Angiosarcoma is a malignant endothelial tumor that can form in any part of the body, including the skin. It is known as hemangiosarcoma or lymphangiosarcoma, depending on whether it derives from the endothelium of the blood vessels or the lymph vessels, respectively.1
It was first described in 1948 by Stewart and Treves2 in a series of 6 cases of lymphangiosarcoma after chronic postmastectomy lymphedema; since then, more than 400 cases have been reported of angiosarcoma associated with chronic lymphedema at different sites.
We report the case of a patient with angiosarcoma of the right arm, associated with chronic lymphedema due to non-Hodgkin lymphoma.
The only relevant history reported by the 84-year-old woman was a nodule in the lower right cervical region; results of a fine-needle aspiration biopsy of the nodule were negative for malignancy. Because of the growth of the nodule, a new fine-needle aspiration procedure was performed a year later and cytology results indicated suspected lymphoma; resection and biopsy were performed and a diagnosis of non-Hodgkin large B cell (CD20+) lymphoma was established.
Computed tomography (CT) revealed several bilateral enlarged axillary lymph nodes; the largest of these, measuring 2.5-3cm, was on the right side and in contact with the rib. The CT scan also revealed multiple enlarged hilar, mediastinal, para-aortic, and retroesophageal lymph nodes, and a 4.3-cm solid mass in the anterior segment of the right upper lobe of the lung.
An atypical segment resection of the right upper lobe and a mediastinal lymphadenectomy were performed, followed by adjuvant chemotherapy with cyclophosphamide, epirubicin, vincristine, and prednisone (6 cycles). Treatment response was complete, except in the right axilla, where the patient developed a palpable mass measuring 5 to 6cm that was fixed to the deeper layers; the mass was painful and produced a cutaneous reaction. The area was treated with external radiotherapy, with a fraction size of 1.8Gy to achieve a dose of 45Gy; the size of the mass decreased considerably in response to treatment.
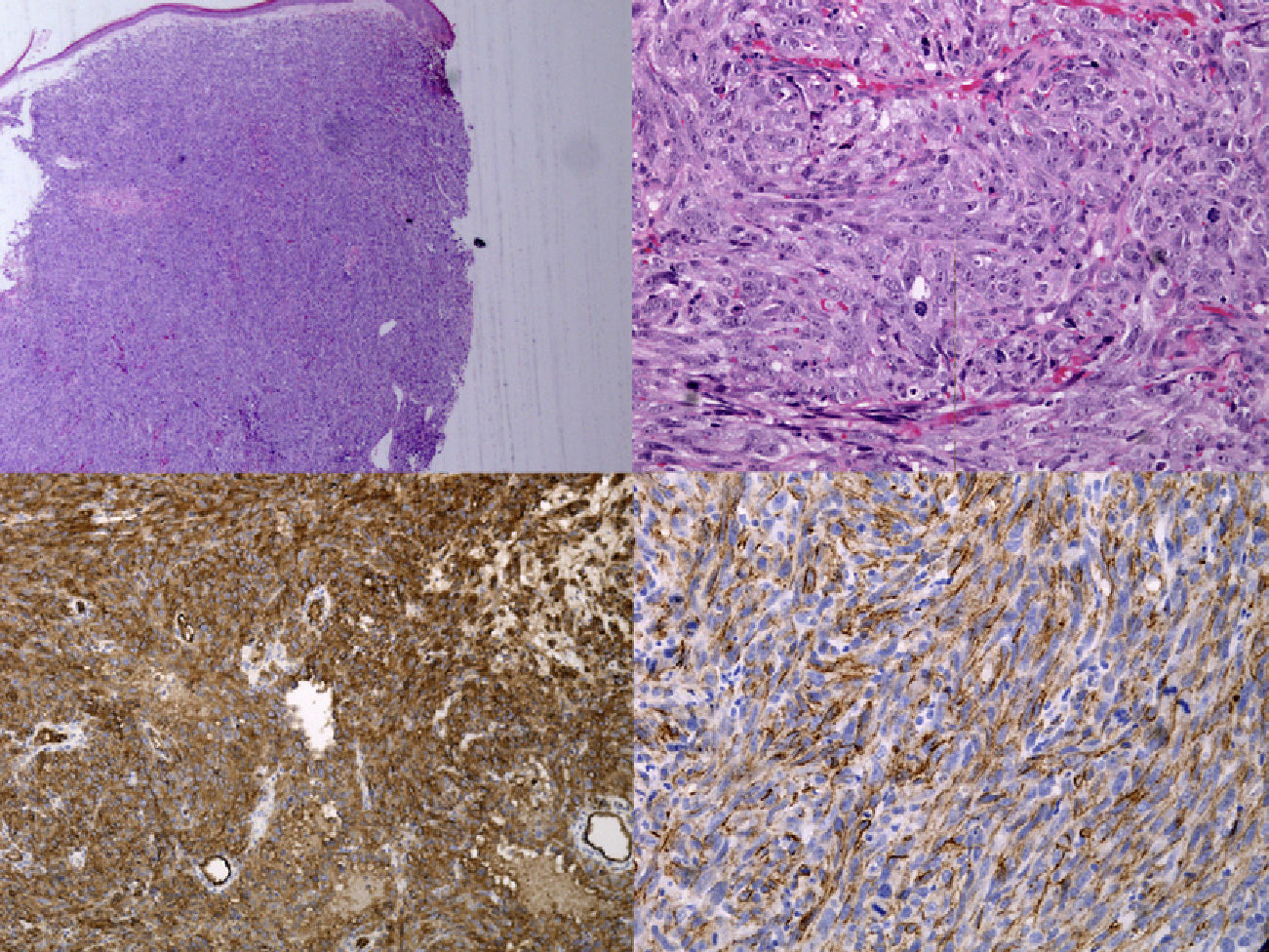
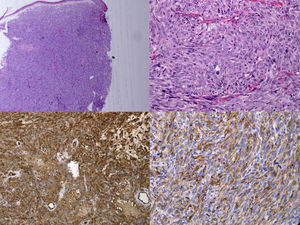
Nine years later, the woman was referred to our department with lesions on the anterior surface of the right arm, at the site of the chronic lymphedema; the lesions had appeared 2 weeks earlier and had begun as reddish-purple macules that transformed into plaques and, finally, gave rise to a tumor measuring 16×6cm. She also had erythematous-violaceous lesions measuring 1cm in diameter which had recently appeared on the outer quadrants of the right breast (Figs. 1 and 2). Histopathology of the lesion on the arm and those on the breast was compatible with lymphangiosarcoma and showed clefts between the collagen bundles, delineated by spindle-shaped endothelial cells and atypical hyperchromatic epithelial cells. Immunohistochemistry was positive for CD34, CD31, and factor VIII, thereby supporting the histologic diagnosis3 (Fig. 3). The staging study was negative.
