To analyze data corresponding to patients who underwent dermatological surgery in an operating room.
Material and methodsThis was a descriptive, retrospective study of operating room activities in the dermatology department of Hospital Universitario de Fuenlabrada in Madrid between January 2005 and December 2010. We analyzed the relative frequency of a range of patient and procedure-related variables, as well as substitution and cancellation rates, the proportional risk of complications, and operating room efficiency.
ResultsIn the period analyzed, 11 516 patients underwent surgery: 9351 required minor surgery, 1998 major ambulatory surgery, and 167 surgery requiring hospitalization. Simple excision was the most common procedure (64.7%), and in the majority of cases (85%), the condition was benign. The mean number of patients treated per day was 9.7, and mean operating room efficiency was 71.9%.
ConclusionsAccurate record-keeping is essential for analyzing operating room activities and comparing results with those from other centers. The analysis of patterns over time shows the effect of changes made on different indicators. In our case, a decrease in operating room efficiency was seen with an increase in the number of patients per day undergoing surgery.
Analizar los datos de pacientes sometidos a cirugía dermatológica en quirófano.
Material y métodoEstudio descriptivo, retrospectivo, de la actividad quirúrgica programada realizada en quirófano en el Servicio de Dermatología del Hospital Universitario de Fuenlabrada desde enero de 2005 a diciembre de 2010. Se analizan distintas variables relativas al paciente y a la cirugía. La medición de las variables se realiza mediante frecuencias relativas. Se estudian los índices de sustitución y de suspensión, el riesgo proporcional de complicaciones y el rendimiento quirúrgico.
ResultadosDurante el periodo de estudio fueron intervenidos 11.516 pacientes, 9.351 en la modalidad de cirugía menor, 1.998 mediante CMA y 167 precisaron cirugía con hospitalización. La patología tratada fue en su gran mayoría de naturaleza benigna (85%) y la escisión simple el procedimiento más realizado (64.7%). El número medio de pacientes/jornada fue de 9.7. El rendimiento quirúrgico medio fue del 71.9%.
ConclusionesEl registro adecuado es fundamental para conocer la actividad realizada y poder comparar con otros centros. El análisis evolutivo de los datos registrados permite observar el efecto que las medidas adoptadas tienen sobre los distintos indicadores. En nuestro caso el rendimiento del quirófano en porcentaje de ocupación disminuye al aumentar el número de pacientes intervenidos por jornada.
A large proportion of routine clinical practice in dermatology involves surgery. The incidences of both melanoma and nonmelanoma skin cancers have risen in recent decades and are expected to continue to do so in the coming years.1 Malignant and premalignant skin lesions are the third most frequent reason for consulting a dermatologist in Spain, and this type of consultation is expected to become even more common as the population ages. Skin cancer is usually treated surgically,2 as are many of the benign tumors we see routinely. The scope of dermatologic surgery, therefore, is considerable. Meanwhile, patients appreciate continuity of care, evaluating positively a process in which the dermatologist diagnoses a skin lesion, chooses and performs the procedure to treat it, and then follows the patient's progress afterwards.3
Although most dermatologic surgical procedures are carried out on an outpatient basis under local anesthesia, the services of an anesthesiologist are sometimes required because of patient characteristics or surgical complexity. In such cases the procedure may be scheduled as major ambulatory surgery (MAS) or the patient may have to be admitted to hospital for postoperative observation.
Adequate record-keeping on all surgical procedures is necessary if we are to understand our practice and manage human and material resources appropriately. The operating room occupancy rate (percentage of available time the space is occupied by patients) is the indicator usually used to reflect operational efficiency, as it allows a surgical department to plan the number of patients it can handle in a given period.4 This statistic is calculated on the basis of data collected, and serves only as a reflection of the time the space was in use, without distinguishing uses and without considering how long procedures should take in accordance with their complexity.
The aim of this study was to analyze data for patients undergoing dermatologic surgery in our operating rooms. By following several indexes over time, we will be better able to plan measures to improve efficiency and quality of care in dermatologic surgery.
Materials and MethodsThis was a descriptive, retrospective study of surgical procedures performed by dermatologists in operating rooms at Hospital Universitario de Fuenlabrada between January 2005 and December 2010. After a dermatologist had made a clinical diagnosis and prescribed surgical treatment, the patient was placed on a wait list. The procedure was then allocated a place in the operating room schedule. Cases were classified according to patient characteristics (age, concurrent diseases) and expected complexity of the procedure according to the Davis criteria (with large lesions, long duration of surgery, or need for sedation or general anesthesia indicating complexity). Grade 1 procedures (interventions under a local anesthetic and requiring no special postoperative care) were classified as minor surgery. Procedures classified as grades 2 and 3 were scheduled as MAS or surgery with planned admission. Grade 2 interventions were those performed under local, regional or general anesthesia or sedation, requiring specific but nonintensive postoperative care that was not of long duration; oral analgesics were available if needed. Grade 3 surgeries were those that required longer postoperative care in the hospital. According to hospital policy, patients under the age of 14 years undergoing any type of surgery were managed under the MAS regimen so that anesthesia could be adequately monitored. MAS procedures with complications that were followed by unplanned admission for postoperative observation were classified as surgery with hospitalization. Unscheduled emergency surgeries were also included.
