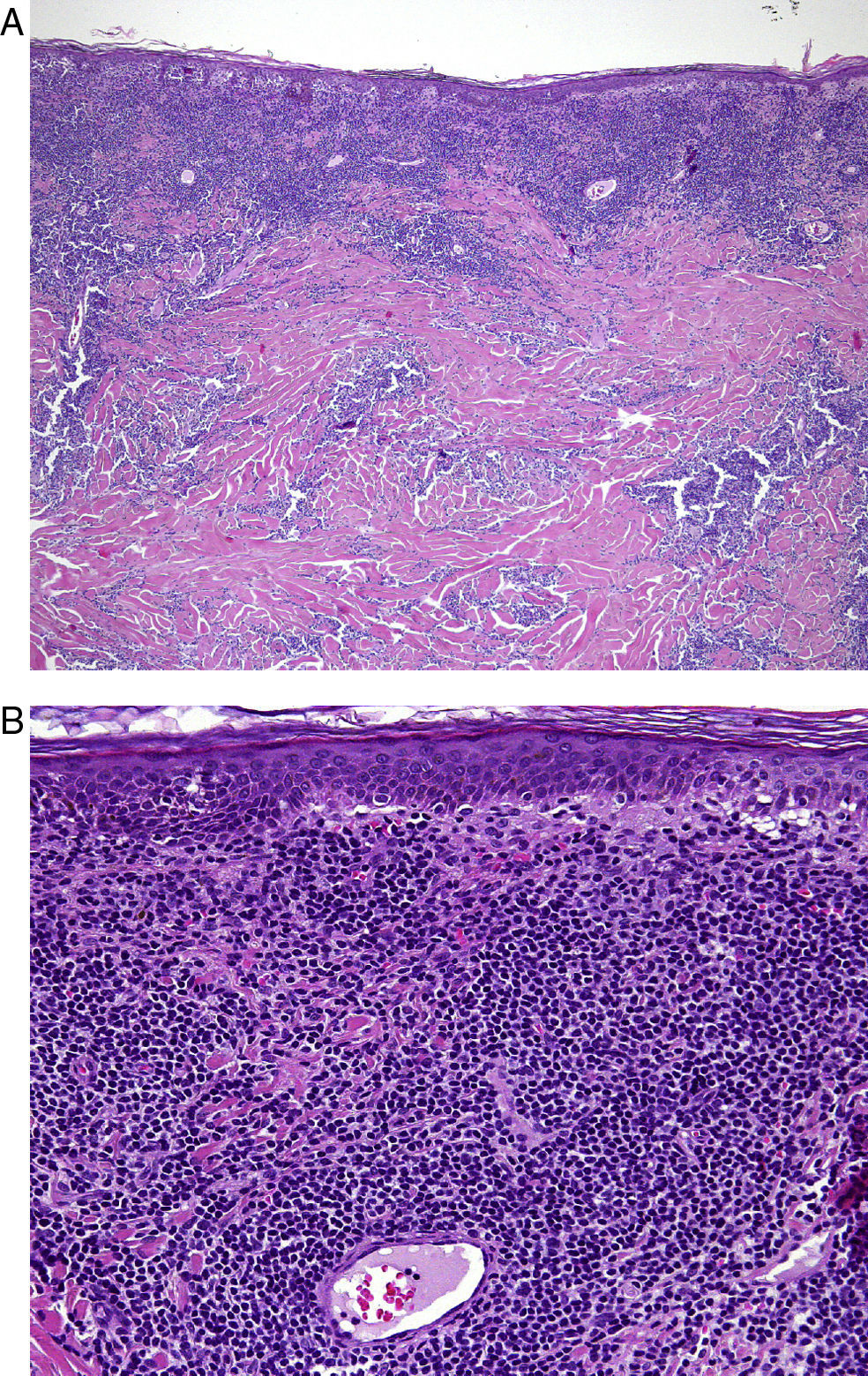
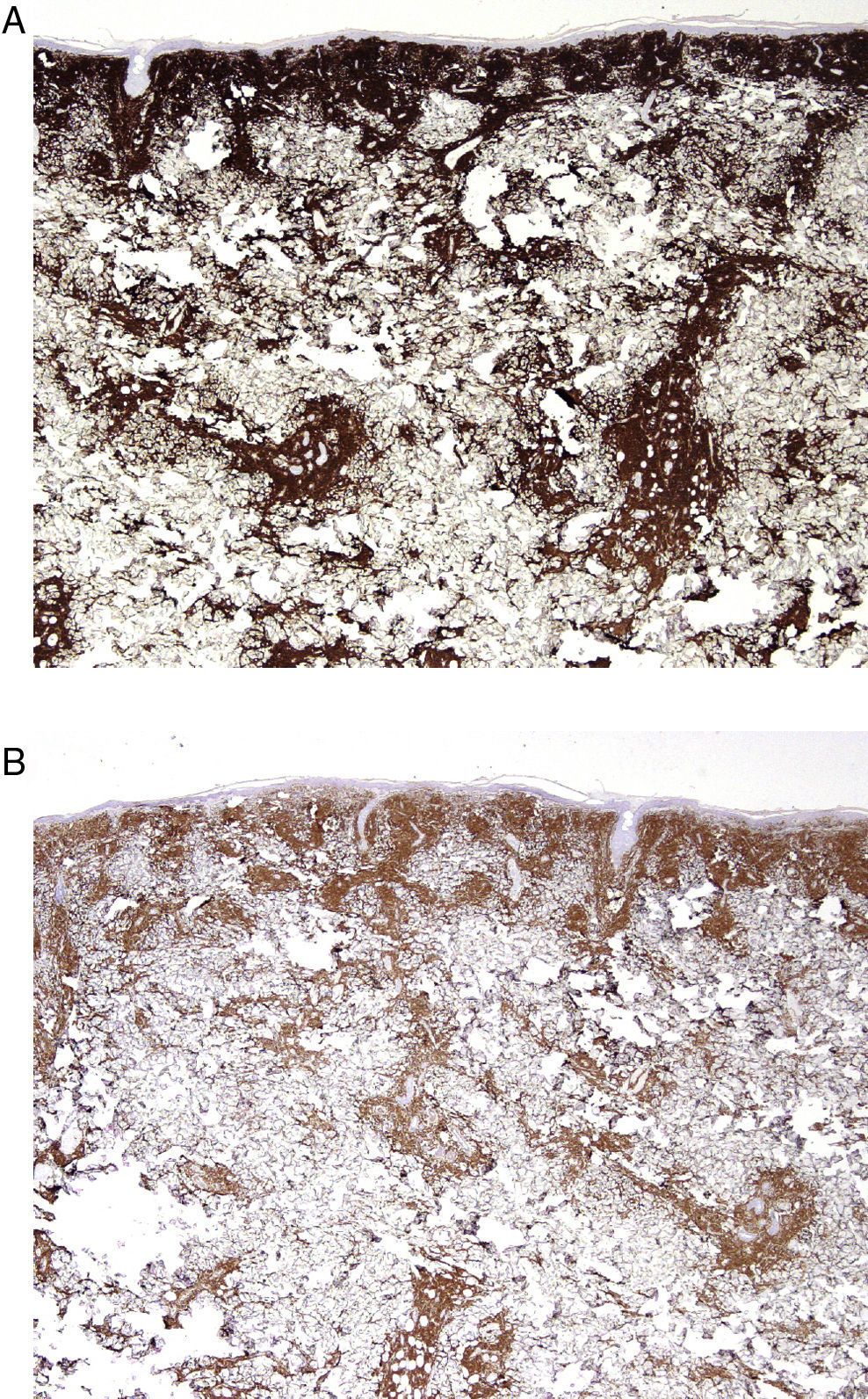
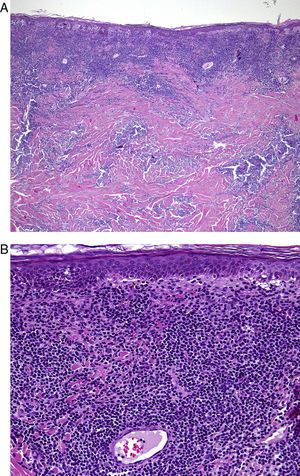
Case DescriptionA 68-year-old man with a history of hypertension and benign prostatic hyperplasia in treatment with doxazosin presented with erythematous-violaceous infiltrated plaques and nodules of 1-year duration. The lesions first appeared on the abdomen and then spread to the trunk and the roots of the limbs (Fig. 1). He had no fever or other symptoms, except noninflammatory arthralgia. Lymph nodes were not palpable in the physical examination. His blood counts showed cytopenia (leukocytes 2000, neutrophils 700, and platelets 88 000). With a suspected diagnosis of a lymphoproliferative process, a skin biopsy was taken. This showed epidermotropic infiltration of the papillary and deep dermis. Intermediate-size lymphocytes with a centroid or monocytoid appearance were present in perivascular and interstitial areas between collagen