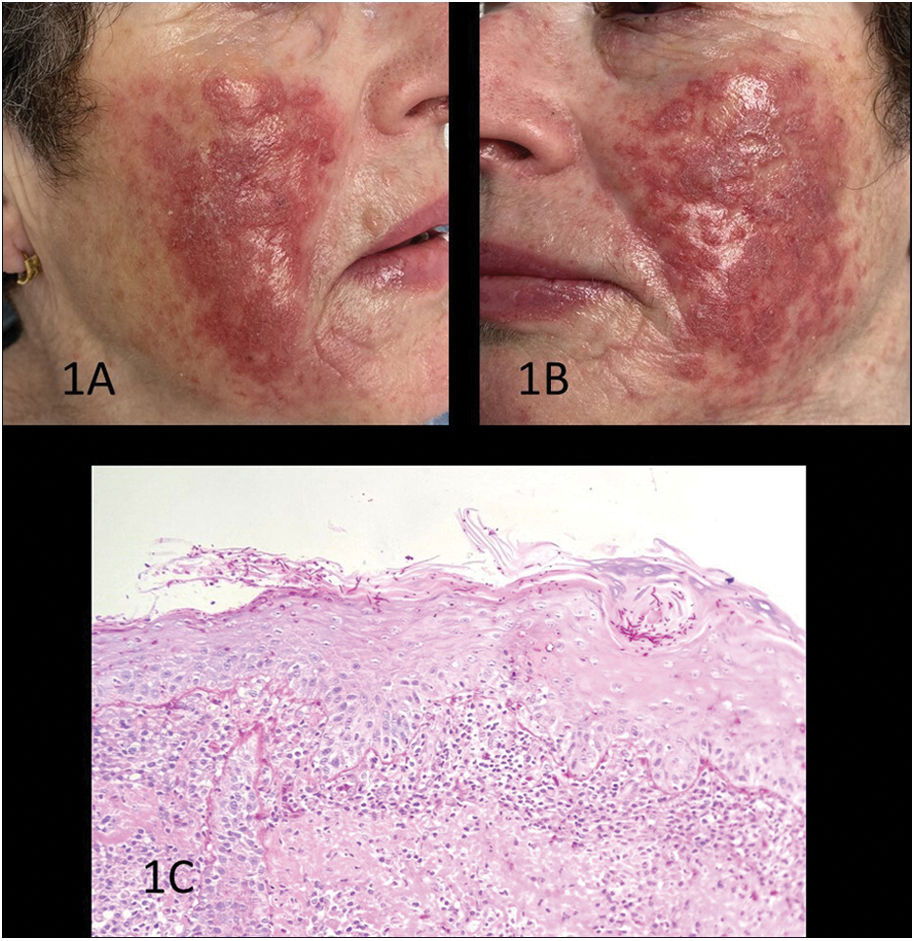
A 73-year-old woman with a past medical history of hypertension, dyslipidemia, and Meniere's syndrome, and currently on enalapril, zolpidem, betahistine, and simvastatin, presented with a 5-year history of erythematous pruritic plaques in the malar region, formed by the confluence of papules and a few random pustules (Fig. 1A, B).
A-B) Clinical images prior to diagnosis. Plaques formed by erythematous papules with slight superficial scaling, with some pustules over an erythematous base. C) Histological study using hematoxylin-eosin staining revealing an acanthotic epidermis with spongiosis, aggregates of intracorneal neutrophils, hyphae, and fungal spores in the stratum corneum positive to PAS staining, and a dense band-like lymphoplasmacytic infiltrate in the underlying dermis.
With a clinical diagnosis of rosacea, she had undergone multiple treatments, both topical (corticosteroids, metronidazole 1%, pimecrolimus) and systemic (isotretinoin 10mg/day, azithromycin 250mg/3 times a week, doxycycline 100mg/day, prednisone 20mg), yet her condition progressively worsened. Among the differential diagnoses suggested, allergic contact dermatitis, chilblain lupus, and acute cutaneous lupus were considered. Blood tests, including a complete blood count, general biochemistry, and autoimmune tests, showed no relevant findings. The histological analysis revealed an acanthotic epidermis with spongiosis, with aggregates of intracorneal neutrophils, hyphae, and fungal spores in the stratum corneum that tested positive to PAS staining, as well as a dense band-like lymphoplasmacytic infiltrate in the underlying dermis (Fig. 1C), findings consistent with the diagnosis of a facial tinea. Oral terbinafine was administered at 250mg/day, a topical solution was applied once daily, and a fungal culture was performed, which, after 1 month, tested positive for Trichophyton tonsurans. After 4 weeks into treatment, lesions improved significantly, leaving only slight residual hyperpigmentation.
Ethical considerationsThe patient has given explicit consent for the publication of the images and their use for scientific, educational, and scientific dissemination purposes.
Conflicts of interestNone declared.
We wish to thank Ricardo Ruiz Villaverde for his contribution to the publication of this case.