Preanesthetic assessment, which was performed by anesthesiology department staff, included a preoperative blood work-up, electrocardiogram, chest radiograph, and other studies as required in relation to concomitant conditions. The anesthesiology department staff also prescribed the prophylactic antibiotic regimen and anticoagulant or antiplatelet therapy required according to hospital protocols. Patients were observed in the day hospital after minor surgery or in the postanesthesia recovery unit in all other cases, once again according to hospital protocol, for later discharge home or transfer to a ward. All MAS patients and hospitalized patients were checked 48hours and 7 days after surgery. Patients who underwent minor surgery were instructed to come to the outpatient clinic if they experienced a new symptom.
From digital records (compiled with the SELENE clinical history program), we collected clinical data, nursing protocols, pathology reports, and the minimum basic data set for each case. We analyzed both patient variables (age, sex, medical history, and dermatologic diagnosis) and surgical variables (procedure, surgical modality, anesthetic technique, and complications). The results are reported as relative frequencies. We calculated substitution rates (percentage of all departmental procedures accomplished as MAS), cancellation rates (percentage not performed on the day assigned), the relative risk of complications, and efficiency.
ResultsOf a total of 11 993 surgeries scheduled by the hospital's dermatology department, 11 516 were performed. Of these, 5213 (45.26%) were in men and 6303 (54.26%) in women.
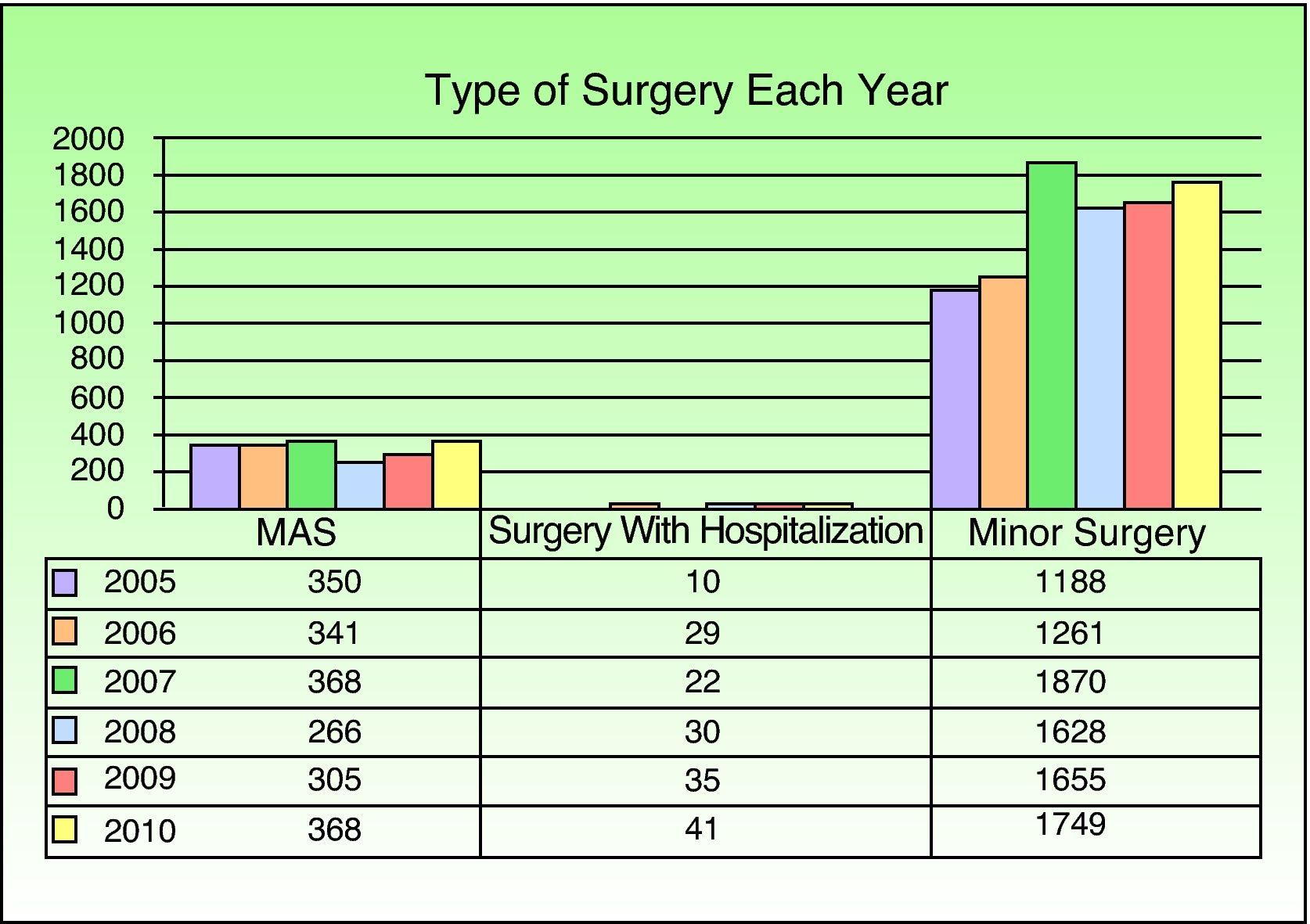
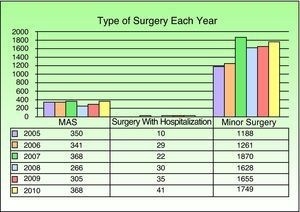
Minor procedures accounted for 81.2% of the total (9351/11 516), MAS for 17.34% (1998/11 516) (substitution rate), and surgery with hospitalization for 1.45% (167/11 516) (Fig. 1).