After evaluation by the soft-tissue sarcoma multidisciplinary committee, it was decided to treat the patient with palliative chemotherapy.
Angiosarcoma that develops on a limb with chronic lymphedema or Stewart-Treves syndrome is a rare complication with a rapid and aggressive course.4 No cure exists to date and the disease is associated with poor prognosis and considerable morbidity. When the disease occurs in the context of a mastectomy, removal of the axillary lymph nodes and radiotherapy are thought to be predisposing factors.5 The course of the disease is usually aggressive, with rapid local or regional growth of lesions and a tendency toward early distant metastasis.6,7
Biopsy is essential for diagnosis and fine-needle aspiration is inadequate. Imaging studies, such as nuclear magnetic resonance imaging, are advisable in order to evaluate local spread.
It is essential to highlight the importance of regular clinical examinations of all patients with chronic lymphedema. While the lesion was first reported in lymphedema secondary to breast cancer, it may occur in any primary or secondary lymphedema. The limbs are the most commonly affected areas, but lymphangiosarcoma has even been reported after abdominoplasty in obese patients.8 Furthermore, according to published research, the mean time between development of lymphedema and diagnosis of angiosarcoma is between 8 and 10 years; it is thus important to carry out long-term follow-up of patients.4,6
When unusual lesions are found on a limb with lymphedema, histologic studies should be performed to detect this complication early on. Early diagnosis together with radical surgery and associated radiation therapy may increase the chance of survival in these patients. Amputation or wide local excision provides the best chance of long-term survival in patients with Stewart-Treves syndrome. Some ex vivo sensitivity studies have shown that chemotherapy appears to be an adequate complementary approach.9,10
Prevention of lymphedema of the limbs, when treatable secondary causes exist, should be considered essential and existing medical measures to achieve this goal should be optimized.
Please cite this article as: M.T. Sánchez-Medina, A. Acosta, J. Vilar, J. Fernández-Palacios. Angiosarcoma en linfedema crónico (síndrome de Stewart-Treves). Actas Dermosifiliogr. 2012;103:545-7.