bundles and in the basal layer of the epidermis. Immunohistochemical staining was positive for CD20, CD79a, bcl2, and immunoglobulin (Ig) D, and negative for CD3, CD5, CD10, bcl6, CD23, cyclin D1, multiple myeloma oncogene 1, and myeloperoxidase (Fig. 2 and Fig. 3). With a provisional diagnosis of MZL, a staging study was performed. The same monoclonal rearrangement of the heavy chain Ig gene was detected in the bone marrow biopsy and peripheral blood analysis. A full biochemical analysis, protein analysis, and serology for Borrelia burgdorferi and for hepatitis virus B and C showed an increase in β2-microglobulin (4.02mg/L) and past hepatitis B infection (negative for hepatitis B surface antigen [HBsAg] and positive for anti-hepatitis B and anti-hepatitis B surface antibodies). The remaining parameters were normal or negative. Only mild superficial gastritis was detected in gastric endoscopy, and no Helicobacter pylori were isolated from the biopsy sample. The thoracoabdominal computed tomography showed massive splenomegalia. With a possible diagnosis of splenic MZL, splenectomy was performed. Almost all the lesions disappeared and bicytopenia resolved after 1 month (Fig. 4). Histologic study of the spleen showed a monomorphic micronodular proliferation with a immunophenotype similar to that of the cutaneous lesion except that IgD was negative. Study by fluorescence in situ hybridization for MALT1 translocation was negative and PCR of IgH showed monoclonality. These findings confirmed the diagnosis of splenic MZL. Four months later new lesions appeared and the patient received 6 cycles of chemotherapy in combination with rituximab (R-CHOP [rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone]) every 3 weeks. The lesions disappeared after this treatment. However, 2 months later, hepatitis developed due to reactivation of the hepatitis B virus and the patient died despite receiving treatment with lamivudine.