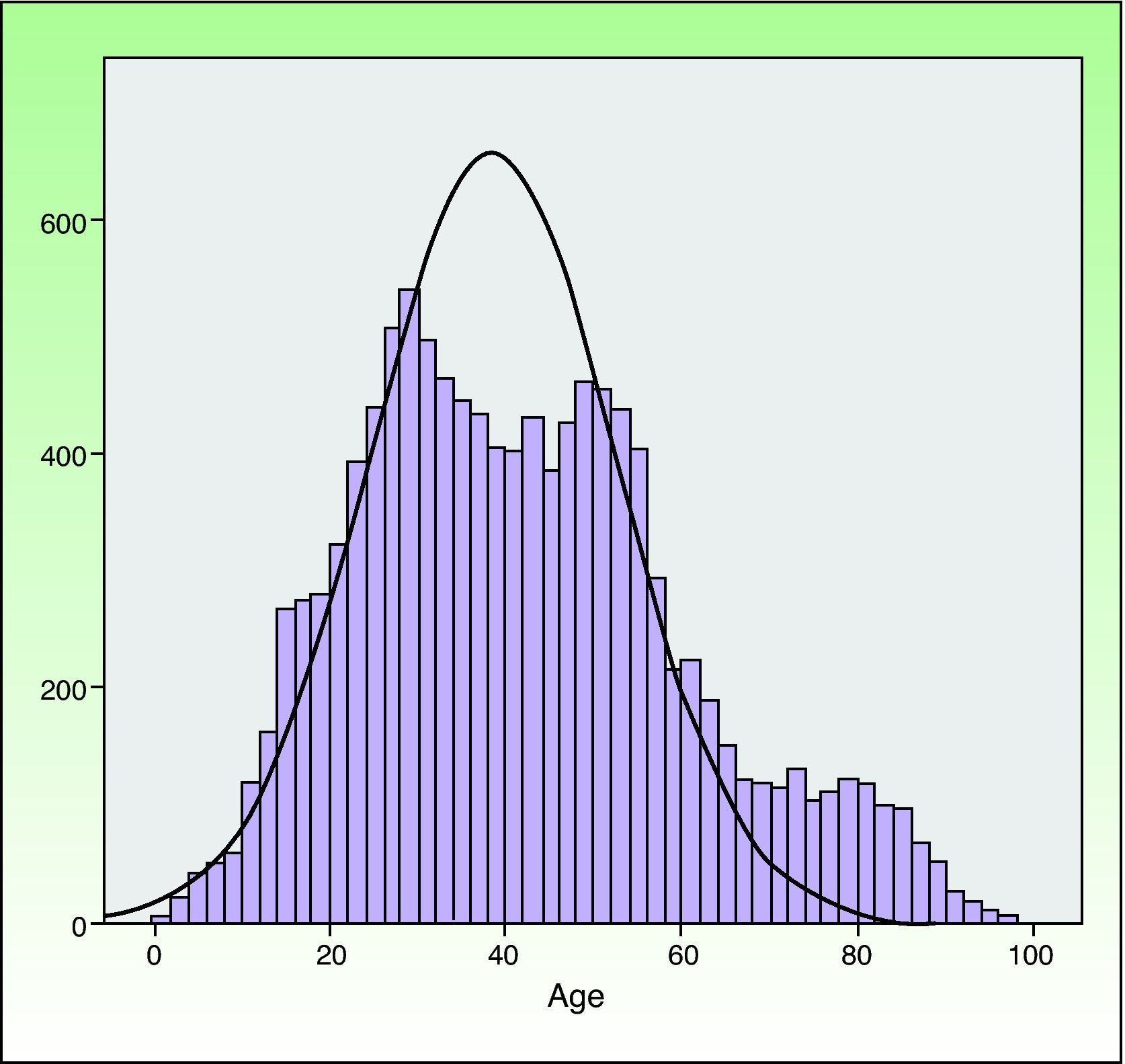
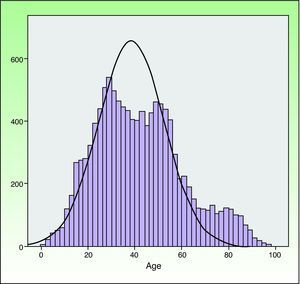
The mean (SD) age was 41.49 (18.66) years, and the age distribution (Fig. 2) was similar for men and women. The mean age of patients undergoing minor surgery was 38.60 (14.85) years, whereas patients managed under other regimens were older (MAS, 52.45 [26.64] years; with hospitalization, 72.53 [17.71] years).
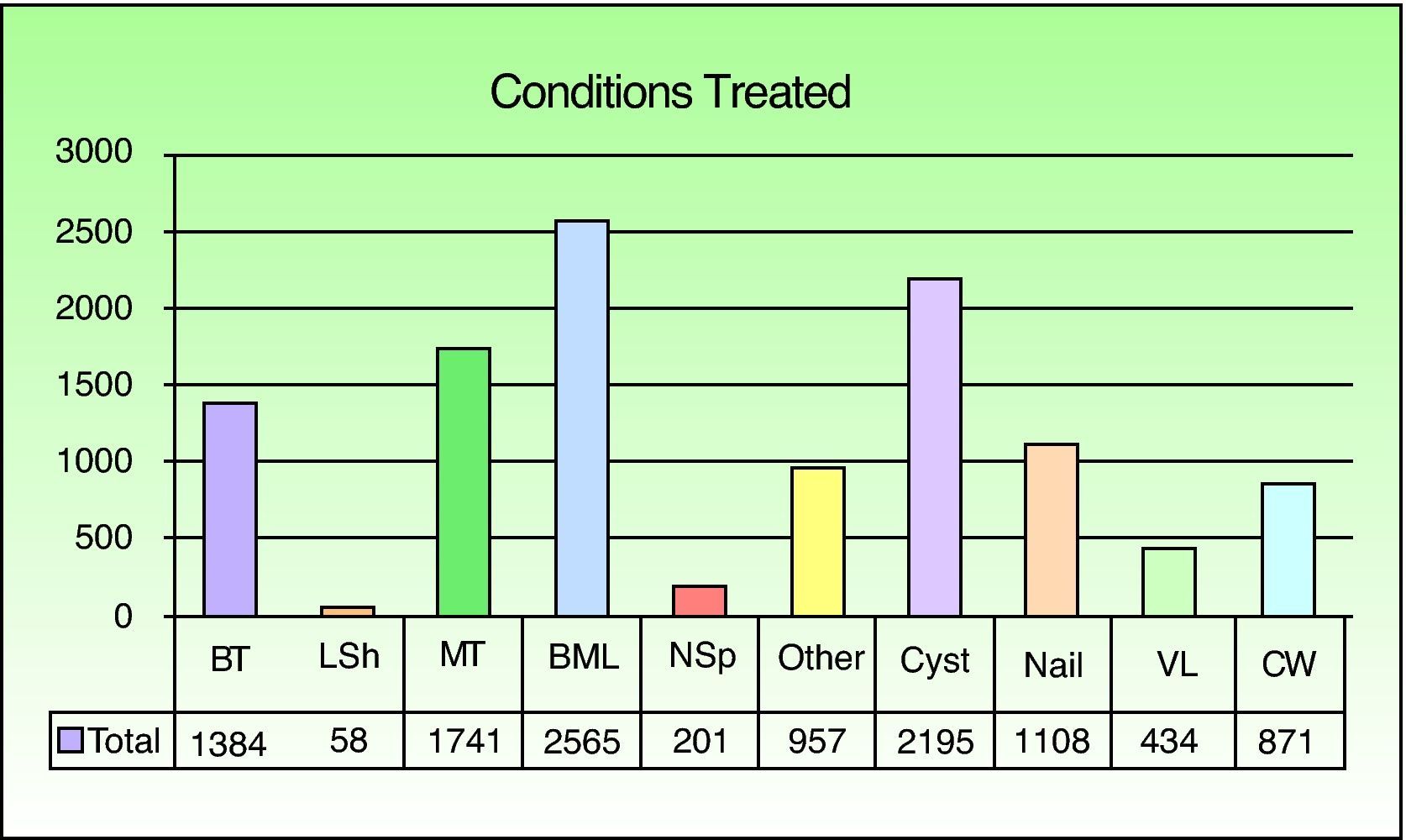
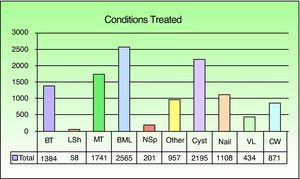
Overall, the most common excisions were of benign melanocytic lesions (22% of the interventions), followed by cystic lesions (19%), and malignant tumors (15%) (Fig. 3). Benign melanocytic lesions (25%) were also the most common type of minor surgery. Malignant tumors, however, accounted for the largest diagnostic category among MAS cases and hospitalized patients (52% and 71%, respectively).
The medical histories of 79% of the patients were unremarkable. The most common comorbidity was hypertension (in 15% of the patients). Among MAS patients, hypertension was found in 37%, heart disease in 12%, and diabetes mellitus in 12%, along with other associated conditions. Among hospitalized surgical patients, 40% had hypertension, 24% some form of heart disease, and 19% diabetes mellitus.