Approximately 25% of primary cutaneous lymphomas are B-cell lymphomas, but in light of the lack of agreement on the classification of cutaneous B-cell lymphomas, the true incidence of MZL is unknown.3,4 According to some authors, MZL is the most frequent type of cutaneous B-cell lymphomas whereas others consider it to be relatively uncommon. Given the differences in behavior and prognosis of different types of MZL, it is important to determine when skin involvement in MZL is primary or secondary. By definition, a lymphoma is considered as a primary cutaneous malignancy if, on diagnosis or during the staging study, no other organ is found to be involved. In our patient, multiorgan involvement (skin, peripheral blood, bone marrow, and spleen) of the MZL was demonstrated. These characteristics are consistent with splenic MZL, which has an indolent course and presents with splenomegalia (almost 100% of the time), along with bone marrow involvement (95%) and peripheral blood involvement (75%).5 At times, autoimmune diseases may be associated with splenic MZL and can be the chief complaint. They were not, however, reported in this patient at any time during the course of the disease. In our case, cells from all involved areas had the same morphology and the same phenotype, suggesting that they originated from the same clone. In addition, the clinical course, in which the skin lesions all but disappeared and blood counts returned to normal after splenectomy, is evidence in favor of diagnosis of splenic lymphoma with secondary skin involvement. Skin involvement in MZL is exceptional and has only be reported occasionally.6,7 Chiang et al.6 reported a patient with multiple papules on the trunk and thighs. Histology revealed MZL mimicking mycosis fungoides. The staging study in that case showed bone marrow involvement and splenomegalia, although histopathology of the spleen was not performed. The patient responded well to narrow-band UV-B phototherapy. In another study of a series of 85 cases of splenic MZL, Mollejo et al.7 singled out 4 cases with a diffuse pattern of infiltration. These lesions were negative for IgD and 2 of them were associated with epidermotropic skin involvement. The authors considered these lymphomas to be a variant of splenic MZL. They did not report the extent of skin involvement, so we do not know whether it was as severe as in our patient. Nevertheless, there are certain similarities with our case, such as intense involvement of the red pulp of the spleen, negative IgD status (splenic MZL usually expresses IgD), and epidermotropic skin involvement. Such epidermotropism is somewhat unusual and not reported in large series of primary cutaneous MZL,8,9 except for a study by Bathelier et al.,10 who reported epidermotropism in 8% of cases. Of the 49 cases of MZL included in that series, 29 were primary cutaneous forms and 20 had systemic involvement though none had involvement of the spleen. The clinical features are not described, and it is not specified whether the cases of epidermotropism corresponded to primary or secondary MZL. In addition to this study and those of Chiang et al.6 and Mollejo et al.7 (which refer to secondary skin involvement in splenic MZL), we could only find 1 other report of primary cutaneous MZL with epidermotropism.11
As is the case with cutaneous MZL, splenic MZL is usually indolent and a watchful waiting approach can be adopted. When treatment is indicated, splenectomy has usually been considered.5 However, new biologics such as rituximab (anti-CD20 monoclonal antibody) may also be administered although there is still some debate about its usefulness. Some authors are in favor of treatment with this drug, with or without associated chemotherapy, depending on the status of the patient.12 The use of rituximab is, however, not without its risks. One of these is reactivation of hepatitis B, which can be fatal, as was the case in our patient. This complication may occur during or after treatment. Cases have been reported up to 12 months after discontinuation.13 The first patient with this complication was reported in 1999, and new cases were subsequently reported, almost always when rituximab was administered in combination with chemotherapy although there have also been reports after monotherapy.14,15 This makes it necessary to screen for hepatotoxic viruses, not only when patients are treated with rituximab but also in the case of treatment with other biologics widely used at present in dermatology such as anti-tumor necrosis factor agents.16 In patients with prior hepatitis B infection (HBsAg-), viral DNA should be monitored to rule out reactivation. Prophylaxis should be given to patients positive for HBsAg as it has been found that no patients who received prophylactic treatment have died even in the presence of hepatitis B reactivation (compared to historical controls).15 Nevertheless, there is no consensus regarding the prophylactic agent of choice (lamivudine, entecavir, or tenofovir) or the duration of treatment, that is, whether it should be longer because of the possibility of late reactivation or shorter because of the development of resistance with prolonged treatment.
In summary, we present a rare case of MZL with skin involvement secondary to splenic MZL. Although histology does not generally allow differentiation between primary MZL and secondary MZL, we highlight that epidermotropism is common when cutaneous infiltration occurs in splenic MZL occurs but rare in primary cutaneous MZL. Finally, we would also like to emphasize the need to screen for the hepatitis virus before using immunosuppressive drugs.
Conflicts of InterestThe authors declare no conflicts of interest.
Please cite this article as: Gómez-de la Fuente E, et al. Linforma B esplénico de la zona marginal con afectación cutánea epidermotropa. Actas Dermosifiliogr.2012;103:427-31.