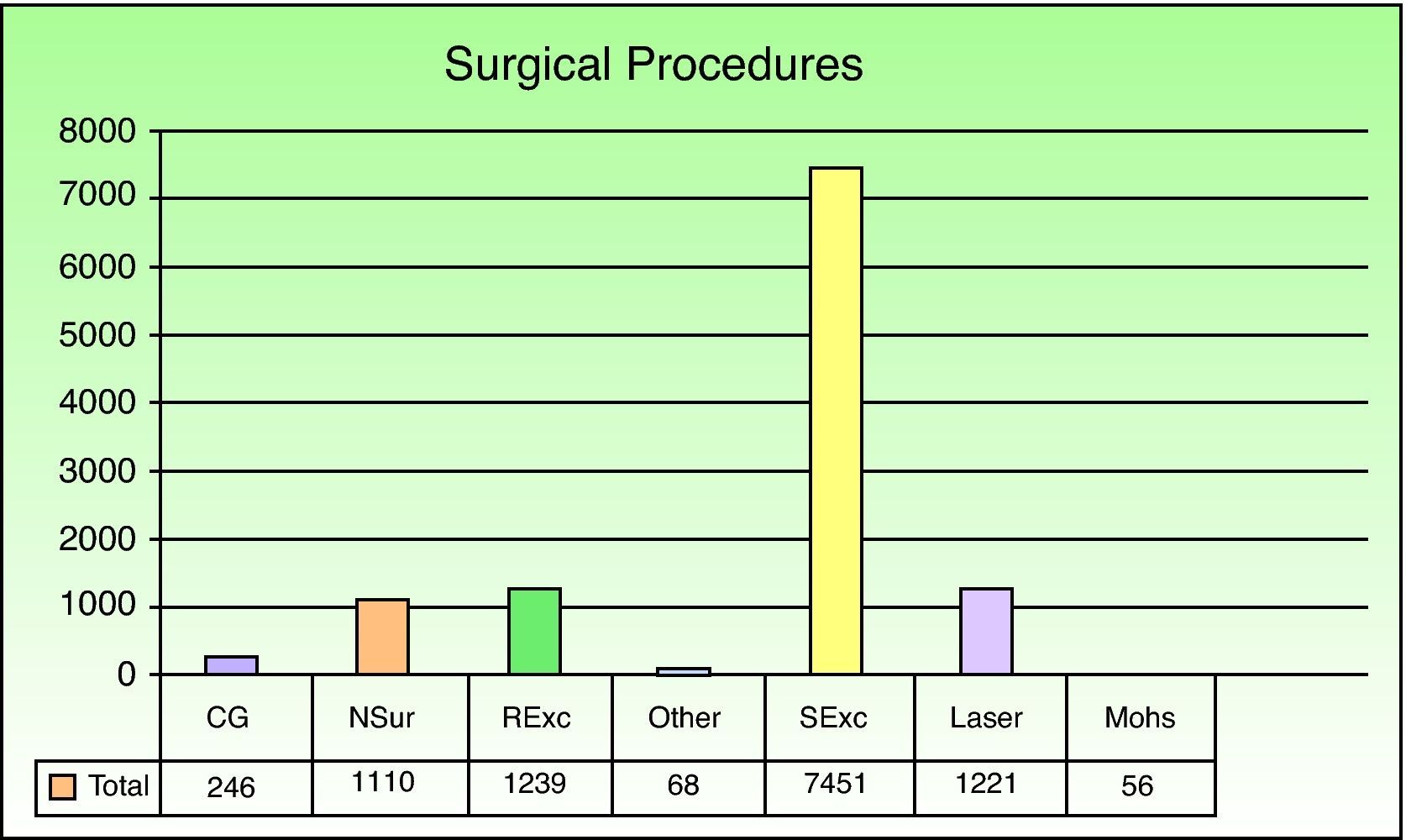
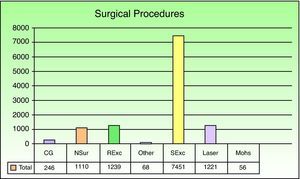
Simple excision of a skin lesion was the most frequently performed procedure overall (in 64.7% of the patients), followed by radical excision of malignant tumors with removal of affected margins (10.75%) (Fig. 4). Among patients undergoing minor surgery, simple excision of a lesion was again the most common procedure (68.93%) and pulsed dye laser therapy was the second most common (13%). The most common MAS procedures were simple excision of a skin lesion (48.24%) and radical tumor excision with removal of affected margins (28.97%). In hospitalized surgical patients, the order was reversed (tumor excision with removal of affected margins, 28.74%; simple excision, 24.55%). MAS procedures (20.95%) or surgeries with hospitalization (8.85%) were used when skin flaps and grafts were needed. Such procedures were the third most common in these 2 patient groups.
Most interventions (84%) were performed under local anesthesia administered by the dermatologist. In 7% of the interventions, an anesthesiologist was required to provide general anesthesia, epidural-spinal anesthesia, or sedation by means of various techniques. Thirty-two percent of the MAS patients and 57% of patients requiring admission received some form of care from an anesthesiologist.
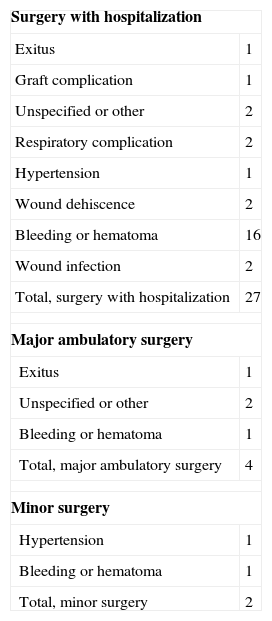
Thirty-three patients developed complications (Table 1). In most of these cases (27), the patient had been hospitalized after surgery (relative risk, 1:6). Complications developed in 4 MAS patients (relative risk, 1:499) and in 2 minor surgery patients (relative risk, 1:4675). Bleeding (16 patients) was the most common complication. Two patients died due to major cardiovascular complications during the period under study.
Perioperative Complications.
| Surgery with hospitalization | |
| Exitus | 1 |
| Graft complication | 1 |
| Unspecified or other | 2 |
| Respiratory complication | 2 |
| Hypertension | 1 |
| Wound dehiscence | 2 |
| Bleeding or hematoma | 16 |
| Wound infection | 2 |
| Total, surgery with hospitalization | 27 |
| Major ambulatory surgery | |
| Exitus | 1 |
| Unspecified or other | 2 |
| Bleeding or hematoma | 1 |
| Total, major ambulatory surgery | 4 |
| Minor surgery | |
| Hypertension | 1 |
| Bleeding or hematoma | 1 |
| Total, minor surgery | 2 |
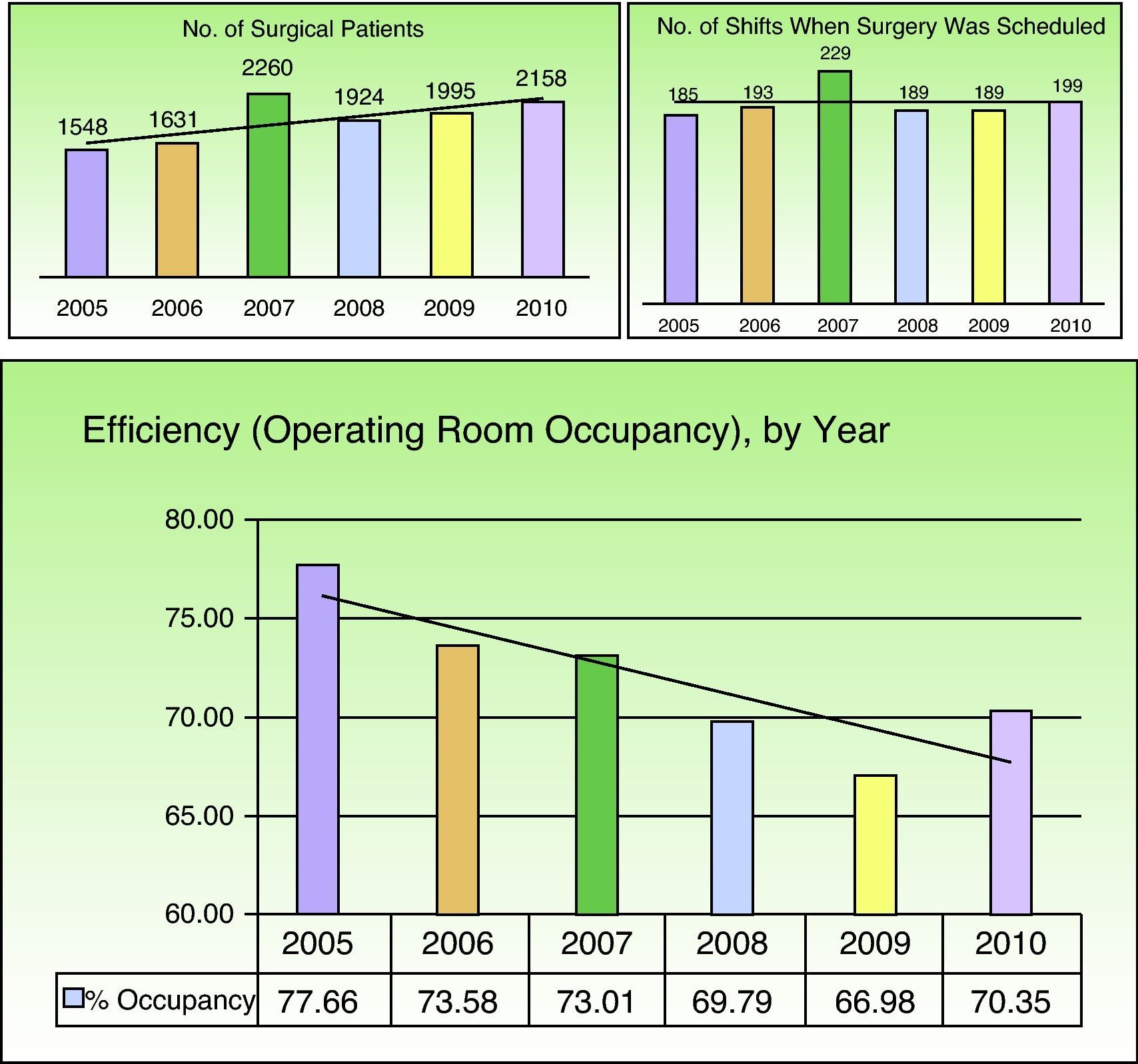
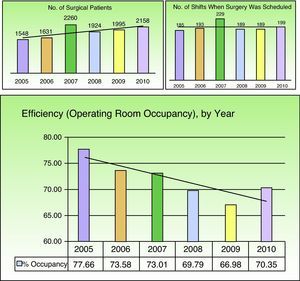
Scheduled procedures were performed on 11 481 patients (99.7%) during 1184 surgery shifts. The remaining 35 procedures were unscheduled emergencies. An average of 9.7 patients were treated per shift, with gradual increases from 8.34 patients per shift in 2005 to 10.73 patients per shift in 2010. The average efficiency during this period, expressed statistically as the operating room occupancy rate, was 71.9%. This statistic for efficiency tended to decrease over the study period and reached a low of 66.97% in 2009 (Fig. 5).
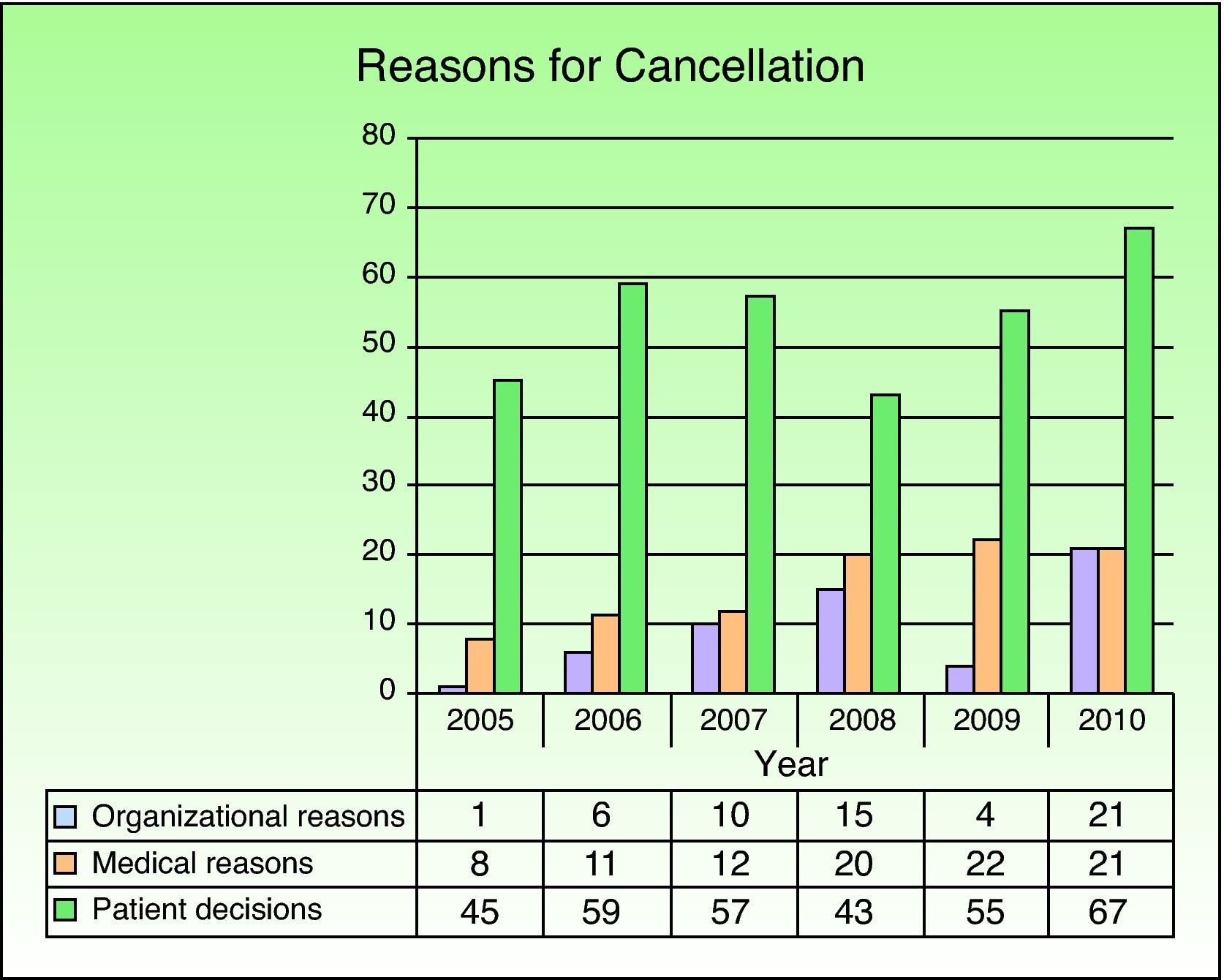
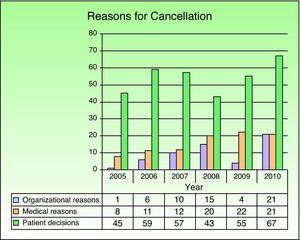
A total of 477 scheduled procedures were cancelled during the study period (overall cancellation rate, 4%). Of the cancelled procedures, 220 (46%) were in men and 257 (54%) in women. The mean age of these patients was 39.95 (18.79) years. The largest proportion of cancelled procedures (404 cases [85%]) would have been minor surgeries (cancellation rate, 4.3% in this category). Only 70 procedures (15%) would have been MAS cases (cancellation rate, 3.5% in this category) and only 3 would have been scheduled surgeries with hospitalization. Failure of the patient to come to the operating room was the reason for cancellation in 326 cases (68.3%) (Fig. 6).
DiscussionOperating room procedures accounted for a considerable proportion of our dermatology department's activity. Many of the dermatologic conditions that can be treated surgically are handled in minor procedures. MAS and surgery with planned hospitalization are safe, efficient alternatives when surgical technique or patient comorbidity call for these approaches. Performing more complex interventions under a MAS regimen reduces the likelihood of complications and the cost of hospitalization.5 The total number of patients undergoing surgery increased annually during the study period, mainly because the volume of minor surgeries increased. The more frequent scheduling of pulsed dye laser treatments in the operating room used for minor procedures from 2006 onward may have been one of the factors that led to a rise in the number of cases managed in this category.
Hospital Universitario de Fuenlabrada serves a predominantly young population. The population over the age of 65 years accounts for only about 6% of the total according to census records for the area. Age determines the type of dermatologic disease patients develop. Young patients have more benign conditions that can be resolved using less complex procedures, explaining the high percentage of minor surgeries in our caseload.
Patient age correlated with type of procedure in our study. Minor surgery patients were younger on average than patients undergoing surgery under other regimens. Older patients usually have more concomitant diseases and are being treated for more complex dermatologic conditions for which MAS or surgery followed by hospitalization would be indicated according to protocol.
We also observed relationships between surgical regimen and the most frequent diagnoses and types of procedure within the groups. Benign tumors subject to simple excision were the most common lesions treated under a minor-surgery regimen. Malignant tumors, which usually present in older patients and which require more complex surgical excision, were the most frequent diagnoses in patients undergoing MAS or surgery with hospitalization. Among admitted patients, the most frequently performed procedure was radical excision of a malignant tumor and affected margins. The construction of flaps or grafts and Mohs micrographic surgery were nearly always done under the MAS regimen or with hospitalization. In other published series, malignant tumors (basal cell and squamous cell carcinomas) have also been diagnosed more frequently in patients who require an anesthesiologist's care.6
The incidence of some type of perioperative complication in our hospitalized and MAS patients was 1.4%, a figure that was similar to or lower than reported elsewhere.5 Perioperative complications appear to be more directly related to type of surgical procedure than to patient characteristics. Such complications are estimated to occur in 3% of patients; the most frequent adverse events are graft failure, wound infection, and bleeding.7 Most adverse events were minor in our series. The most common one, bleeding, occurred in 0.8%. Exitus is very rare after MAS procedures, for which the associated mortality is lower than for conventional surgery with hospitalization.8 Cardiovascular events in patients of advanced age are the most frequent causes of death. The small size of our series prevents us from undertaking comparative analyses to draw conclusions about which patient characteristics, lesion locations, or procedures might increase risk of complications. Some minor complications in our patients who underwent minor surgery may have been treated in primary care settings and, therefore, may not have been recorded, possibly introducing bias. To attempt to guard against such bias, however, patients were instructed to come to our clinic if a new symptom appeared.
The average occupancy rates (the surgical efficiency measure) for dermatology departments have ranged from 70% to 85% in different published series.9 Operating room occupancy rates can be improved by beginning punctually at the start of each shift, reducing dead time between procedures, and increasing the number of patients scheduled during each shift.8
The number of patients scheduled for each shift increased gradually over the years we studied but the occupancy rate fell. Possible explanations are an increase in dead times between procedures or the inclusion of minor surgery occupancy rates in this study. The weight of minor surgery in our study was greater than in other series that only looked at patients undergoing MAS procedures.
The occupancy rate may not be the best indicator of efficiency in dermatology, given the importance of minor surgical procedures in this specialty. Other indicators, such as the operating room occupancy rate adjusted for standard operating times would probably be more appropriate for dermatology. Standard times are allocated according to International Classification of Disease codes (such as those of the 9th clinical modification, ICD-9-CM), with criteria defined by consensus among clinicians; standard associated dead times between procedures are added. Activity data should continue to be analyzed and different indicators compared to discover which ones faithfully reflect surgical efficiency in dermatology. The ideal indicator would take into consideration the times associated with each type of procedure, including adjustments for complexity, patient characteristics, and surgeon skill. In university hospitals, where residents participate and teaching occurs, the expected duration of procedures would be longer. An adjusted statistic would more accurately reflect the characteristics of dermatologic surgery and allow for comparisons that could identify the most efficient hospitals and even the most efficient surgeons.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Córdoba S, et al. Análisis de la actividad quirúrgica realizada en el Servicio de Dermatología del Hospital Universitario de Fuenlabrada (2005-2010). Actas Dermosifiliogr.2013;104:38-43.